Podcast
Questions and Answers
What is the primary function of lysozyme and defensins secreted by serous and mucus-producing cells?
What is the primary function of lysozyme and defensins secreted by serous and mucus-producing cells?
- To produce sound via vocal cords
- To provide structural support to the larynx
- To offer antibacterial protection (correct)
- To regulate air volume in the lungs
Which regions divide the pharynx?
Which regions divide the pharynx?
- Nasopharynx, laryngopharynx, hypopharynx
- Oropharynx, trachea, laryngopharynx
- Nasopharynx, oropharynx, trachea
- Nasopharynx, oropharynx, laryngopharynx (correct)
What significant feature does the thyroid cartilage possess?
What significant feature does the thyroid cartilage possess?
- It is located superior to the cricoid cartilage
- It is the largest cartilage of the larynx (correct)
- It contains the epiglottis
- It is the smallest cartilage in the larynx
What role does the epiglottis play when it is in the closed position?
What role does the epiglottis play when it is in the closed position?
Which cartilages are involved in the movement of the vocal cords?
Which cartilages are involved in the movement of the vocal cords?
How many C-shaped pieces of cartilage comprise the trachea?
How many C-shaped pieces of cartilage comprise the trachea?
What is the main purpose of the trachealis muscle and elastic connective tissue in the trachea?
What is the main purpose of the trachealis muscle and elastic connective tissue in the trachea?
Which part of the larynx is known as the 'Adam's apple'?
Which part of the larynx is known as the 'Adam's apple'?
What is the primary function of type II alveolar cells?
What is the primary function of type II alveolar cells?
Which of the following is NOT a characteristic of asthma?
Which of the following is NOT a characteristic of asthma?
What role do alveolar macrophages play in the respiratory system?
What role do alveolar macrophages play in the respiratory system?
Which of the following triggers might lead to an asthma attack?
Which of the following triggers might lead to an asthma attack?
What is a common symptom of a severe asthma attack requiring immediate medical attention?
What is a common symptom of a severe asthma attack requiring immediate medical attention?
Which type of cell primarily constitutes the alveolar surface area?
Which type of cell primarily constitutes the alveolar surface area?
How can asthma medications be delivered to young children who have difficulty using an inhaler?
How can asthma medications be delivered to young children who have difficulty using an inhaler?
What is the thickness of type I alveolar cells approximately?
What is the thickness of type I alveolar cells approximately?
What is the primary function of the pleural fluid during breathing?
What is the primary function of the pleural fluid during breathing?
Which statement describes Boyle's Law?
Which statement describes Boyle's Law?
What role does atmospheric pressure play in pulmonary ventilation?
What role does atmospheric pressure play in pulmonary ventilation?
What is the effect of increasing the volume within a container of gas, according to Boyle's Law?
What is the effect of increasing the volume within a container of gas, according to Boyle's Law?
How does the pleurae contribute to preventing the spread of infection?
How does the pleurae contribute to preventing the spread of infection?
What factors drive pulmonary ventilation?
What factors drive pulmonary ventilation?
During inhalation, what happens to the intrapleural pressure?
During inhalation, what happens to the intrapleural pressure?
What happens when the volume of gas in a container decreases?
What happens when the volume of gas in a container decreases?
At what week does significant respiratory development milestones occur for premature infants?
At what week does significant respiratory development milestones occur for premature infants?
What is the main function of pulmonary surfactant produced late in pregnancy?
What is the main function of pulmonary surfactant produced late in pregnancy?
What percentage of infants born between 26 and 28 weeks may develop respiratory distress syndrome?
What percentage of infants born between 26 and 28 weeks may develop respiratory distress syndrome?
What is a characteristic of fetal breathing movements observed during development?
What is a characteristic of fetal breathing movements observed during development?
When does the formation of pulmonary capillaries primarily occur in fetal development?
When does the formation of pulmonary capillaries primarily occur in fetal development?
What happens to the fetal lungs during passage through the birth canal?
What happens to the fetal lungs during passage through the birth canal?
At what age does a full complement of functional alveoli typically develop?
