Podcast
Questions and Answers
Which of the following processes is NOT directly involved in respiration?
Which of the following processes is NOT directly involved in respiration?
- Systemic circulation of nutrients. (correct)
- Internal respiration.
- External respiration.
- Pulmonary ventilation.
Where does external respiration, a key component of overall respiration, take place?
Where does external respiration, a key component of overall respiration, take place?
- Within the cells during energy production.
- Within the heart chambers during circulation.
- Between the lungs and the blood. (correct)
- Between the blood and systemic tissues.
If a patient has damage to their larynx, which of the following functions would be MOST affected?
If a patient has damage to their larynx, which of the following functions would be MOST affected?
- Air filtration.
- Voice production. (correct)
- Gas exchange.
- Sense of smell.
A patient requires an emergency airway intervention due to upper airway obstruction. Which structure is incised in a cricothyrotomy?
A patient requires an emergency airway intervention due to upper airway obstruction. Which structure is incised in a cricothyrotomy?
What is the primary function of the epiglottis during swallowing?
What is the primary function of the epiglottis during swallowing?
Which anatomical structure is often used as a key landmark during endotracheal intubation?
Which anatomical structure is often used as a key landmark during endotracheal intubation?
What is the primary purpose of the C-shaped cartilage rings in the trachea?
What is the primary purpose of the C-shaped cartilage rings in the trachea?
Damage to the carina of the trachea may result in which of the following?
Damage to the carina of the trachea may result in which of the following?
How do the structural characteristics of bronchioles contribute to their function?
How do the structural characteristics of bronchioles contribute to their function?
Which structural change occurs in the respiratory tract as it transitions from bronchi to bronchioles in the conducting zone?
Which structural change occurs in the respiratory tract as it transitions from bronchi to bronchioles in the conducting zone?
What is the primary function of the respiratory bronchioles?
What is the primary function of the respiratory bronchioles?
How is the thinness of the respiratory membrane directly related to its function?
How is the thinness of the respiratory membrane directly related to its function?
What is the primary role of Type II alveolar cells in the respiratory membrane?
What is the primary role of Type II alveolar cells in the respiratory membrane?
Which function is associated with alveolar macrophages?
Which function is associated with alveolar macrophages?
What role do alveolar pores play in alveolar function?
What role do alveolar pores play in alveolar function?
How does pulmonary circulation differ from bronchial circulation in the lungs?
How does pulmonary circulation differ from bronchial circulation in the lungs?
What is the role of angiotensin-converting enzyme (ACE) in the lungs?
What is the role of angiotensin-converting enzyme (ACE) in the lungs?
Why is it important to maintain a negative intrapleural pressure?
Why is it important to maintain a negative intrapleural pressure?
How does the lymphatic system contribute to maintaining proper intrapleural pressure?
How does the lymphatic system contribute to maintaining proper intrapleural pressure?
What is the expected outcome if the intrapleural pressure equals or exceeds the intrapulmonary pressure?
What is the expected outcome if the intrapleural pressure equals or exceeds the intrapulmonary pressure?
Which of the following best describes the role of intrapleural pressure (Pip) in breathing?
Which of the following best describes the role of intrapleural pressure (Pip) in breathing?
Which of the following is TRUE regarding the mechanics of breathing?
Which of the following is TRUE regarding the mechanics of breathing?
Which event causes intrapulmonary pressure to increase during expiration?
Which event causes intrapulmonary pressure to increase during expiration?
What is the primary function of the conducting zone of the respiratory system?
What is the primary function of the conducting zone of the respiratory system?
Identify the main role of the paranasal sinuses present in the upper respiratory system.
Identify the main role of the paranasal sinuses present in the upper respiratory system.
What mechanisms does the respiratory system employ to protect against pathogens?
What mechanisms does the respiratory system employ to protect against pathogens?
In the bronchioles, which component significantly influences airway resistance?
In the bronchioles, which component significantly influences airway resistance?
Which change occurs as the respiratory tract transitions from bronchi to an alveolar duct?
Which change occurs as the respiratory tract transitions from bronchi to an alveolar duct?
How does fluid accumulation in the pleural cavity impact intrapleural pressure (Pip)?
How does fluid accumulation in the pleural cavity impact intrapleural pressure (Pip)?
What is the primary function of the smallest bronchioles in the respiratory tract?
What is the primary function of the smallest bronchioles in the respiratory tract?
Which characteristic makes the carina a trigger for coughing?
Which characteristic makes the carina a trigger for coughing?
