Podcast
Questions and Answers
Which of the following is the primary function of the respiratory system?
Which of the following is the primary function of the respiratory system?
- Filtering air to remove all harmful substances.
- Maintaining a constant body temperature.
- Producing vocalizations for communication.
- Exchanging oxygen and carbon dioxide between air and blood. (correct)
How does the respiratory system contribute to maintaining a stable body pH?
How does the respiratory system contribute to maintaining a stable body pH?
- By directly neutralizing acids and bases in the blood.
- By regulating carbon dioxide levels in the blood. (correct)
- By filtering acidic substances from inhaled air.
- By producing buffers that counteract pH changes.
Which of the following is the main function of the upper respiratory tract?
Which of the following is the main function of the upper respiratory tract?
- Facilitating the exchange of oxygen and carbon dioxide.
- Controlling the rate and depth of breathing.
- Warming, wetting and filtering the air. (correct)
- Regulating blood pressure through gas exchange.
How does the filtering action of the upper respiratory tract remove particles?
How does the filtering action of the upper respiratory tract remove particles?
What anatomical structures comprise the lower respiratory tract?
What anatomical structures comprise the lower respiratory tract?
How would you describe the function of the thoracic cage during breathing?
How would you describe the function of the thoracic cage during breathing?
What are the series of the structures in the 'conducting system' of the lungs?
What are the series of the structures in the 'conducting system' of the lungs?
How do the number and size of airways change from the trachea to the alveoli and why?
How do the number and size of airways change from the trachea to the alveoli and why?
What is the primary function of alveoli in the respiratory system?
What is the primary function of alveoli in the respiratory system?
How do pulmonary arterioles and venules contribute to gas exchange at the alveoli?
How do pulmonary arterioles and venules contribute to gas exchange at the alveoli?
What best summarizes the role of alveolar macrophages?
What best summarizes the role of alveolar macrophages?
What are the key components that facilitate gas exchange at the exchange surface of the alveoli?
What are the key components that facilitate gas exchange at the exchange surface of the alveoli?
How does the pleura contribute to effective lung function?
How does the pleura contribute to effective lung function?
Which of the following correctly describes the relationship between pressure and volume of a gas, as stated by Boyle's Law (assuming constant temperature and number of moles)?
Which of the following correctly describes the relationship between pressure and volume of a gas, as stated by Boyle's Law (assuming constant temperature and number of moles)?
In the context of respiratory physiology, what does a spirometer measure?
In the context of respiratory physiology, what does a spirometer measure?
How is Inspiratory Reserve Volume (IRV) defined?
How is Inspiratory Reserve Volume (IRV) defined?
What change in alveolar pressure results in inspiration?
What change in alveolar pressure results in inspiration?
How does intrapleural pressure change during inspiration, and why?
How does intrapleural pressure change during inspiration, and why?
What is the significance of the anatomical dead space in alveolar ventilation?
What is the significance of the anatomical dead space in alveolar ventilation?
How does the respiratory system respond when there is an increase in $PCO_2$ and a decrease in $PO_2$?
How does the respiratory system respond when there is an increase in $PCO_2$ and a decrease in $PO_2$?
Oxygen diffuses from the alveoli into the blood, and carbon dioxide diffuses from the blood into the alveoli. What drives this exchange?
Oxygen diffuses from the alveoli into the blood, and carbon dioxide diffuses from the blood into the alveoli. What drives this exchange?
What factors can influence gas exchange between alveoli and blood?
What factors can influence gas exchange between alveoli and blood?
What is the primary mechanism by which oxygen is transported in the blood?
What is the primary mechanism by which oxygen is transported in the blood?
What percentage of oxygen is transported in the blood on hemoglobin?
What percentage of oxygen is transported in the blood on hemoglobin?
What does a shift to the right on the oxygen-hemoglobin dissociation curve indicate?
What does a shift to the right on the oxygen-hemoglobin dissociation curve indicate?
Which of the following conditions causes a rightward shift (decreased affinity) on the oxygen-hemoglobin dissociation curve?
Which of the following conditions causes a rightward shift (decreased affinity) on the oxygen-hemoglobin dissociation curve?
