Podcast
Questions and Answers
Which structural feature is present in respiratory bronchioles but absent in alveolar ducts?
Which structural feature is present in respiratory bronchioles but absent in alveolar ducts?
- Type I pneumocytes
- Cilia (correct)
- Alveoli
- Elastic fibers
What is the primary function of alveolar macrophages within the alveoli?
What is the primary function of alveolar macrophages within the alveoli?
- Removing dust and debris (correct)
- Synthesizing pulmonary surfactant
- Regenerating alveolar cells
- Facilitating gas exchange
If a disease damages type II pneumocytes, which of the following direct consequences is most likely to occur in the lungs?
If a disease damages type II pneumocytes, which of the following direct consequences is most likely to occur in the lungs?
- Restricted regeneration of alveolar macrophages
- Excessive production of elastic fibers
- Inability to remove debris from the alveoli
- Increased surface tension in the alveoli (correct)
The respiratory zone is characterized by which of the following?
The respiratory zone is characterized by which of the following?
After migrating to the bronchioles, what happens to the debris-laden alveolar macrophages?
After migrating to the bronchioles, what happens to the debris-laden alveolar macrophages?
Which of the following is the primary function of the conducting zone of the respiratory system?
Which of the following is the primary function of the conducting zone of the respiratory system?
What structural feature primarily supports the patency (openness) of the conducting airways lacking cartilage?
What structural feature primarily supports the patency (openness) of the conducting airways lacking cartilage?
How do sympathetic adrenergic neurons influence the smooth muscle of the conducting airways, and what receptor mediates this effect?
How do sympathetic adrenergic neurons influence the smooth muscle of the conducting airways, and what receptor mediates this effect?
Which generation of conducting airways marks the disappearance of cartilage in their walls?
Which generation of conducting airways marks the disappearance of cartilage in their walls?
A patient with asthma experiences bronchoconstriction. Which type of medication would be most effective in providing immediate relief by dilating the airways?
A patient with asthma experiences bronchoconstriction. Which type of medication would be most effective in providing immediate relief by dilating the airways?
What is the role of ciliated cells in the conducting airways?
What is the role of ciliated cells in the conducting airways?
How does the parasympathetic nervous system affect the conducting airways?
How does the parasympathetic nervous system affect the conducting airways?
In which zone of the respiratory system does gas exchange primarily occur?
In which zone of the respiratory system does gas exchange primarily occur?
A researcher is studying lung tissue samples under a microscope. Which characteristic would help them differentiate between alveolar ducts and respiratory bronchioles?
A researcher is studying lung tissue samples under a microscope. Which characteristic would help them differentiate between alveolar ducts and respiratory bronchioles?
During an autopsy, a pathologist observes an abnormally high amount of debris accumulated within the alveoli. Which of the following cell types is most likely to be impaired in its function?
During an autopsy, a pathologist observes an abnormally high amount of debris accumulated within the alveoli. Which of the following cell types is most likely to be impaired in its function?
A premature infant is born with a deficiency in pulmonary surfactant. Which immediate physiological challenge is the infant most likely to face?
A premature infant is born with a deficiency in pulmonary surfactant. Which immediate physiological challenge is the infant most likely to face?
A scientist is investigating the regenerative capacity of lung cells following an injury. Damage to which cell type would most significantly impair the repair of both type I and type II pneumocytes?
A scientist is investigating the regenerative capacity of lung cells following an injury. Damage to which cell type would most significantly impair the repair of both type I and type II pneumocytes?
A sample of lung tissue is analyzed and found to have a reduced number of alveolar macrophages. This deficiency would most directly impair which process?
A sample of lung tissue is analyzed and found to have a reduced number of alveolar macrophages. This deficiency would most directly impair which process?
Which mechanism primarily prevents the collapse of conducting airways lacking cartilage?
Which mechanism primarily prevents the collapse of conducting airways lacking cartilage?
A researcher is studying the effects of different bronchodilators on airway diameter. Which receptor type, when activated, would be expected to cause bronchodilation?
A researcher is studying the effects of different bronchodilators on airway diameter. Which receptor type, when activated, would be expected to cause bronchodilation?
In the respiratory system, which of the following is the primary role of the mucociliary transport system?
In the respiratory system, which of the following is the primary role of the mucociliary transport system?
If a patient's autonomic nervous system is stimulating muscarinic receptors in the lungs, what physiological response would be expected?
If a patient's autonomic nervous system is stimulating muscarinic receptors in the lungs, what physiological response would be expected?
In which generation of conducting airways does cartilage begin to disappear from the airway walls?
In which generation of conducting airways does cartilage begin to disappear from the airway walls?
A pharmaceutical company is developing a new drug to treat asthma. Which of the following mechanisms of action would be most effective in dilating the airways?
A pharmaceutical company is developing a new drug to treat asthma. Which of the following mechanisms of action would be most effective in dilating the airways?
Which of the following best describes the function of the conducting zone of the respiratory system?
Which of the following best describes the function of the conducting zone of the respiratory system?
A patient has a condition that impairs the function of their ciliated cells. What is the most likely consequence of this condition?
A patient has a condition that impairs the function of their ciliated cells. What is the most likely consequence of this condition?
Flashcards
Respiratory Zone
Respiratory Zone
Part of the lung where gas exchange occurs, includes respiratory bronchioles, alveolar ducts, and alveolar sacs.