What structural mechanism does the trachea employ to keep from collapsing?
What structural mechanism does the trachea employ to keep from collapsing?
How might an increase in thoracic cavity volume during inhalation affect pressure?
How might an increase in thoracic cavity volume during inhalation affect pressure?
What alteration in the lungs is facilitated by Type II alveolar cells?
What alteration in the lungs is facilitated by Type II alveolar cells?
Epithelial changes from pseudostratified columnar to cuboidal, what does that tell you?
Epithelial changes from pseudostratified columnar to cuboidal, what does that tell you?
What is a notable characteristic of the respiratory membrane that optimizes diffusion?
What is a notable characteristic of the respiratory membrane that optimizes diffusion?
In cases where there are blockages of the respitory system, which structure serves as an alternate route for air?
In cases where there are blockages of the respitory system, which structure serves as an alternate route for air?
Pulmonary arteries differ from other arteries by?
Pulmonary arteries differ from other arteries by?
When the body experiences pneumothorax resulting in compromised Pip, what follows?
When the body experiences pneumothorax resulting in compromised Pip, what follows?
Flashcards
Pulmonary Ventilation
Pulmonary Ventilation
The process of moving air into and out of the lungs.
External Respiration
External Respiration
Exchange of oxygen (O2) and carbon dioxide (CO2) between the lungs and blood.
Internal Respiration
Internal Respiration
Exchange of oxygen (O2) and carbon dioxide (CO2) between systemic blood vessels and tissues.
Upper Respiratory System
Upper Respiratory System
Signup and view all the flashcards
Lower Respiratory System
Lower Respiratory System
Signup and view all the flashcards
Larynx
Larynx
Signup and view all the flashcards
Three Functions of Larynx
Three Functions of Larynx
Signup and view all the flashcards
Trachea
Trachea
Signup and view all the flashcards
Trachea Mucosa
Trachea Mucosa
Signup and view all the flashcards
Trachea Submucosa
Trachea Submucosa
Signup and view all the flashcards
Trachea Cartilage
Trachea Cartilage
Signup and view all the flashcards
Trachea Adventitia
Trachea Adventitia
Signup and view all the flashcards
Trachealis
Trachealis
Signup and view all the flashcards
Carina
Carina
Signup and view all the flashcards
Segmental Bronchi
Segmental Bronchi
Signup and view all the flashcards
Bronchioles
Bronchioles
Signup and view all the flashcards
Terminal Bronchioles
Terminal Bronchioles
Signup and view all the flashcards
Conducting Zone
Conducting Zone
Signup and view all the flashcards
Respiratory Zone
Respiratory Zone
Signup and view all the flashcards
Respiratory Zone Start
Respiratory Zone Start
Signup and view all the flashcards
Alveolar Sacs
Alveolar Sacs
Signup and view all the flashcards
Respiratory Membrane
Respiratory Membrane
Signup and view all the flashcards
Respiratory Membrane Thickness
Respiratory Membrane Thickness
Signup and view all the flashcards
Type I Alveolar Cells
Type I Alveolar Cells
Signup and view all the flashcards
Type II Alveolar Cells
Type II Alveolar Cells
Signup and view all the flashcards
Alveolar Pores
Alveolar Pores
Signup and view all the flashcards
Pulmonary Arteries
Pulmonary Arteries
Signup and view all the flashcards
Pulmonary Veins
Pulmonary Veins
Signup and view all the flashcards
Lung Capillary Enzymes
Lung Capillary Enzymes
Signup and view all the flashcards
Bronchial Arteries
Bronchial Arteries
Signup and view all the flashcards
Inspiration
Inspiration
Signup and view all the flashcards
Expiration
Expiration
Signup and view all the flashcards
Atmospheric Pressure
Atmospheric Pressure
Signup and view all the flashcards
Intrapulmonary Pressure
Intrapulmonary Pressure
Signup and view all the flashcards
Intrapleural Pressure
Intrapleural Pressure
Signup and view all the flashcards
Lung Collapse
Lung Collapse
Signup and view all the flashcards
Outward Forces in Lungs
Outward Forces in Lungs
Signup and view all the flashcards
Transpulmonary Pressure
Transpulmonary Pressure
Signup and view all the flashcards
Study Notes
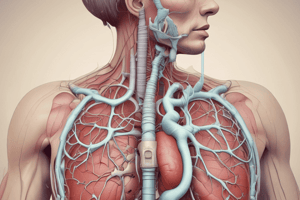
- Lecture 6 covers Respiratory System I and the functional anatomy of the respiratory system.
