Podcast
Questions and Answers
What is the correct method to calculate Functional Residual Capacity (FRC)?
What is the correct method to calculate Functional Residual Capacity (FRC)?
- Add the volume indicated by 'F' (correct)
- Subtract the volume indicated by 'F'
- Subtract the volume indicated by 'E'
- Add the volume indicated by 'E'
What does Intrapleural Pressure (IPP) represent?
What does Intrapleural Pressure (IPP) represent?
- Pressure between visceral and parietal pleura (correct)
- Pressure exerted by external atmosphere
- Pressure within the chest cavity only
- Pressure inside lung alveoli
At Functional Residual Capacity (FRC), what is the state of Transpulmonary Pressure Gradient (Ptm)?
At Functional Residual Capacity (FRC), what is the state of Transpulmonary Pressure Gradient (Ptm)?
- Always positive (correct)
- Varies randomly
- Always zero
- Always negative
Which statement best describes compliance within the lungs?
Which statement best describes compliance within the lungs?
In the event of a tension pneumothorax, what happens to Intrapleural Pressure (IPP)?
In the event of a tension pneumothorax, what happens to Intrapleural Pressure (IPP)?
How is Transpulmonary Pressure Gradient (Ptm) mathematically defined?
How is Transpulmonary Pressure Gradient (Ptm) mathematically defined?
What primarily influences lung elasticity during respiration?
What primarily influences lung elasticity during respiration?
What characterizes lungs with high compliance?
What characterizes lungs with high compliance?
Which of the following statements about elasticity and compliance in the lungs is true?
Which of the following statements about elasticity and compliance in the lungs is true?
What is the formula for calculating transpulmonary pressure?
What is the formula for calculating transpulmonary pressure?
Which pressure gradient affects the volume of the thoracic cavity during respiration?
Which pressure gradient affects the volume of the thoracic cavity during respiration?
What is the partial pressure of oxygen in alveolar air (PAO2)?
What is the partial pressure of oxygen in alveolar air (PAO2)?
How does a decrease in volume due to muscle relaxation affect intra-alveolar pressure?
How does a decrease in volume due to muscle relaxation affect intra-alveolar pressure?
What is the effect of humidifying inspired air on gas partial pressures?
What is the effect of humidifying inspired air on gas partial pressures?
What is the typical value for intra-pleural pressure at rest?
What is the typical value for intra-pleural pressure at rest?
Which of the following correctly defines partial pressure?
Which of the following correctly defines partial pressure?
What is the respiratory pressure gradient that exists between intra-alveolar pressure and atmospheric pressure called?
What is the respiratory pressure gradient that exists between intra-alveolar pressure and atmospheric pressure called?
Which value represents the partial pressure of carbon dioxide in the alveoli?
Which value represents the partial pressure of carbon dioxide in the alveoli?
What gas exchange process occurs in the alveoli?
What gas exchange process occurs in the alveoli?
What is the effect of loop diuretics on electrolyte levels in the filtrate?
What is the effect of loop diuretics on electrolyte levels in the filtrate?
In which part of the nephron does the renal tubular fluid first become hypoosmotic to plasma?
In which part of the nephron does the renal tubular fluid first become hypoosmotic to plasma?
What happens to the tubular fluid in the thick ascending loop of Henle?
What happens to the tubular fluid in the thick ascending loop of Henle?
How do NKCC2 transporters affect water reabsorption in the collecting ducts?
How do NKCC2 transporters affect water reabsorption in the collecting ducts?
What is the role of potassium ions (K+) in the thick ascending limb of the Loop of Henle?
What is the role of potassium ions (K+) in the thick ascending limb of the Loop of Henle?
What is the primary function of the thick ascending limb of the Loop of Henle?
What is the primary function of the thick ascending limb of the Loop of Henle?
What happens to pleural pressure during inspiration?
What happens to pleural pressure during inspiration?
Which statement is true regarding alveolar pressure when air is being inhaled?
Which statement is true regarding alveolar pressure when air is being inhaled?
If the intrapleural pressure is measured at 760 mm Hg, what can be inferred about the atmospheric conditions?
If the intrapleural pressure is measured at 760 mm Hg, what can be inferred about the atmospheric conditions?
What determines the partial pressure of a gas in a mixture according to the gas laws?
What determines the partial pressure of a gas in a mixture according to the gas laws?
In the context of gas exchange, what is true for a gas with a higher partial pressure in the alveoli?
In the context of gas exchange, what is true for a gas with a higher partial pressure in the alveoli?
Which value of alveolar pressure would result in air flowing into the lungs?
Which value of alveolar pressure would result in air flowing into the lungs?
What effect does humidifying inspired air have on gas partial pressures?
What effect does humidifying inspired air have on gas partial pressures?
What is the partial pressure of oxygen (PO2) in the inspired air at sea level?
What is the partial pressure of oxygen (PO2) in the inspired air at sea level?
Which factor does NOT influence energy expenditure during ventilation?
Which factor does NOT influence energy expenditure during ventilation?
