Podcast
Questions and Answers
Which muscles are involved in quiet breathing?
Which muscles are involved in quiet breathing?
- Sternocleidomastoid and scalene muscles
- Diaphragm and external intercostals (correct)
- Pectoralis major and latissimus dorsi
- Internal intercostals and abdominal muscles
How does the diaphragm move during contraction?
How does the diaphragm move during contraction?
- It does not move during contraction
- Its central portion flattens and moves superiorly
- Its central portion flattens and moves inferiorly (correct)
- It becomes more dome-shaped
What is the function of the external intercostal muscles during contraction?
What is the function of the external intercostal muscles during contraction?
- They elevate the ribs (correct)
- They depress the ribs
- They have no effect on the ribs
- They rotate the ribs
Which of the following are muscles of forced inspiration?
Which of the following are muscles of forced inspiration?
What happens when the muscles of quiet breathing relax?
What happens when the muscles of quiet breathing relax?
Which muscles are involved in forced expiration?
Which muscles are involved in forced expiration?
What is the primary stimulus for breathing in certain respiratory disorders like emphysema?
What is the primary stimulus for breathing in certain respiratory disorders like emphysema?
What happens when oxygen is administered to a person experiencing the hypoxic drive?
What happens when oxygen is administered to a person experiencing the hypoxic drive?
What happens to the chemoreceptors' sensitivity to Pco2 in the hypoxic drive?
What happens to the chemoreceptors' sensitivity to Pco2 in the hypoxic drive?
Which receptors, when stimulated by body movement, increase the depth of breathing?
Which receptors, when stimulated by body movement, increase the depth of breathing?
What is the function of the Hering-Breuer reflex?
What is the function of the Hering-Breuer reflex?
Which receptors are stimulated by stretch within the lungs and bronchioles?
Which receptors are stimulated by stretch within the lungs and bronchioles?
What are the muscles responsible for forced inspiration and expiration collectively referred to as?
What are the muscles responsible for forced inspiration and expiration collectively referred to as?
In which dimensions does the thoracic cavity change volume during breathing?
In which dimensions does the thoracic cavity change volume during breathing?
Which movement causes an increase in the vertical dimension of the thoracic cavity during inspiration?
Which movement causes an increase in the vertical dimension of the thoracic cavity during inspiration?
What causes the vertical dimensions of the thoracic cavity to decrease during expiration?
What causes the vertical dimensions of the thoracic cavity to decrease during expiration?
During quiet breathing, how much do the vertical dimensions of the thoracic cavity typically change?
During quiet breathing, how much do the vertical dimensions of the thoracic cavity typically change?
What causes greater changes in the superior movement of the diaphragm during forced expiration?
What causes greater changes in the superior movement of the diaphragm during forced expiration?
Why are some balloons easier to inflate compared to others?
Why are some balloons easier to inflate compared to others?
What primarily influences the amount of surface tension in the alveoli?
What primarily influences the amount of surface tension in the alveoli?
In which condition do premature infants face collapsing alveoli with each expiration?
In which condition do premature infants face collapsing alveoli with each expiration?
What happens to resistance in the airways if compliance decreases?
What happens to resistance in the airways if compliance decreases?
Which factor causes high surface tension within the alveoli?
Which factor causes high surface tension within the alveoli?
How does resistance to airflow change with bronchiole constriction?
How does resistance to airflow change with bronchiole constriction?
What is the primary function of the baroreceptors when they are overstretched?
What is the primary function of the baroreceptors when they are overstretched?
What is the role of the medulla oblongata in the sneezing and coughing reflexes?
What is the role of the medulla oblongata in the sneezing and coughing reflexes?
How do higher brain centers, such as the hypothalamus, limbic system, and cerebral cortex, influence breathing rate?
How do higher brain centers, such as the hypothalamus, limbic system, and cerebral cortex, influence breathing rate?
What is the purpose of the explosive blast of exhaled air generated by the sneezing and coughing reflexes?
What is the purpose of the explosive blast of exhaled air generated by the sneezing and coughing reflexes?
What is the primary role of the baroreceptors in infants?