Elements of survival
- The average person can survive:
- 1-2 months without food
- 3 days without water
- 2-3 minutes without oxygen
Objectives of the lecture
- Learn the location, structure, and function of the upper respiratory system including the nose, nasal cavity, sinuses, and pharynx.
- Describe the protective mechanisms of the respiratory system.
- Learn the location, structure, and function of the lower respiratory system including the larynx, trachea, and bronchi.
- Describe the features of the bronchial tree.
Respiration
- Respiration involves four processes:
- Pulmonary ventilation: Movement of air into and out of the lungs (breathing)
- External respiration: Exchange of oxygen and carbon dioxide between the lungs and blood.
- Transport: Transport of oxygen and carbon dioxide in the blood.
- Internal respiration: Exchange of oxygen and carbon dioxide between systemic blood vessels and tissues.
- Respiratory System is comprised of the lungs, Pulmonary Circulation
- Circulatory system is comprised of Systemic Circulation
Functional Anatomy: Major Organs
- Major organs of the respiratory system can be divided into upper and lower respiratory system.
- Upper respiratory: nose and nasal cavity, paranasal sinuses, and pharynx
- Lower respiratory: larynx, trachea, bronchi and branches, lungs and alveoli
Lower Respiratory System
- Consists of the larynx, trachea, bronchi with microscopic structures, and lungs.
- Broken into two zones:
- Conducting zone: Conduits that transport gas to and from gas exchange sites, cleanses, warms, and humidifies air.
- Respiratory zone: Site of gas exchange.
- It has all other respiratory structures
- Has microscopic structures such as respiratory bronchioles, alveolar ducts, and alveoli
Lower Respiratory - Larynx
- The larynx (voice box) extends from the 3rd to 6th cervical vertebra and attaches to the hyoid bone.
- It opens into the laryngopharynx and is continuous with the trachea.
- There are three functions of the larynx:
- Provides a patent airway.
- Routes air and food into proper channels.
- Responsible for voice production
- Includes the vocal folds
Larynx - Epiglottis and Vallecula
- The epiglottis consists of elastic cartilage.
- Covers the laryngeal inlet during swallowing
- Covered in taste bud-containing mucosa
- Vallecula: Space between the epiglottis and tongue
- Important landmark during endotracheal intubation
The Trachea
- The trachea (windpipe) extends from the larynx into the mediastinum.
- It divides into two main bronchi.
- Approximately 4 inches long and ¾ inch in diameter.
- The tracheal wall has three layers:
- Mucosa: Ciliated pseudostratified epithelium containing goblet cells.
- Submucosa: Connective tissue with seromucous glands.
- Adventitia: Outer layer made of connective tissue, containing C-shaped cartilage rings for support.
The Trachea - Trachealis
- Trachealis consists of smooth muscle fibers that connect posterior parts of cartilage rings.
The Trachea - Carina
- The carina is the last tracheal cartilage.
- It expands at the point where the trachea branches into left and right bronchi.
- The right bronchus deviates 20 to 30 degrees from the midline.
- Compared to the left, it's smaller in diameter and twice as long.
- The left bronchus deviates 45 to 55 degrees from midline.
- Isothermic Saturation Boundary (ISB) is where air is 100% saturated at a temperature of 37°C.
- The mucosa of the carina is highly sensitive.
Bronchi and Subdivisions - Conducting Zone
- Each lobar bronchus branches into segmental (tertiary) bronchi, which divide repeatedly and become smaller.
- Bronchioles are less than 1 mm in diameter.
- Terminal bronchioles are the smallest of all branches and less than 0.5 mm in diameter.
- In the conducting zone, from bronchi to bronchioles, the structures change:
- Support structures change: cartilage rings become irregular plates, and elastic fibers replace cartilage altogether in bronchioles.
- Epithelium type changes: Pseudostratified columnar gives way to cuboidal, and cilia and goblet cells become more sparse.
- The amount of smooth muscle increases, which allows bronchioles to provide substantial resistance to air passage.
Bronchi and Subdivisions - Respiratory Zone
- The respiratory zone begins where terminal bronchioles feed into respiratory bronchioles.
- Respiratory bronchioles lead into alveolar ducts which then lead into alveolar sacs (saccules).
- Alveolar sacs have clusters of alveoli.
- Most lungs have 300 million alveoli that are the sites of gas exchange.
Bronchi and Subdivisions - Respiratory Membrane
- Respiratory membrane: Blood-air barrier consisting of alveolar and capillary walls along with their fused basement membranes.