At what age does a full complement of functional alveoli typically develop?
What does respiratory distress syndrome primarily occur in infants born at?
What does respiratory distress syndrome primarily occur in infants born at?
What is the primary function of the trachealis muscle?
What is the primary function of the trachealis muscle?
Which type of epithelium lines the bronchial tree?
Which type of epithelium lines the bronchial tree?
What role do alveolar pores play in the lung?
What role do alveolar pores play in the lung?
At which point does the respiratory zone begin?
At which point does the respiratory zone begin?
How many terminal bronchioles are there approximately in each lung?
How many terminal bronchioles are there approximately in each lung?
What is the significance of cartilage rings in the trachea?
What is the significance of cartilage rings in the trachea?
What initiates violent coughing at the carina?
What initiates violent coughing at the carina?
What characterizes the walls of bronchioles compared to bronchi?
What characterizes the walls of bronchioles compared to bronchi?
Flashcards are hidden until you start studying
Study Notes
Serous and Mucous Producing Cells
- Secrete lysozyme enzyme and defensins, both of which have antibacterial properties.
- Immune cells help protect connective tissue deep to the respiratory epithelium.
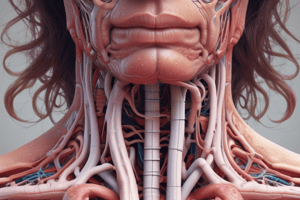
Pharynx
- A tube formed by skeletal muscle and lined with mucous membrane that's continuous with the nasal cavities.
- Divided into three regions: nasopharynx, oropharynx, and laryngopharynx.
Larynx
- Cartilaginous structure inferior to the laryngopharynx.
- Connects the pharynx to the trachea.
- Regulates the volume of air that enters and leaves the lungs.
- Composed of several pieces of cartilage including the thyroid cartilage, epiglottis, and cricoid cartilage.
- The thyroid cartilage is the largest cartilage piece of the larynx and contains the laryngeal prominence, or "Adam's apple."
- The cricoid cartilage is thick and makes a ring, with a wider region posteriorly and a thinner region anteriorly.
- Three smaller pairs of cartilages, including the arytenoids, corniculates, and cuneiforms, attach to the epiglottis and vocal cords.
- The epiglottis attaches to the thyroid cartilage and is a very flexible piece of elastic cartilage that covers the opening of the trachea.
- The glottis contains the vestibular folds, true vocal cords, and the space between these folds.
- A vestibular fold, or false vocal cord, is a folded section of mucous membrane.
- A true vocal cord is a white, membranous fold attached to the thyroid and arytenoid cartilages of the larynx.
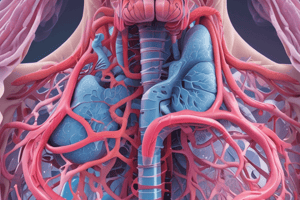
Trachea
- Extends from the larynx to the lungs.
- Consists of 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue.
- The trachealis muscle and elastic connective tissue forms the fibroelastic membrane, which is flexible membrane connecting the C-shaped cartilages.
- The fibroelastic membrane allows the trachea to expand during inhalation and exhalation, and the rings of cartilage provide structural support.
- The fibroelastic membrane helps to prevent the trachea from collapsing.
- The trachealis muscle can contract to force air through the trachea during exhalation.
- Lined with pseudostratified ciliated columnar epithelium.
Bronchial Tree
- The trachea branches into the right and left primary bronchi at the carina.
- Bronchi are lined by pseudostratified ciliated columnar epithelium that contains mucus-producing goblet cells.
- The carina is a raised structure that triggers coughing if foreign bodies are present.
- The main function of the bronchi is to provide a passageway for air to move into and out of each lung.
- Mucous membranes trap debris and pathogens.
- A bronchiole branches from the tertiary bronchi.
- Bronchioles further branch, becoming terminal bronchioles, which lead to the respiratory zone structures involved in gas exchange.
- There are over 1000 terminal bronchioles in each lung.
- The muscular walls of the bronchioles do not contain cartilage.
- The muscular wall can change the size of the tubing to increase or decrease airflow.
