Podcast
Questions and Answers
What is the primary role of pleural fluid?
What is the primary role of pleural fluid?
- To assist in gas exchange
- To facilitate nutrient absorption
- To reduce friction and adhere the lungs to the thoracic wall (correct)
- To store air for the lungs
Which lung is shorter and wider?
Which lung is shorter and wider?
- Left lung
- Neither lung is shorter nor wider
- Right lung (correct)
- Both lungs are equal in size
How many lobes does the left lung have?
How many lobes does the left lung have?
- Three
- Four
- Two (correct)
- One
What is a bronchopulmonary segment?
What is a bronchopulmonary segment?
What role does the pulmonary artery play in the lungs?
What role does the pulmonary artery play in the lungs?
Which system is responsible for bronchodilation?
Which system is responsible for bronchodilation?
What separates the lobules in the lungs?
What separates the lobules in the lungs?
Where does gas exchange primarily occur in the lungs?
Where does gas exchange primarily occur in the lungs?
What is the purpose of the cardiac notch?
What is the purpose of the cardiac notch?
What is the shape of the diaphragm?
What is the shape of the diaphragm?
What is one of the primary functions of the respiratory system?
What is one of the primary functions of the respiratory system?
Which of the following structures is part of the conducting zone?
Which of the following structures is part of the conducting zone?
Which muscles are included in the chest wall of the respiratory system?
Which muscles are included in the chest wall of the respiratory system?
What role does the epithelium of the nasal passages play?
What role does the epithelium of the nasal passages play?
In which area of the respiratory system does gas exchange occur?
In which area of the respiratory system does gas exchange occur?
What function does the respiratory system serve during childbirth?
What function does the respiratory system serve during childbirth?
Which of the following is NOT a function of the conducting zone?
Which of the following is NOT a function of the conducting zone?
What is a non-vital function of the respiratory system?
What is a non-vital function of the respiratory system?
What are the two major functions of the pleurae?
What are the two major functions of the pleurae?
Which pressure is typically negative relative to intra-alveolar pressure?
Which pressure is typically negative relative to intra-alveolar pressure?
What is the term for the pressure difference between intrapleural and intra-alveolar pressures?
What is the term for the pressure difference between intrapleural and intra-alveolar pressures?
What role does pleural fluid play during breathing?
What role does pleural fluid play during breathing?
Which law explains the relationship between volume and pressure in gases?
Which law explains the relationship between volume and pressure in gases?
What is the primary mechanism driving pulmonary ventilation?
What is the primary mechanism driving pulmonary ventilation?
Where do sensory nerve fibers that contribute to lung function primarily arise from?
Where do sensory nerve fibers that contribute to lung function primarily arise from?
What is the function of the visceral pleura?
What is the function of the visceral pleura?
Which statement about pulmonary ventilation is true?
Which statement about pulmonary ventilation is true?
Which layer of the pleura is attached to the thoracic wall?
Which layer of the pleura is attached to the thoracic wall?
What happens to gas pressure when the volume of the container is increased?
What happens to gas pressure when the volume of the container is increased?
What is the relationship described by Boyle's law between pressure (P) and volume (V)?
What is the relationship described by Boyle's law between pressure (P) and volume (V)?
How does intra-alveolar pressure compare to atmospheric pressure during normal breathing?
How does intra-alveolar pressure compare to atmospheric pressure during normal breathing?
What kind of pressure is intrapleural pressure typically considered?
What kind of pressure is intrapleural pressure typically considered?
What primarily contributes to the negative intrapleural pressure within the thorax?
What primarily contributes to the negative intrapleural pressure within the thorax?
During which phase of the breathing cycle is intrapleural pressure expected to be approximately –4 mmHg?
During which phase of the breathing cycle is intrapleural pressure expected to be approximately –4 mmHg?
What must be closely monitored to maintain proper intrapleural pressure?
What must be closely monitored to maintain proper intrapleural pressure?
What is the formula for calculating the relationship between initial and final pressure and volume in Boyle's law?
What is the formula for calculating the relationship between initial and final pressure and volume in Boyle's law?
What occurs when gas moves from an area of lower volume to higher volume?
What occurs when gas moves from an area of lower volume to higher volume?
What effect does increasing the number of gas molecules have on pressure in a constant volume container?
What effect does increasing the number of gas molecules have on pressure in a constant volume container?
What causes air to flow into the lungs during inspiration?
What causes air to flow into the lungs during inspiration?
What role does pulmonary surfactant play in the alveoli?
What role does pulmonary surfactant play in the alveoli?
How does the size of the airway affect gas flow?
How does the size of the airway affect gas flow?
What is the primary factor affecting the ability to ventilate the lungs?
What is the primary factor affecting the ability to ventilate the lungs?
What happens to intra-alveolar pressure during expiration?
What happens to intra-alveolar pressure during expiration?
What is the consequence of low thoracic wall compliance?
What is the consequence of low thoracic wall compliance?
Which statement accurately describes the movement of air during breathing?
Which statement accurately describes the movement of air during breathing?
During which phase of breathing is the thoracic wall compressed?
During which phase of breathing is the thoracic wall compressed?
What does the formula F = ∆P / R represent?
What does the formula F = ∆P / R represent?
Which factor does NOT directly influence pulmonary ventilation?
Which factor does NOT directly influence pulmonary ventilation?