Respiratory Bronchioles
Respiratory Bronchioles
Transitional structures with both cilia and alveoli for gas exchange.
Alveoli
Alveoli
Small pouches in the lungs, about 300 million per lung, where gas exchange primarily occurs.
Type II Pneumocytes
Type II Pneumocytes
Signup and view all the flashcards
Alveolar Macrophages
Alveolar Macrophages
Signup and view all the flashcards
Conducting Zone
Conducting Zone
Signup and view all the flashcards
Function of Conducting Zone
Function of Conducting Zone
Signup and view all the flashcards
Trachea
Trachea
Signup and view all the flashcards
Cartilage in Airways
Cartilage in Airways
Signup and view all the flashcards
Mucus and Ciliated Cells
Mucus and Ciliated Cells
Signup and view all the flashcards
Sympathetic Effect on Airways
Sympathetic Effect on Airways
Signup and view all the flashcards
Parasympathetic Effect on Airways
Parasympathetic Effect on Airways
Signup and view all the flashcards
What is the Respiratory Zone?
What is the Respiratory Zone?
Signup and view all the flashcards
Alveolar Ducts
Alveolar Ducts
Signup and view all the flashcards
Alveolar Sacs
Alveolar Sacs
Signup and view all the flashcards
Type I and Type II Pneumocytes
Type I and Type II Pneumocytes
Signup and view all the flashcards
Respiratory System
Respiratory System
Signup and view all the flashcards
Airway Generation
Airway Generation
Signup and view all the flashcards
Sympathetic Nervous System Effect
Sympathetic Nervous System Effect
Signup and view all the flashcards
Parasympathetic Nervous System Effect
Parasympathetic Nervous System Effect
Signup and view all the flashcards
Structural Support Function
Structural Support Function
Signup and view all the flashcards
β₂-Adrenergic Agonists
β₂-Adrenergic Agonists
Signup and view all the flashcards
Study Notes
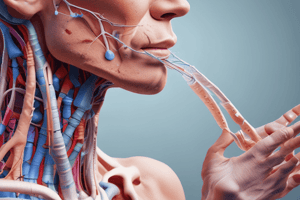
- The respiratory system includes the lungs and a series of airways that connect the lungs to the external environment
- The respiratory system is subdivided into conducting and respiratory zones with differing structures and functions.
Conducting Zone
- Includes the nose, nasopharynx, larynx, trachea, bronchi, bronchioles, and terminal bronchioles
- Functions to bring air into and out of the respiratory zone
- Warms, humidifies and filters air before it reaches the gas exchange region
- Progressively bifurcating airways are referred to by generation number
- The trachea, or zeroth generation, is the main conducting airway
- The trachea divides into the right and left mainstem bronchi (first generation), then into smaller bronchi, continuing through 23 generations, and culminating in the airways of the 23rd generation.
- Cartilage is present in the walls of the 0th-10th generations to keep airways open
- From the 11th generation, cartilage disappears and airways depend on transmural pressure
- Conducting airways are lined with mucus-secreting and ciliated cells to remove inhaled particles
- Large particles are filtered out in the nose, while small particles are captured by mucus and swept upward by cilia
- Smooth muscle in the conducting airways is regulated by the autonomic nervous system
- Sympathetic adrenergic neurons activate β2 receptors on bronchial smooth muscle to cause relaxation and dilation of the airways
- β2 receptors are activated by epinephrine from the adrenal medulla and by β2-adrenergic agonists like isoproterenol
- Parasympathetic cholinergic neurons activate muscarinic receptors for contraction and constriction of airways
- Changes in airway diameter affect airway resistance, altering airflow
- β2-adrenergic agonists (e.g., epinephrine, isoproterenol, albuterol) are used to dilate airways in the treatment of asthma
Respiratory Zone
- Includes structures lined with alveoli, allowing gas exchange: respiratory bronchioles, alveolar ducts, and alveolar sacs
- Respiratory bronchioles are transitional structures with cilia and smooth muscle like conducting airways, but also participate in gas exchange from alveoli occasionally bud off their walls
- Alveolar ducts are completely lined with alveoli, but contain no cilia and little smooth muscle
- Alveolar sacs are the terminal structures of the respiratory zone, which are also lined with alveoli.
- Alveoli are pouchlike evaginations of the respiratory bronchioles, alveolar ducts, and alveolar sacs
- Each lung contains about 300 million alveoli, with a diameter of ~200 micrometers (μm)
- Thin alveolar walls and large surface area allow for rapid and efficient diffusion of oxygen (O2) and carbon dioxide (CO2) between alveolar gas and pulmonary capillary blood
- Alveolar walls contain elastic fibers and epithelial cells called type I and type II pneumocytes (alveolar cells)
- Type II pneumocytes synthesize pulmonary surfactant, which reduces surface tension in the alveoli, and they have regenerative capacity for type I and type II pneumocytes
- Alveoli also contain phagocytic cells called alveolar macrophages, that keep the alveoli free of dust and debris, because alveoli have no cilia
- Macrophages migrate to the bronchioles, where cilia transport debris to the pharynx for swallowing or expectoration
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
The respiratory system connects the lungs to the external environment. It's divided into conducting and respiratory zones. The conducting zone includes the nose, larynx, trachea, and bronchioles, warming and filtering air.