Respiratory Zone
- Directly involved in gas exchange.
- Begins where the terminal bronchioles join the respiratory bronchiole, the smallest type of bronchiole.
- Respiratory bronchioles lead to alveolar ducts and a cluster of alveoli.
Alveoli
- An alveolar duct is a tube composed of smooth muscle and connective tissue.
- An alveolus is a small, grape-like sac attached to the alveolar duct.
- An alveolar sac is a cluster of alveoli that are responsible for gas exchange.
- An alveolus is 200 mm in diameter and has elastic walls that allow it to stretch with each breath.
- Alveoli are connected by alveolar pores that maintain equal air pressure.
- The alveolar wall contains three cell types: type I alveolar cells, type II alveolar cells, and alveolar macrophages.
- Type I alveolar cells are squamous epithelial cells that make up 97% of the alveolar surface area.
- Type II alveolar cells secrete pulmonary surfactant.
- Alveolar macrophages remove debris and pathogens.
Asthma
- Chronic disease affecting the lungs in both children and adults.
- Characterized by inflammation, airway edema, bronchospasms, and excessive mucus secretion.
- Immune cells like eosinophils and mononuclear cells may infiltrate the bronchi and bronchioles.
- Attacks are triggered by environmental factors such as dust, pollen, pet hair, changes in the weather, mold, tobacco smoke, respiratory infections, exercise, and stress.
- Asthma attacks cause coughing, shortness of breath, wheezing, and tightness of the chest.
- Severe attacks may cause difficulty breathing, blue lips, confusion, drowsiness, rapid pulse, sweating, and anxiety.
The Pleurae
- The layer that covers the lungs is called the visceral pleura.
- The outer layer lining the thoracic cavity is called the parietal pleura.
- The pleural cavity contains pleural fluid that acts as lubrication to reduce friction and prevent trauma during breathing.
- Pleural fluid helps maintain the position of the lungs against the thoracic wall.
- The pleurae create a barrier between major organs.
The Process of Breathing (Pulmonary ventilation):
- The movement of air into and out of the lungs.
- The major mechanisms of pulmonary ventilation involve atmospheric pressure, alveolar pressure, and intrapleural pressure.
- Inspiration and expiration depend on the differences in pressure between the atmosphere and the lungs.
Pressure Relationships
- Pressure is created by the movement of molecules confined in an area.
- Boyle's Law describes the relationship between the volume and pressure of a gas at a constant temperature.
- Boyle's Law states that the pressure of a gas is inversely proportional to its volume.
- Atmospheric pressure is the force that is exerted by gases in the surrounding air.
Development of the Lungs
- Major growth and maturation of the respiratory system occurs between week 24 of gestation through term.
- Alveolar precursors develop and larger amounts of pulmonary surfactant are produced.
- Surfactant levels are inadequate to create effective lung compliance until about the eighth month of pregnancy.
- The respiratory system continues to expand, and the surfaces that will form the respiratory membrane develop further.
- Pulmonary capillaries form and expand creating a larger surface area for gas exchange.
- At week 28, a baby born prematurely can usually breathe on its own.
- Alveoli continue to develop and mature through childhood.
- A full complement of functional alveoli does not appear until around 8 years of age.
- Fetal breathing movements begin at 20-21 weeks of development.
- Fetal breathing movements involve muscle contractions that cause the inhalation and exhalation of amniotic fluid, surfactant, and mucus.
Birth
- Prior to birth, the lungs are filled with amniotic fluid, mucus, and surfactant.
- The fetal thoracic cavity is compressed, expelling some of the fluid.
- Remaining fluid is absorbed shortly after birth.
- The first inhalation occurs within 10 seconds after birth and inflates the lungs.
- Pulmonary surfactant is critical for lung inflation.
- Preterm birth before 26 weeks frequently results in respiratory distress syndrome.
Respiratory Distress Syndrome (RDS)
- Primarily occurs in infants born prematurely.
- Up to 50% of infants born between 26 and 28 weeks, and fewer than 30% of infants born between 30 and 31 weeks, develop RDS.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.