What is the normal percentage of methaemoglobin, compared to total haemoglobin, in the blood?
What is the normal percentage of methaemoglobin, compared to total haemoglobin, in the blood?
What happens in the blood when carbon dioxide reacts with water?
What happens in the blood when carbon dioxide reacts with water?
What is the role of carbonic anhydrase in carbon dioxide transport?
What is the role of carbonic anhydrase in carbon dioxide transport?
Why is it important to remove carbon dioxide from the body?
Why is it important to remove carbon dioxide from the body?
What effect does acidosis have on the respiratory system?
What effect does acidosis have on the respiratory system?
Approximately what percentage of carbon dioxide is transported in the RBCs?
Approximately what percentage of carbon dioxide is transported in the RBCs?
What is the ‘chloride shift’ that occurs in red blood cells during carbon dioxide transport?
What is the ‘chloride shift’ that occurs in red blood cells during carbon dioxide transport?
What is the most significant factor to consider when assessing the lung capacity a patient should have
What is the most significant factor to consider when assessing the lung capacity a patient should have
Which lung disease involves decreased alveolar ventilation?
Which lung disease involves decreased alveolar ventilation?
Which lung pathology has a reduced capacity due to fibrosis
Which lung pathology has a reduced capacity due to fibrosis
When measuring lung capacity, what does FRC stand for?
When measuring lung capacity, what does FRC stand for?
During pulmonary gas exchange, what happens to the partial pressures of oxygen and carbon dioxide as blood flows through the pulmonary capillaries?
During pulmonary gas exchange, what happens to the partial pressures of oxygen and carbon dioxide as blood flows through the pulmonary capillaries?
What role does the mucociliary escalator play in the respiratory system?
What role does the mucociliary escalator play in the respiratory system?
What factors determine the effectiveness of alveolar ventilation?
What factors determine the effectiveness of alveolar ventilation?
According to Dalton's Law of Partial Pressures, if the partial pressures of nitrogen, oxygen, and carbon dioxide in a gas mixture are 597 mm Hg, 160 mm Hg, and 0.3 mm Hg respectively, what is the total pressure of the gas mixture?
According to Dalton's Law of Partial Pressures, if the partial pressures of nitrogen, oxygen, and carbon dioxide in a gas mixture are 597 mm Hg, 160 mm Hg, and 0.3 mm Hg respectively, what is the total pressure of the gas mixture?
How does the presence of surfactant affect the surface tension in the alveoli and what is the physiological consequence?
How does the presence of surfactant affect the surface tension in the alveoli and what is the physiological consequence?
What is the effect of increased levels of 2,3-diphosphoglycerate (2,3-DPG) on the oxygen-hemoglobin dissociation curve, and what does this indicate about oxygen affinity?
What is the effect of increased levels of 2,3-diphosphoglycerate (2,3-DPG) on the oxygen-hemoglobin dissociation curve, and what does this indicate about oxygen affinity?
During exercise, several factors change in the body. Which combination of these changes would lead to increased oxygen unloading from hemoglobin to tissues?
During exercise, several factors change in the body. Which combination of these changes would lead to increased oxygen unloading from hemoglobin to tissues?
Why is carbon dioxide able to diffuse more readily across the alveolar-capillary membrane compared to oxygen, despite having a similar partial pressure gradient?
Why is carbon dioxide able to diffuse more readily across the alveolar-capillary membrane compared to oxygen, despite having a similar partial pressure gradient?
If a patient has a tidal volume of 500 mL and a respiratory rate of 12 breaths per minute, and their anatomical dead space is estimated to be 150 mL, what is their approximate alveolar ventilation?
If a patient has a tidal volume of 500 mL and a respiratory rate of 12 breaths per minute, and their anatomical dead space is estimated to be 150 mL, what is their approximate alveolar ventilation?
In the context of carbon dioxide transport, what is the 'chloride shift' and why does it occur?
In the context of carbon dioxide transport, what is the 'chloride shift' and why does it occur?
What is the functional role of the pleura and pleural fluid in respiration?
What is the functional role of the pleura and pleural fluid in respiration?
