Podcast
Questions and Answers
What is the role of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
What is the role of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
- To regulate the stretch receptors in the lungs
- To sense changes in oxygen and carbon dioxide levels in the blood (correct)
- To control the movement of the diaphragm and intercostal muscles
- To modulate the elasticity of the thorax
What is the reason for measuring pressures driving respiratory airflow in cm H2O rather than mm Hg?
What is the reason for measuring pressures driving respiratory airflow in cm H2O rather than mm Hg?
- To ensure accurate measurement of pressure changes in the lungs
- To avoid confusion with other pressure measurements in the body (correct)
- To reflect the compressibility of air in the respiratory system
- To account for the resistance offered by the alveoli during expiration
How does intrapulmonary pressure change relative to atmospheric pressure during inspiration?
How does intrapulmonary pressure change relative to atmospheric pressure during inspiration?
- It fluctuates rapidly during inspiration
- It remains constant throughout inspiration
- It increases to a level higher than atmospheric pressure
- It decreases to a level lower than atmospheric pressure (correct)
What is the role of elastic recoil of the thorax in expiration?
What is the role of elastic recoil of the thorax in expiration?
How does pulmonary ventilation get affected by bronchodilation?
How does pulmonary ventilation get affected by bronchodilation?
What is the difference between restrictive and obstructive disorders of respiration?
What is the difference between restrictive and obstructive disorders of respiration?
What is the definition of eupnea?
What is the definition of eupnea?
How is minute respiratory volume calculated?
How is minute respiratory volume calculated?
What does Kussmaul respiration refer to?
What does Kussmaul respiration refer to?
What is the role of the sternum and rib cage during the respiratory cycle?
What is the role of the sternum and rib cage during the respiratory cycle?
How does pulmonary ventilation get affected by bronchoconstriction?
How does pulmonary ventilation get affected by bronchoconstriction?
What is the neural pathway for voluntary control of respiration?
What is the neural pathway for voluntary control of respiration?
Why are the pressures driving respiratory airflow measured in cm H2O rather than mm Hg like other pressures?
Why are the pressures driving respiratory airflow measured in cm H2O rather than mm Hg like other pressures?
What is the relationship of airflow, pressure, and resistance in the context of pulmonary ventilation?
What is the relationship of airflow, pressure, and resistance in the context of pulmonary ventilation?
What is the effect of alveolar surfactant on pulmonary ventilation?
What is the effect of alveolar surfactant on pulmonary ventilation?
How does intrapulmonary pressure change relative to atmospheric pressure in expiration?
How does intrapulmonary pressure change relative to atmospheric pressure in expiration?
What is the typical adult tidal volume, and how much of this ventilates the alveoli?
What is the typical adult tidal volume, and how much of this ventilates the alveoli?
What are the locations and functions of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
What are the locations and functions of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
How does dyspnea differ from hyperpnea?
How does dyspnea differ from hyperpnea?
What is the mathematical relationship between airflow, pressure, and resistance in the context of pulmonary ventilation?
What is the mathematical relationship between airflow, pressure, and resistance in the context of pulmonary ventilation?
What does intrapulmonary pressure do relative to atmospheric pressure during expiration?
What does intrapulmonary pressure do relative to atmospheric pressure during expiration?
What is the role of the sternum and rib cage during the respiratory cycle?
What is the role of the sternum and rib cage during the respiratory cycle?
How are the pressures driving respiratory airflow measured, and why in this manner?
How are the pressures driving respiratory airflow measured, and why in this manner?
What is the difference between restrictive and obstructive disorders of respiration?
What is the difference between restrictive and obstructive disorders of respiration?
How does pulmonary ventilation get affected by bronchoconstriction?
How does pulmonary ventilation get affected by bronchoconstriction?
What is the neural pathway for voluntary control of respiration in humans?
What is the neural pathway for voluntary control of respiration in humans?
How does dyspnea differ from hyperpnea?
How does dyspnea differ from hyperpnea?
How does intrapulmonary pressure change relative to atmospheric pressure during inspiration?
