Podcast
Questions and Answers
Which symptoms indicate uncontrolled asthma?
Which symptoms indicate uncontrolled asthma?
- Rescue drug needed less than twice weekly
- Symptoms limiting activity once a week
- Waking from night sleep with symptoms occurring three to four times a week (correct)
- Daytime symptoms occurring only once a week
What is the primary goal of asthma management?
What is the primary goal of asthma management?
- Achieve complete avoidance of allergens
- Improve airflow and gas exchange (correct)
- Reduce the frequency of rescue medication use
- Eliminate all symptoms completely
Which type of asthma medication is classified as a rescue drug?
Which type of asthma medication is classified as a rescue drug?
- Long acting beta agonists (LABAs)
- Corticosteroids
- Leukotriene modifiers
- Short acting beta adrenergic agonists (SABAs) (correct)
What test can help identify specific allergens related to asthma?
What test can help identify specific allergens related to asthma?
Which of the following is a common characteristic of moderate persistent asthma?
Which of the following is a common characteristic of moderate persistent asthma?
What is a vital component of asthma management related to education?
What is a vital component of asthma management related to education?
Which of the following drugs is an anticholinergic used for asthma treatment?
Which of the following drugs is an anticholinergic used for asthma treatment?
What percentage of eosinophils in blood tests can indicate allergic conditions associated with asthma?
What percentage of eosinophils in blood tests can indicate allergic conditions associated with asthma?
What is the primary function of alveoli in the respiratory system?
What is the primary function of alveoli in the respiratory system?
Which of the following characteristics is associated with the pediatric respiratory system?
Which of the following characteristics is associated with the pediatric respiratory system?
Asthma in children is most prevalent in which age group?
Asthma in children is most prevalent in which age group?
What contributes to bronchospasm in asthma conditions?
What contributes to bronchospasm in asthma conditions?
Which factor increases the risk of asthma in children?
Which factor increases the risk of asthma in children?
What is the role of surfactant in the respiratory system?
What is the role of surfactant in the respiratory system?
Which condition is characterized by inflammation and increased sensitivity of airway tissues?
Which condition is characterized by inflammation and increased sensitivity of airway tissues?
What is one common physiological feature of infants regarding respiration?
What is one common physiological feature of infants regarding respiration?
What substance is primarily released by mast cells during an immediate allergic reaction?
What substance is primarily released by mast cells during an immediate allergic reaction?
Which of the following is NOT a non-allergenic stimulus that can cause bronchoconstriction?
Which of the following is NOT a non-allergenic stimulus that can cause bronchoconstriction?
What is a characteristic feature of the late reaction in asthma?
What is a characteristic feature of the late reaction in asthma?
Which assessment finding is NOT typically associated with an acute asthma attack?
Which assessment finding is NOT typically associated with an acute asthma attack?
What type of assessment could indicate a decreased forced vital capacity (FVC) in asthmatic patients?
What type of assessment could indicate a decreased forced vital capacity (FVC) in asthmatic patients?
Which of the following is considered a risk factor for asthma?
Which of the following is considered a risk factor for asthma?
What is a common environmental trigger for asthma that can lead to an exacerbation?
What is a common environmental trigger for asthma that can lead to an exacerbation?
In what position might individuals with severe asthma exacerbations be found to alleviate breathing difficulty?
In what position might individuals with severe asthma exacerbations be found to alleviate breathing difficulty?
Which medication is classified as a long-acting beta 2 adrenergic agent?
Which medication is classified as a long-acting beta 2 adrenergic agent?
What combination medication includes both an inhaled corticosteroid and a long-acting beta 2 adrenergic agent?
What combination medication includes both an inhaled corticosteroid and a long-acting beta 2 adrenergic agent?
Which of the following is a sign indicating the need for emergency treatment due to asthma exacerbation?
Which of the following is a sign indicating the need for emergency treatment due to asthma exacerbation?
Which of the following medications is an anti-IgE antibody used for allergic asthma?
Which of the following medications is an anti-IgE antibody used for allergic asthma?
What is the main purpose of leukotriene inhibitors in asthma management?
What is the main purpose of leukotriene inhibitors in asthma management?
Which scenario best describes status asthmaticus?
Which scenario best describes status asthmaticus?
What environmental modification can help reduce asthma triggers related to dust?