Which of the following mechanisms explains how high carbon dioxide levels can lead to problems with nervous system function?
Which of the following mechanisms explains how high carbon dioxide levels can lead to problems with nervous system function?
Under normal physiological conditions, intrapleural pressure is always lower than alveolar pressure. Why is this pressure gradient important?
Under normal physiological conditions, intrapleural pressure is always lower than alveolar pressure. Why is this pressure gradient important?
Which of the following factors does NOT directly influence the rate of gas exchange between the alveoli and the blood?
Which of the following factors does NOT directly influence the rate of gas exchange between the alveoli and the blood?
A patient presents with cyanosis and blood tests reveal a higher-than-normal level of methemoglobin. How does methemoglobin affect oxygen transport?
A patient presents with cyanosis and blood tests reveal a higher-than-normal level of methemoglobin. How does methemoglobin affect oxygen transport?
Flashcards
Respiratory System's Gas Exchange
Respiratory System's Gas Exchange
Exchange of oxygen and carbon dioxide between air and blood.
Respiratory System's pH Balance
Respiratory System's pH Balance
Maintaining a stable pH level within the body.
Respiratory System's Protection
Respiratory System's Protection
The respiratory system protects against harmful substances through mechanisms like mucus and cilia.
Respiratory System's Vocalisation
Respiratory System's Vocalisation
Signup and view all the flashcards
Upper Respiratory Tract Components
Upper Respiratory Tract Components
Signup and view all the flashcards
Upper Respiratory Tract's Air Preparation
Upper Respiratory Tract's Air Preparation
Signup and view all the flashcards
Lower Respiratory Tract Components
Lower Respiratory Tract Components
Signup and view all the flashcards
Thoracic Cage
Thoracic Cage
Signup and view all the flashcards
Conducting system vs. exchange surface
Conducting system vs. exchange surface
Signup and view all the flashcards
Alveoli's Function
Alveoli's Function
Signup and view all the flashcards
Alveolar Cells Types
Alveolar Cells Types
Signup and view all the flashcards
Alveoli Exchange Surface Structure
Alveoli Exchange Surface Structure
Signup and view all the flashcards
Pleura
Pleura
Signup and view all the flashcards
Ideal Gas Law in the Body
Ideal Gas Law in the Body
Signup and view all the flashcards
Boyle's Law
Boyle's Law
Signup and view all the flashcards
Dalton's Law of Partial Pressures
Dalton's Law of Partial Pressures
Signup and view all the flashcards
Spirometer
Spirometer
Signup and view all the flashcards
The pressures of Inspiration and Expiration
The pressures of Inspiration and Expiration
Signup and view all the flashcards
Thoracic Cage Movement During Breathing
Thoracic Cage Movement During Breathing
Signup and view all the flashcards
Intrapulmonary pressure
Intrapulmonary pressure
Signup and view all the flashcards
Intrapleural pressure
Intrapleural pressure
Signup and view all the flashcards
Tidal Volume
Tidal Volume
Signup and view all the flashcards
Intrapleural Pressure
Intrapleural Pressure
Signup and view all the flashcards
Anatomical Dead Space
Anatomical Dead Space
Signup and view all the flashcards
Ventilation-Perfusion Coupling
Ventilation-Perfusion Coupling
Signup and view all the flashcards
Gas Movement
Gas Movement
Signup and view all the flashcards
Oxygen in the Blood
Oxygen in the Blood
Signup and view all the flashcards
Influences on Gas Exchange
Influences on Gas Exchange
Signup and view all the flashcards
Oxygen Mass Balance
Oxygen Mass Balance
Signup and view all the flashcards
CO2 vs O2 Content
CO2 vs O2 Content
Signup and view all the flashcards
O2 Transport
O2 Transport
Signup and view all the flashcards
Bound Oxygen Fraction
Bound Oxygen Fraction
Signup and view all the flashcards
Oxygen-haemoglobin binding curve
Oxygen-haemoglobin binding curve
Signup and view all the flashcards
Methaemoglobin
Methaemoglobin
Signup and view all the flashcards
Forms of Carbon Dioxide
Forms of Carbon Dioxide
Signup and view all the flashcards
Consequences of Untreated CO2
Consequences of Untreated CO2
Signup and view all the flashcards
Understanding Oxygenation
Understanding Oxygenation
Signup and view all the flashcards
Lung capacity normal values
Lung capacity normal values
Signup and view all the flashcards
What diseases change lung function?