Flashcards are hidden until you start studying
Study Notes
Introduction
- Respiratory system includes the lungs, airways, CNS control mechanisms, and chest wall.
- Chest wall consists of respiratory muscles - diaphragm, intercostals and abdominal muscles - and the rib cage.
Functions
- Supplies O2 to cells and removes CO2 produced by metabolism.
- Serves non-vital functions: odor sensing, speech production, straining.
Respiratory System Areas
- Conducting zone: passageways for air: nasal cavity, pharynx, trachea, bronchi, bronchioles. Structures not directly involved in gas exchange.
- Respiratory zone: structures involved in gas exchange: respiratory bronchioles and alveoli.
Conducting Zone Functions
- Provides passage for air.
- Removes debris and pathogens from incoming air.
- Warms and humidifies incoming air.
- Epithelium in nasal passages for odor sensing.
- Mesothelial cells of the pleura create pleural fluid.
- Pleural fluid serves as lubricant and adhesive for lung-chest wall movement.
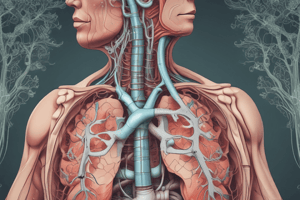
Lung Anatomy
- Lungs: pyramid-shaped, paired organs connected to the trachea by right and left bronchi.
- Diaphragm: flat, dome-shaped muscle at base of lungs and thoracic cavity.
- Lungs enclosed by pleurae, attached to the mediastinum.
- Right lung shorter and wider than left lung.
- Cardiac notch on left lung for heart space.
- Apex is the superior region, base is near the diaphragm.
- Costal surface borders ribs, mediastinal surface faces midline.
Lung Lobes
- Right lung: superior, middle and inferior lobes.
- Left lung: superior and inferior lobes.
- Fissures separate lobes.
Bronchopulmonary Segments
- Division of a lobe, each receives air from a tertiary bronchus and blood from its own artery.
- Targeted surgical removal possible.
Pulmonary Lobules
- Subdivision formed by bronchi branching into bronchioles.
- Each lobule receives a large bronchiole with multiple branches.
- Interlobular septum (connective tissue wall) separates lobules.
Lung Blood Supply
- Pulmonary circulation for gas exchange.
- Deoxygenated blood travels to lungs where erythrocytes pick up O2.
- Pulmonary artery carries deoxygenated blood to the alveoli.
- One arteriole and venule supply and drain a pulmonary lobule.
- Pulmonary capillary network with thin walls form respiratory membrane alongside alveolar walls for gas exchange.
- Oxygenated blood drains from alveoli through pulmonary veins.
Lung Innervation
- Sympathetic nervous system: bronchodilation.
- Parasympathetic nervous system: bronchoconstriction.
- Reflexes like coughing and O2/CO2 regulation through ANS control.
- Sensory nerve fibers from vagus nerve and thoracic ganglia.
- Pulmonary plexus at hilum innervates muscle fibers, glands and blood vessels.
Pleura
- Serous membrane surrounding each lung.
- Right and left pleurae separated by mediastinum.
- Visceral pleura: inner layer, superficial to lungs.
- Parietal pleura: outer layer, connects to thoracic wall, mediastinum, and diaphragm.
- Pleural cavity: space between visceral and parietal layers.
Pleural Fluid
- Secreted by mesothelial cells, lubricates pleural surfaces to prevent friction.
- Creates surface tension that adheres lungs to thoracic wall for expansion during ventilation.
Pulmonary Ventilation
- Act of breathing, movement of air in and out of lungs.
- Driven by pressure differences: atmospheric pressure (Patm), intra-alveolar pressure (Palv), intrapleural pressure (Pip).
Pressure Relationships
- Atmospheric pressure: force exerted by gases in atmosphere, 1 atm = 760 mmHg.
- Intra-alveolar pressure: force exerted by gases within the alveoli, equalizes with atmospheric pressure.
- Intrapleural pressure: force exerted by gases in pleural cavity, always lower than intra-alveolar pressure by about -4 mmHg.
Transpulmonary Pressure
- Difference between intrapleural and intra-alveolar pressures determines lung size.
- Higher transpulmonary pressure corresponds to a larger lung.
Boyle's Law
- Pressure of a gas is inversely proportional to its volume.
- Higher volume = lower pressure, lower volume = higher pressure.
Inspiration and Expiration
- Driven by pressure differences between atmosphere and lungs.
- Inspiration: atmospheric pressure > intra-alveolar pressure.
- Expiration: intra-alveolar pressure > atmospheric pressure.
Physical Factors Affecting Ventilation
- Lung elasticity, surface tension of alveolar fluid, surface tension of pleural fluid, thoracic wall elasticity.
- Muscle contraction/relaxation: diaphragm and intercostal muscles drive pressure changes.
- Resistance to airflow: primarily influenced by airway size.
Pulmonary Surfactant
- Secreted by type II alveolar cells.
- Reduces surface tension within alveoli to prevent collapse during expiration.
Thoracic Wall Compliance
- Ability of thoracic wall to stretch under pressure.
- Affects the effort required for breathing.
- Poor compliance makes thoracic expansion difficult.
Transpulmonary Pressure Definition
- It's the difference between the pressure inside the alveoli of the lungs (intra-alveolar pressure) and the pressure in the pleural cavity (intrapleural pressure).
- It determines lung size, as a higher transpulmonary pressure corresponds to a larger lung volume.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.