How does intrapulmonary pressure change relative to atmospheric pressure during inspiration?
What is the role of elastic recoil of the thorax in expiration?
What is the role of elastic recoil of the thorax in expiration?
How does pulmonary ventilation get affected by bronchodilation?
How does pulmonary ventilation get affected by bronchodilation?
What are the locations and roles of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
What are the locations and roles of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
What is the role of the sternum and rib cage during the respiratory cycle?
What is the role of the sternum and rib cage during the respiratory cycle?
How and why does intrapulmonary pressure change relative to atmospheric pressure in expiration?
How and why does intrapulmonary pressure change relative to atmospheric pressure in expiration?
What is the impact of bronchodilation on pulmonary ventilation?
What is the impact of bronchodilation on pulmonary ventilation?
What is the mathematical relationship among airflow, pressure, and resistance in the context of pulmonary ventilation?
What is the mathematical relationship among airflow, pressure, and resistance in the context of pulmonary ventilation?
What is the difference between restrictive and obstructive disorders of respiration?
What is the difference between restrictive and obstructive disorders of respiration?
What is the primary role of elastic recoil of the thorax in expiration?
What is the primary role of elastic recoil of the thorax in expiration?
What are the locations and functions of the brainstem respiratory centers?
What are the locations and functions of the brainstem respiratory centers?
How does alveolar surfactant affect pulmonary ventilation?
How does alveolar surfactant affect pulmonary ventilation?
What is the reason for measuring pressures driving respiratory airflow in cm H2O rather than mm Hg?
What is the reason for measuring pressures driving respiratory airflow in cm H2O rather than mm Hg?
What is the neural pathway for voluntary control of respiration?
What is the neural pathway for voluntary control of respiration?
What are the locations and roles of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
What are the locations and roles of the central and peripheral chemoreceptors in modulating the respiratory rhythm?
Flashcards are hidden until you start studying
Study Notes
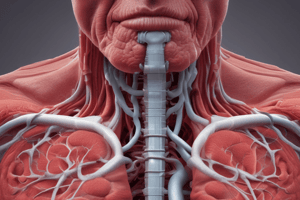
Respiratory System
- The central and peripheral chemoreceptors play a crucial role in modulating the respiratory rhythm by detecting changes in CO2 levels and pH.
Respiratory Pressures
- Pressures driving respiratory airflow are measured in cm H2O rather than mm Hg because cm H2O is a more sensitive unit of measurement for low pressures.
Intrapulmonary Pressure
- During inspiration, intrapulmonary pressure decreases relative to atmospheric pressure.
- During expiration, intrapulmonary pressure increases relative to atmospheric pressure.
Elastic Recoil of the Thorax
- Elastic recoil of the thorax plays a crucial role in expiration by helping to return the thorax to its original shape.
Pulmonary Ventilation
- Bronchodilation increases pulmonary ventilation by increasing airflow.
- Bronchoconstriction decreases pulmonary ventilation by decreasing airflow.
- Alveolar surfactant increases pulmonary ventilation by reducing surface tension in the alveoli.
Respiratory Cycle
- The sternum and rib cage play a crucial role in the respiratory cycle by expanding and relaxing to facilitate breathing.
Respiratory Disorders
- Restrictive disorders of respiration are characterized by a reduction in lung volume, whereas obstructive disorders are characterized by a reduction in airflow.
Respiratory Terms
- Eupnea refers to normal, tranquil breathing.
- Dyspnea refers to difficult or labored breathing.
- Hyperpnea refers to rapid, deep breathing.
- Kussmaul respiration refers to rapid, deep breathing often seen in diabetic ketoacidosis.
Minute Respiratory Volume
- Minute respiratory volume is calculated by multiplying tidal volume by respiratory rate.
Neural Control of Respiration
- The neural pathway for voluntary control of respiration involves the cerebral cortex, brainstem, and spinal cord.
Airflow, Pressure, and Resistance
- The mathematical relationship among airflow, pressure, and resistance in the context of pulmonary ventilation is described by the equation: Pressure = (Airflow x Resistance).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.