What diseases change lung function?
Signup and view all the flashcards
VC
VC
Signup and view all the flashcards
IRV
IRV
Signup and view all the flashcards
ERV
ERV
Signup and view all the flashcards
FRC
FRC
Signup and view all the flashcards
RV
RV
Signup and view all the flashcards
Study Notes
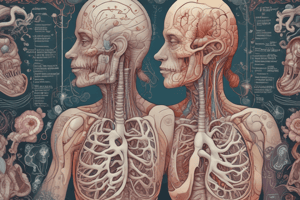
- The main functions of the respiratory system include exchanging O2 and CO2 between air and blood, keeping body pH stable, protecting from harmful substances, and vocalisation.
- The functional anatomy of the respiratory system consists of the upper and lower respiratory tracts.
Upper Respiratory Tract
- The upper respiratory tract includes the mouth, nasal cavity, pharynx, and larynx which warms, wets, and filters air.
- The particles trapped by the filtering action in the upper respiratory tract are either swallowed, spat out, or expelled through sneezing.
Lower Respiratory Tract
- The lower respiratory tract consists of the trachea, two primary bronchi, branches of bronchi (22 divisions) i.e. bronchioles, and the lungs.
- The thoracic cage, which surrounds the respiratory system, comprises bones and muscles, including the sternum, ribs, diaphragm, and intercostal muscles.
Airways and Alveoli
- The respiratory system includes a conducting system and an exchange surface.
- The conducting system consists of the trachea, primary bronchi, and smaller bronchi, all the way down to the bronchioles.
- The trachea divides into 2 primary bronchi.
- The trachea has a diameter of 15-22 mm, with one of them and a cross-sectional area of 2.5 cm.
- The primary bronchi have a diameter of 10-15 mm and there are 2 of them.
- The smaller bronchi go trhough 22 divisions.
- The exchange surface consists of bronchioles and alveoli.
- The bronchioles have a diameter of 0.5 - 1mm.
- The exchange surface consists of alveoli, where gas exchange with the blood occurs, and there are 3-6 X 10^8 of them.
- The exchange of the alveoli has a a diameter of 0.3 mm and an area of >1 X 10^6 cm.
Alveolar Structures
- Pulmonary venules carry high O2.
- Pulmonary arterioles carry low O2.
Alveolar Cells
- Alveolar fluid lining contains pulmonary surfactant.
- Other structures in the alveoli include alveolar macrophage, alveolar cells type I and II, erythrocytes and pulmonary capillaries
Exchange Surface of the Alveoli
- The alveolar exchange surface contains a thin layer of alveolar epithelium, endothelium, surfactant, and fused basement membranes.
- It's imperative that this layer be thin otherwise gas exchange will be compromised
Pleura
- The pleura consists of a double-walled closed sac separating each lung from the thoracic wall where the parietal pleura is attached to the thoracic cage wall.
- The visceral pleura is attached to the lungs.
- The space between the pleural membranes contains pleural fluid, which keeps the membranes together and provides lubrication.
Gas Laws
- Boyle's Law describes the inverse relationship between pressure and volume of a gas in a system: P1V1 = P2V2
- Dalton’s law of partial pressures explains that an increase in pressure of one gas, will increase total pressure
- In the human body, it can be assumed that 'n' (number of moles) and 'T' (temperature) are constant, therefore V (volume) = 1/P.
Pulmonary Function Test
- Pulmonary function tests use a spirometer to measure lung volumes and capacities.
- Lung volumes and capacities include inspiratory reserve volume (IRV), tidal volume (VT), expiratory reserve volume (ERV), and residual volume.
Lung Capacities
- Total lung capacity measurement in males is 6000 ml, while in females it is 4200 ml.
- Functional residual capacity is 700ml.
Mechanics of Ventilation
- Inspiration and expiration depend on changes in intrapulmonary or alveolar pressure.