What is the primary role of the baroreceptors in infants?
What factor influences airflow by establishing air pressure gradients in the respiratory system?
What factor influences airflow by establishing air pressure gradients in the respiratory system?
Which factor directly affects the resistance to airflow in the respiratory system?
Which factor directly affects the resistance to airflow in the respiratory system?
In the cardiovascular system, what is responsible for driving blood through the blood vessels?
In the cardiovascular system, what is responsible for driving blood through the blood vessels?
What opposes the airflow in the respiratory system due to factors like compliance and surface tension?
What opposes the airflow in the respiratory system due to factors like compliance and surface tension?
Which system experiences resistance within blood vessels similar to how air experiences resistance in the respiratory tract?
Which system experiences resistance within blood vessels similar to how air experiences resistance in the respiratory tract?
What causes an increase in airflow in the respiratory system?
What causes an increase in airflow in the respiratory system?
According to the passage, which of the following is the best analogy for the relationship between the medullary respiratory center and the pontine respiratory center?
According to the passage, which of the following is the best analogy for the relationship between the medullary respiratory center and the pontine respiratory center?
If a spinal cord injury occurs at C2 or above, what would be the predicted consequence to breathing?
If a spinal cord injury occurs at C2 or above, what would be the predicted consequence to breathing?
If a spinal cord injury occurs between C6 and T11, what would be the predicted consequence to breathing?
If a spinal cord injury occurs between C6 and T11, what would be the predicted consequence to breathing?
Which of the following receptors is NOT mentioned in the passage as being able to alter breathing rate and depth through reflexes?
Which of the following receptors is NOT mentioned in the passage as being able to alter breathing rate and depth through reflexes?
According to the passage, what is the primary function of the Hering-Breuer reflex?
According to the passage, what is the primary function of the Hering-Breuer reflex?
What is the primary stimulus for breathing in certain respiratory disorders like emphysema?
What is the primary stimulus for breathing in certain respiratory disorders like emphysema?
What is the main difference between minute ventilation and alveolar ventilation?
What is the main difference between minute ventilation and alveolar ventilation?
What is the relationship between anatomic dead space and physiologic dead space?
What is the relationship between anatomic dead space and physiologic dead space?
If the resistance to airflow increases, what change in breathing must occur to maintain adequate alveolar ventilation?
If the resistance to airflow increases, what change in breathing must occur to maintain adequate alveolar ventilation?
What is the approximate volume of anatomic dead space in a person weighing 150 pounds?
What is the approximate volume of anatomic dead space in a person weighing 150 pounds?
If a person's minute ventilation is 6000 mL and their anatomic dead space is 150 mL, what is their alveolar ventilation?
If a person's minute ventilation is 6000 mL and their anatomic dead space is 150 mL, what is their alveolar ventilation?
What is the normal tidal volume and respiratory rate for an adult, according to the text?
What is the normal tidal volume and respiratory rate for an adult, according to the text?
What is the primary function of the forced expiratory volume in 1 second (FEV1) test?
What is the primary function of the forced expiratory volume in 1 second (FEV1) test?
What is the typical range for the forced expiratory volume in 1 second (FEV1) in a healthy individual?
What is the typical range for the forced expiratory volume in 1 second (FEV1) in a healthy individual?
What is the maximum voluntary ventilation (MVV) test used to measure?
What is the maximum voluntary ventilation (MVV) test used to measure?
What is a typical value for maximum voluntary ventilation (MVV) in healthy individuals?
What is a typical value for maximum voluntary ventilation (MVV) in healthy individuals?
Which statement about individuals with respiratory disorders is true, according to the text?
Which statement about individuals with respiratory disorders is true, according to the text?
What is the primary purpose of pulmonary function tests like FEV1 and MVV?
What is the primary purpose of pulmonary function tests like FEV1 and MVV?
What is the inspiratory capacity (IC) composed of?
What is the inspiratory capacity (IC) composed of?
Which respiratory capacity includes the residual volume?
Which respiratory capacity includes the residual volume?
What does forced expiratory volume (FEV) measure?
What does forced expiratory volume (FEV) measure?