- Very thin (~0.5 μm) allows gas exchange across the membrane by simple diffusion.
- Alveolar walls consist of:
- Single layer of squamous epithelium (type I alveolar cells).
- Scattered cuboidal type II alveolar cells secrete surfactant (and antimicrobial proteins).
Respiratory Membrane - Alveolar Wall
- Major cell types found in alveoli consist of:
- Single layer of squamous epithelium (type I alveolar cells).
- Scattered cuboidal type II alveolar cells secrete surfactant and antimicrobial proteins.
- Alveolar macrophages keep alveolar surfaces sterile, with 2 million dead macrophages/hour carried by cilia to the throat and swallowed.
- Other features of alveoli:
- Surrounded by fine elastic fibers and pulmonary capillaries.
- Alveolar pores connect adjacent alveoli, equalize air pressure throughout the lung, and provide alternate routes in case of blockages.
Gross Anatomy of the Lungs - Blood and Nerve Supply
- Lungs are perfused by two circulations:
- Pulmonary circulation: Pulmonary arteries deliver systemic venous blood from the heart to lungs for oxygenation.
- Branches feed into pulmonary capillary networks where gas exchange occurs.
- Pulmonary veins carry oxygenated blood from respiratory zones back to the heart.
- Low-pressure, high-volume system.
- Lung capillary endothelium contains many enzymes that act on different substances in blood, like angiotensin-converting enzyme (blood pressure).
- Bronchial circulation: Bronchial arteries provide oxygenated blood to lung tissue
- These arise from the aorta and enter lungs at hilum.
- It supplies all lung tissue except alveoli.
- Bronchial veins anastomose with pulmonary veins, which carry most venous blood back to the heart.
- Pulmonary circulation: Pulmonary arteries deliver systemic venous blood from the heart to lungs for oxygenation.
Respiratory Physiology
- Pulmonary ventilation consists of two phases:
- Inspiration: Gases flow into lungs.
- Expiration: Gases exit lungs.
Pressure Relationships in the Thoracic Cavity
- Atmospheric Pressure (Patm): the pressure exerted by the air surrounding the body.
- At sea level 760 mm Hg equals one atmosphere.
- Respiratory pressures are described relative to atmospheric pressure.
- A respiratory pressure of -5 mm Hg means the pressure is lower than Patm by 5 mm Hg.
Pressure Relationships in Thoracic Cavity: Intrapulmonary Pressure
- Intrapulmonary Pressure (Ppul): Pressure in the alveoli also called intra-alveolar pressure.
- Fluctuates with breathing, but always eventually equalizes with Patm
Pressure Relationships in Thoracic Cavity: Intrapleural Pressure
- Intrapleural Pressure (Pip): Pressure in the pleural cavity
- Fluctuates with breathing and is always a negative pressure (less than Patm and Ppul).
- Usually 4 mm Hg less than Ppul
- A minimum amount of fluid level must be maintained, with excess fluid pumped out by the lymphatic system.
- If fluid accumulates, positive Pip pressure develops, leading to lung collapse.
Pressure Relationships in Thoracic Cavity: Intrapleural Pressure
- Two inward forces promote lung collapse:
- Lungs' natural tendency to recoil (because of elasticity, lungs always try to assume the smallest size).
- Surface tension of the alveolar fluid: Surface tension pulls on alveoli to try to reduce alveolar size.
- One outward force promotes lung expansion: Elasticity of the chest wall pulls the thorax outward or like a compressed spring.
- One outward force tends to enlarge lungs:
- Elasticity of chest wall pulls thorax outward 'like a compressed spring'
- Negative Pip is affected by opposing forces, maintained by strong adhesive force between parietal and visceral pleurae
- Chest wall pulls outward into the intrapleural space.
- It causes forces created by recoil and surface tension.
- Lungs pull inward that tends to separate the visceral and parietal pleurae.
Pressure Relationships in Thoracic Cavity - Transpulmonary Pressure
- Transpulmonary pressure is the difference between intrapulmonary and intrapleural pressures (Ppul - Pip) and keeps air spaces in the lungs open.
- If this is compromised (pneumothorax), transpulmonary pressure will fail.
- In order for lungs to not fail and remain inflated the negative Pip must be maintained.
Changes in Pip and Ppul During Inspiration and Expiration
- During Inspiration
- Pressure inside lung decreases as lung volume increases
- Pleural cavity pressure becomes more negative as chest wall expands
- During Expiration
- Pressure inside lung increases
- Pleural cavity pressure returns to initial value
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.