Podcast
Questions and Answers
What is external respiration primarily concerned with?
What is external respiration primarily concerned with?
- The regulation of breathing rates in response to carbon dioxide levels
- The exchange of gases between the environment and body cells (correct)
- The transport of oxygen solely in the bloodstream
- The intracellular use of oxygen and carbon dioxide production
Which step is NOT part of the process of external respiration?
Which step is NOT part of the process of external respiration?
- Pulmonary ventilation
- Transport of gases in systemic circulation
- Internal metabolic processes in mitochondria (correct)
- Gas exchange between alveoli and blood
What occurs during pulmonary ventilation?
What occurs during pulmonary ventilation?
- Conversion of oxygen to carbon dioxide in cells
- Transport of nutrients to the cells by the blood
- Gas exchange between the blood and tissue cells
- Movement of air in and out of the alveoli (correct)
What is involved in the transport of gases during external respiration?
What is involved in the transport of gases during external respiration?
Which of the following best defines internal respiration?
Which of the following best defines internal respiration?
What is the role of systemic circulation in respiration?
What is the role of systemic circulation in respiration?
What are the two main phases of breathing known as?
What are the two main phases of breathing known as?
Which factor increases the diffusion rate of gas through the alveolar membrane?
Which factor increases the diffusion rate of gas through the alveolar membrane?
How does pulmonary edema affect gas exchange?
How does pulmonary edema affect gas exchange?
Which of the following structures is NOT part of the upper respiratory system?
Which of the following structures is NOT part of the upper respiratory system?
What causes air to flow into and out of the lungs during respiration?
What causes air to flow into and out of the lungs during respiration?
What condition is characterized by damaged alveolar walls that reduce gas exchange?
What condition is characterized by damaged alveolar walls that reduce gas exchange?
Which of the following respiratory muscles is primarily responsible for inhalation?
Which of the following respiratory muscles is primarily responsible for inhalation?
What role does the diaphragm play during breathing?
What role does the diaphragm play during breathing?
What type of hypoxia is associated with microcytic hypochromic anemia?
What type of hypoxia is associated with microcytic hypochromic anemia?
Which of the following is a likely arterial pressure of oxygen in the child with anemic hypoxia?
Which of the following is a likely arterial pressure of oxygen in the child with anemic hypoxia?
What dietary change did the nutritionist recommend for the child?
What dietary change did the nutritionist recommend for the child?
What is the expected effect on circulating red blood cells with anemic hypoxia?
What is the expected effect on circulating red blood cells with anemic hypoxia?
Why might the child experience lethargy and fatigue?
Why might the child experience lethargy and fatigue?
What is the normal arterial pressure of carbon dioxide expected in the child?
What is the normal arterial pressure of carbon dioxide expected in the child?
What is the effect of lung fibrosis on gas exchange?
What is the effect of lung fibrosis on gas exchange?
How is oxygen primarily transported in the blood?
How is oxygen primarily transported in the blood?
Which type of hypoxia is characterized by insufficient oxygen at the cellular level?
Which type of hypoxia is characterized by insufficient oxygen at the cellular level?
What percentage of carbon dioxide is transported in the blood as bicarbonate?
What percentage of carbon dioxide is transported in the blood as bicarbonate?
In the context of the case scenario, what would likely be observed in the blood gas analysis of the child experiencing hypoxic hypoxia?
In the context of the case scenario, what would likely be observed in the blood gas analysis of the child experiencing hypoxic hypoxia?
What would be the likely effect of bronchial asthma on hemoglobin saturation during an asthma attack?
What would be the likely effect of bronchial asthma on hemoglobin saturation during an asthma attack?
What condition occurs when there is inadequate Hb saturation despite normal arterial PO2 levels?
What condition occurs when there is inadequate Hb saturation despite normal arterial PO2 levels?
Which factor is NOT associated with tissue oxygenation?
Which factor is NOT associated with tissue oxygenation?
What kind of hypoxia results from poisoning where cells cannot use oxygen efficiently?
What kind of hypoxia results from poisoning where cells cannot use oxygen efficiently?
In a scenario where a child is exposed to high altitude, what is the primary type of hypoxia expected?
In a scenario where a child is exposed to high altitude, what is the primary type of hypoxia expected?
Flashcards
External Respiration
External Respiration
The entire process of gas exchange between the outside environment and the body's cells.
Pulmonary Ventilation
Pulmonary Ventilation
The movement of air into and out of the lungs.
Gas Exchange (Alveoli)
Gas Exchange (Alveoli)
Oxygen enters the blood, and carbon dioxide leaves the blood in the alveoli.