- Intrapleural pressure needs to be lower than atmospheric pressure for optimal breathing.
- During inspiration, volume increases, causing air to flow in. During expiration, volume decreases, causing air to flow out.
- During breathing in the chest expands, the ribs go up and the diaphragm contracts, while during breathing out, the chest contracts, the ribs move downward and the diaphragm relaxes.
Pressure Types in Respiration
- During each breath, pressure gradients move 0.5 liter of air into and out of the lungs.
- Intrapulmonary pressure inside the lung decreases during inspiration and increases during expiration.
- Intrapleural pressure in the pleural cavity becomes more negative as the chest wall expands during inspiration.
- Atmospheric pressure needs to be higher than alveolar pressure.
Anatomical Dead Space
- Anatomical dead space must be taken into account to determine determining alveolar ventilation. It is calculated by subtracting the number of breaths per minute from 500–150 ml per breath.
Ventilation
- Ventilation and perfusion are matched to ensure efficient gas exchange.
- Gas exchange occurs via diffusion.
- Air composition, ventilation properties such as resistance, perfusion, and diffusion properties between alveoli and blood influence gas exchange.
Gas Exchange
- Influences on gas exchange between alveoli and blood include air composition, ventilation properties like resistance, perfusion, and the properties of diffusion between alveoli and blood.
- Oxygen enters the blood at the alveolar-capillary interface and is transported in blood dissolved in plasma, or bound to hemoglobin inside RBCs, then oxygen diffuses into cells.
- CO2 diffuses out of cells and is transported dissolved, bound to hemoglobin, or as HCO3, then CO2 enters alveoli at the alveolar-capillary interface.
- In venous blood pO2 levels should be equal to or less than 40 mm Hg. pCO2 levels should be higher or equal to 46 mm Hg.
Pathological Conditions
- Pathological conditions causing hypoxia include asthma (decreased alveolar ventilation), pulmonary edema (fluid in the interstitial space), and emphysema (less surface area due to destruction of alveoli).
Mass Balance and Flow of Oxygen
- Arterial O2 transport minus venous O2 transport equals cell use of O2.
- O2 transport equals cardiac output (CO) X O2 concentration.
- Hence, CO X (Arterial [O2] - Venous [O2]) equals cell use of O2.
- Arterial transport: Hb+O2 > 98%; Dissolved O2 2
- O2 content is less than CO2, even in arterial blood where PaO2 is 100 mm Hg and PaCO2 is 40 mm Hg.
- Normally around 1% of total haemoglobin.
- High methaemoglobin levels in the blood can cause cyanosis
Blood Gas Transport
- Approximately 98% of blood O2 is delivered to tissues bound to haemoglobin.
- CO2 reacts with H2O to form H2CO3 (carbonic acid), then HCO3- (bicarbonate) + H+.
- If CO2 is not removed, pH disturbances (acidosis) occurs, as well as protein denaturation and nervous system dysfunction.
- In venous blood, CO2 70% load turns into bicarbonate.
- At the lungs ,CO2 unbinds and returns to HCO3, and turns into H2O and CO2 to be exhaled.
- Oxygenation of the blood results in CO2 being removed from the blood, and if PaCO2 = 0, there is no CO2 in the blood.
Lung Characteristics
- Factors that might affect lung parameter are Age, Height and Gender
- Diseases that might affect lung function includes COPD, Bronchitis, Asthma, Infections like Pneumonia, Emphysema, Fibrosis, and Silicosis.
- Vital Capacity is the maximal volume that can be expired after a maximal inspiration.
- Inspiratory Reserve Volume (IRV) is the maximal volume which can be inspired from end-tidal inspiration.
- Expiratory Reserve Volume (ERV) is the maximal volume which can be expired from the resting end-expiratory level.
- Inspiratory Capacity is the maximal volume which can be inspired from the resting end-expiratory level.
- Functional Residual Capacity (FRC) is the volume of gas in the lungs at the resting end-expiratory level.
- Residual Volume is the volume of gas in the lungs at the end of maximal expiration.
- Total Lung Capacity is the volume of gas in the lungs at the end of a maximal inspiration.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.