When the total energy expenditure increases during quiet breathing, which factor is most likely at play?
When the total energy expenditure increases during quiet breathing, which factor is most likely at play?
What is the primary component of the glomerular exchange pathway that results in a protein-free filtrate?
What is the primary component of the glomerular exchange pathway that results in a protein-free filtrate?
In nephrotic syndrome, the loss of negative charges from the filtration barrier primarily affects which of the following components?
In nephrotic syndrome, the loss of negative charges from the filtration barrier primarily affects which of the following components?
What condition is often referred to as minimal change disease in children?
What condition is often referred to as minimal change disease in children?
Which factor has the most significant impact on the Glomerular Filtration Rate (GFR)?
Which factor has the most significant impact on the Glomerular Filtration Rate (GFR)?
What clinical sign indicates a loss of plasma oncotic pressure in nephrotic syndrome?
What clinical sign indicates a loss of plasma oncotic pressure in nephrotic syndrome?
What role does sympathetic control play in kidney function during dehydration?
What role does sympathetic control play in kidney function during dehydration?
Which mechanism primarily regulates the radius of the afferent arteriole to control glomerular blood flow?
Which mechanism primarily regulates the radius of the afferent arteriole to control glomerular blood flow?
Which of the following is NOT a component of the filtration system that a particle must pass through?
Which of the following is NOT a component of the filtration system that a particle must pass through?
How is sodium excretion affected by changes in GFR?
How is sodium excretion affected by changes in GFR?
What is the most common indicator of severe protein loss in nephrotic syndrome?
What is the most common indicator of severe protein loss in nephrotic syndrome?
Flashcards are hidden until you start studying
Study Notes
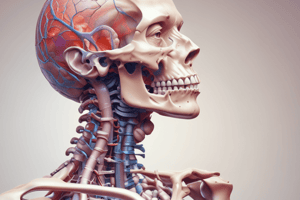
FRC (Functional Residual Capacity)
- FRC represents the volume of air remaining in the lungs after a normal exhale.
Intrapleural Pressure (IPP)
- IPP refers to the pressure within the thin fluid layer between the visceral pleura (attached to the lung) and the parietal pleura (attached to the chest wall).
- The outward recoil of the chest wall and the inward recoil of the lung create a negative (subatmospheric) IPP.
Transpulmonary Pressure (Transmural) Pressure Gradient (Ptm)
- Ptm = Pinside – Poutside
- Ptm is positive at FRC because IPP is subatmospheric.
- The positive outward force counteracts the lung's elastic recoil, preventing alveolar collapse.
Transpulmonary Pressure Gradient Pathology
-
Traumatic pneumothorax: Perforation of the chest wall allows air to enter the pleural space (PP), increasing IPP and creating a negative TMP. This leads to lung collapse and chest wall expansion on the affected side.
-
Tension pneumothorax: Air enters the PP space from damaged alveoli, increasing IPP and producing a negative TMP. The increased pressure can cause tracheal deviation and is a serious condition, particularly in patients on positive-pressure ventilation.
Compliance and Elasticity
- Compliance: Indicates the amount of effort needed to stretch or distend the lungs. Lower compliance (stiffer lungs) requires more effort to inflate.
- Elasticity: The force that drives the lungs to return to their original shape.
- Compliance is crucial for inspiration, while elasticity is important for expiration.
- Lung compliance varies with volume; it's easier to inflate at smaller volumes but becomes harder as the volume increases.
Components of Lung Recoil
- Elastic recoil (caused by three factors) drives lung collapse:
- Elastic recoil of the chest and lung: The primary contributor to lung recoil.
- Frictional resistance to gas flow in the airways: Airflow resistance within the airways.
- Tissue frictional resistance: Resistance caused by the movement of lung tissue.
Inspiration
- Pleural pressure is more negative during inspiration than at FRC.
- Alveolar pressure is lower than atmospheric pressure during inspiration.
Intrapleural Pressure (IPP)
- If IPP is 760 mm Hg, it indicates atmospheric pressure and the lung is not actively breathing.
Alveolar Ventilation
- The process of exchanging oxygen (O2) and carbon dioxide (CO2) between the alveoli of the lungs and the external environment.
Gas Partial Pressure
- Gas exchange relies on the simple diffusion of O2 and CO2 down partial pressure gradients.
- Partial pressure is calculated by multiplying the pressure exerted on the gas by its percentage in the mixture.
PO2: Atmospheric and Inspired Air
- PatmO2 = 0.21(760) = 160 mm Hg (Atmospheric oxygen partial pressure)
- Inspired air is warmed to 37°C and humidified.
- Humidification reduces the partial pressure of other gases.
Transpulmonary Pressure
- The difference in pressure between the inside and outside of a compartment.
- At FRC:
- Transpulmonary Pressure = Intra-alveolar Pressure – Intra-pleural Pressure
- Transthoracic Pressure = Intra-pleural Pressure – Atmospheric Pressure
- Transrespiratory Pressure = Intra-alveolar Pressure – Atmospheric Pressure
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.