Respiratory System
Respiratory System
Signup and view all the flashcards
Internal Respiration
Internal Respiration
Signup and view all the flashcards
Respiration
Respiration
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Gas Exchange
Gas Exchange
Signup and view all the flashcards
Diffusion Rate
Diffusion Rate
Signup and view all the flashcards
Pulmonary Edema
Pulmonary Edema
Signup and view all the flashcards
Emphysema
Emphysema
Signup and view all the flashcards
Anemic Hypoxia
Anemic Hypoxia
Signup and view all the flashcards
Cause of Lethargy in Anemic Hypoxia
Cause of Lethargy in Anemic Hypoxia
Signup and view all the flashcards
Microcytic Hypochromic Anemia
Microcytic Hypochromic Anemia
Signup and view all the flashcards
Dietary Intervention for Microcytic Anemia
Dietary Intervention for Microcytic Anemia
Signup and view all the flashcards
PO2 in Anemic Hypoxia
PO2 in Anemic Hypoxia
Signup and view all the flashcards
Impact on RBC Count in Anemic Hypoxia
Impact on RBC Count in Anemic Hypoxia
Signup and view all the flashcards
Lung fibrosis
Lung fibrosis
Signup and view all the flashcards
O2 transport
O2 transport
Signup and view all the flashcards
CO2 transport
CO2 transport
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Hypoxic hypoxia
Hypoxic hypoxia
Signup and view all the flashcards
Histotoxic hypoxia
Histotoxic hypoxia
Signup and view all the flashcards
Status asthmaticus
Status asthmaticus
Signup and view all the flashcards
Blood gas analysis
Blood gas analysis
Signup and view all the flashcards
Study Notes
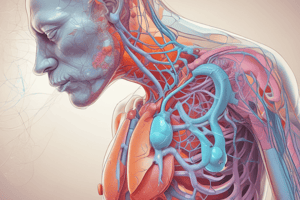
Respiratory Physiology
- Focuses on respiration, encompassing the definition, types, gas exchange and transport, and hypoxia.
- Textbook: Sherwood, L. (2015). Human physiology: from cells to systems. Cengage Learning. Chapter 13
- Respiration: Obtaining oxygen for bodily functions and eliminating carbon dioxide.
What is Respiration?
- Process of acquiring oxygen for the body and expelling produced carbon dioxide.
Internal vs. External Respiration
- Internal respiration: Intracellular metabolic processes in mitochondria (using O2 and producing CO2).
- External respiration: Full sequence of gas exchange between environment and body cells. Consists of 4 steps.
External Respiration Steps
- Pulmonary ventilation (inhaling and exhaling air between atmosphere and alveoli).
- Gas exchange (between air in alveoli and blood in pulmonary capillaries).
- Transport of gases (in the blood between lungs and tissues).
- Exchange of gases (between blood in systematic capillaries and tissues).
Respiratory System Structure
- Air-conducting parts: Nasal cavity, pharynx, vocal cords, esophagus, larynx, trachea, bronchus.
- Gas exchange zone (alveoli): Terminal bronchioles, alveolar sacs (alveoli) with thin walls.
Mechanisms of Pulmonary Ventilation
- Inhalation: Rib muscles contract, expanding the rib cage. Diaphragm contracts, pulling it down.
- Exhalation: Rib muscles relax, contracting the rib cage, diaphragm relaxes, moving up.
Breathing Phases
- Inspiration: Air flows into the lungs.
- Expiration: Gases exit the lungs.
Muscles of Respiration
- Rib muscles: Expand or contract rib cage, changing the thoracic cavity, influencing air pressure.
- Diaphragm: Contracts down or relaxes up to alter volume in the thoracic cavity.
Factors Affecting Gas Exchange
- Diffusion rate through alveolar membrane is impacted by membrane thickness, surface area, gas solubility, and pressure difference.
Factors Affecting Diffusion through Respiratory Membrane
- Pulmonary edema: Increased thickness of membrane, decreasing gas exchange.
- Emphysema: Damage to alveolar walls, reducing surface area and gas exchange.
- Lung fibrosis: Increased thickness of respiratory membrane, decreasing gas exchange.
Normal Partial Pressures of Oxygen and Carbon Dioxide
- Alveoli oxygen (PO2): 100 mmHg
- Alveoli carbon dioxide (PCO2): 40 mmHg
- Circulatory oxygen (PO2): Lower than alveoli
- Circulatory carbon dioxide (PCO2): Higher than alveoli
- Peripheral tissue oxygen (PO2): Lower than circulatory
- Peripheral tissue carbon dioxide (PCO2): Higher than circulatory
Oxygen Transport in the Blood
- Dissolved in plasma: 1.5%
- Bound to hemoglobin: 98.5%
Carbon Dioxide Transport in the Blood
- Physically dissolved: 10%
- Bound to hemoglobin: 30%
- As bicarbonate: 60%
Hypoxemia
- Insufficient oxygen at cellular level.
Types of Hypoxia
- Hypoxic Hypoxia: Decreased oxygen delivered to the tissues.
- Causes: Respiratory malfunction, high altitude.
- Characteristics: Decreased PO2, Decreased O2 content
- Anemic Hypoxia: Decreased oxygen-carrying capacity in the blood.
- Causes: Low red blood cells, Hemoglobin abnormalities (e.g., CO poisoning).
- Characteristics: Normal PO2, Decreased O2 content
- Circulatory Hypoxia: Inadequate blood flow to the tissues.
- Causes: Congestive heart failure, circulatory shock.
- Characteristics: Normal PO2, Normal O2 content
- Histotoxic Hypoxia: Cells unable to use oxygen.
- Causes: Cyanide poisoning.
- Characteristics: Normal PO2, Normal O2 content
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.