Which of the following is true about functional residual capacity (FRC)?
Which of the following is true about functional residual capacity (FRC)?
What is the primary significance of vital capacity (VC)?
What is the primary significance of vital capacity (VC)?
What does total lung capacity (TLC) represent?
What does total lung capacity (TLC) represent?
Flashcards are hidden until you start studying
Study Notes
Respiratory System
- Hypoxic Drive: In certain respiratory disorders, such as emphysema, the decreased ability to expire carbon dioxide leads to decreased blood Po2 levels, which becomes the stimulus for breathing.
- Chemoreceptors: Decreased Po2 levels stimulate chemoreceptors, which are less sensitive to Pco2 levels. Administering oxygen would elevate Po2 levels and interfere with a person's ability to breathe on their own.
Altering Breathing Patterns
- Proprioceptors: Stimulated by body movement, proprioceptors increase nerve signals to the respiratory center, leading to an increase in breathing depth.
- Baroreceptors: Stimulated by stretch, baroreceptors initiate a reflex to prevent overstretching of the lungs by inhibiting inspiration activities, known as the Hering-Breuer reflex.
- Irritant Receptors: Stimulated by irritants, irritant receptors initiate a sneezing or coughing reflex to remove the irritant.
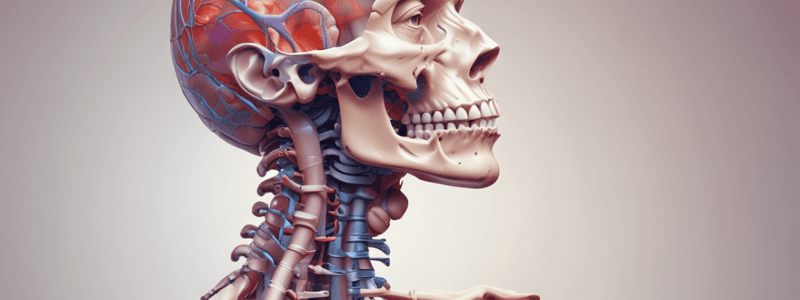
Mechanics of Breathing
- Skeletal Muscles of Breathing: The diaphragm and external intercostals are involved in quiet breathing, while the muscles of forced inspiration and forced expiration are classified as accessory muscles of breathing.
- Volume Changes: Contraction of breathing muscles causes thoracic cavity volume changes in three dimensions: vertically, laterally, and in an anterior-posterior direction.
- Pressure Changes: Pressure changes result from volume changes, based on Boyle's gas law.
Minute Ventilation and Alveolar Ventilation
- Minute Ventilation: The volume of air taken in during 1 minute, calculated by multiplying the tidal volume by the number of breaths per minute.
- Alveolar Ventilation: The amount of air that reaches the alveoli and is available for gas exchange per minute.
- Anatomic Dead Space: The collective space in the conducting zone where there is no exchange of respiratory gases, with an average volume of approximately 150 mL.
Reflexes and Higher Brain Centers
- Reflexes: Reflexes can alter breathing rate and depth, primarily initiated by chemoreceptors, but also by proprioceptors, baroreceptors, and irritant receptors.
- Higher Brain Centers: The hypothalamus, limbic system, and cerebral cortex can influence breathing rate in response to various factors, such as temperature, emotions, and emotional memories.
Airflow and Resistance
- Airflow: Directly related to the pressure gradient and inversely related to resistance.
- Pressure Gradient: Established by the skeletal muscles of breathing, with a steeper gradient resulting in greater airflow.
- Resistance: Opposes airflow, influenced by bronchiole diameter, compliance, and surface tension within the alveoli.
Pulmonary Function Tests
- Forced Expiratory Volume (FEV): The percentage of the vital capacity that can be forcefully expelled in a specific period of time, such as FEV1, which is the vital capacity percentage that is expired in 1 second.
- Maximum Voluntary Ventilation (MVV): The greatest amount of air that can be taken into and then expelled from the lungs in 1 minute.
- Respiratory Capacities: Calculated from the summation of two or more respiratory volumes, including inspiratory capacity, functional residual capacity, vital capacity, and total lung capacity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.