What environmental modification can help reduce asthma triggers related to dust?
What should be monitored to prevent toxicity in patients taking theophylline?
What should be monitored to prevent toxicity in patients taking theophylline?
Flashcards are hidden until you start studying
Study Notes
Key Concepts
- Gas Exchange is the central focus.
- Interrelated concepts: Perfusion, Inflammation, Cellular Regulation.
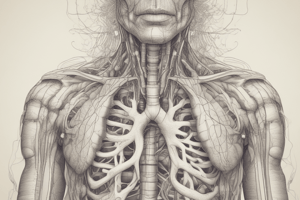
Respiratory System Overview
- Upper Airway: Comprises nares, pharynx, and larynx (housing vocal cords).
- Lower Airway: Includes trachea, bronchi, bronchioles, and alveoli (site of gas exchange).
Pediatric vs. Adult Respiratory System
- Infants have less surfactant and smaller, undeveloped airways.
- Infants are obligatory nose breathers and exhibit poorly developed intercostal muscles.
- Newborns often experience brief apnea.
- Faster respiratory rate and metabolic needs in pediatrics.
- Eustachian tubes are relatively horizontal, increasing risk for ear infections.
- Enlarged tonsillar tissue and a more flexible larynx, prone to spasms.
- Children tend to be abdominal breathers.
Asthma: Incidence and Prevalence
- Asthma can develop at any age, peaking between 10-17 years.
- It's a leading cause of acute/chronic illness in children, prevalent in 8.3% of U.S. children.
- Higher incidence in African American and urban populations.
Asthma Pathophysiology
- Characterized as a chronic, intermittent disease with genetic and environmental influences.
- Leads to airway inflammation and hypersensitivity.
- Immediate Reaction: Allergen activation of IgE receptors causes bronchoconstriction through histamines and leukotrienes.
- Late Reaction: Involves eosinophils and neutrophils which contribute to prolonged bronchoconstriction and hyperresponsive airways.
Asthma Assessment: History
- Consider risk factors: family history, previous wheezing episodes, and respiratory infections.
- Note symptoms like coughing (especially at night or post-exercise), shortness of breath (SOB), and allergies.
Asthma Triggers
- Cold air, smoke, allergens (pollen, mold), respiratory infections, stress, exercise, environmental pollutants, specific foods, and medications can provoke symptoms.
Asthma Signs and Symptoms
- Monitor vital signs (heart rate, respiratory rate), check for wheezing, stridor, and chest tightness.
- Observe for use of accessory muscles during respiratory distress and symptoms of anxiety or restlessness.
- Symptoms may worsen at night and lead to difficulty with talking or eating.
Asthma Diagnostics
- Laboratory assessments include pulse oximetry, end-tidal CO2 monitoring, and arterial blood gases (ABGs).
- Use of a peak flow meter for daily monitoring is recommended.
- Diagnostic pulmonary function tests show decreased FVC and FEV1.
Classification of Asthma
- Intermittent, Mild Persistent, Moderate Persistent, and Severe Persistent classifications exist for management strategies.
Therapeutic Management of Asthma
- Aim to improve airflow and gas exchange through swift recognition of symptoms, adherence to action plans, trigger avoidance, medication administration, and education.
Asthma Medications
- Rescue Drugs: SABA (short-acting beta-agonists), bronchodilators like Albuterol, Ipratropium bromide.
- Control Therapy: Long-term anti-inflammatory agents (e.g., Budesonide), LABAs (e.g., Salmeterol), leukotriene inhibitors (Montelukast), and anti-IgE treatments (Omalizumab).
Emergency Indicators for Asthma
- Symptoms necessitating emergency treatment include worsening cough/wheeze, lack of response to bronchodilators, difficulty breathing, or listlessness.
- Signs of insufficient aeration or cyanosis indicate a critical state needing immediate intervention.
Status Asthmaticus
- A severe, potentially life-threatening asthma episode that may not respond to standard treatment.
- Requires urgent IV fluids, systemic bronchodilators, steroids, epinephrine, and oxygen.
Asthma Action Plan
- Recommendations and resources for managing asthma episodes effectively.
Environmental Modifications
- Implement changes to reduce exposure to Pollen and Dust, such as regular washing of bedding, avoiding certain materials, using air filters, and maintaining household humidity levels.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.