Podcast
Questions and Answers
What is the main job of the cardiovascular system?
What is the main job of the cardiovascular system?
To keep blood moving.
What is the purpose of the renin-angiotensin-aldosterone system (RAAS)?
What is the purpose of the renin-angiotensin-aldosterone system (RAAS)?
The RAAS regulates blood pressure and water balance.
What is the main job of aldosterone?
What is the main job of aldosterone?
Aldosterone stimulates the DCT and collecting duct to reabsorb sodium ions.
What is the name of the hormone that regulates the reabsorption of water?
What is the name of the hormone that regulates the reabsorption of water?
Osmoreceptors detect pressure changes.
Osmoreceptors detect pressure changes.
Baroreceptors detect osmolality changes.
Baroreceptors detect osmolality changes.
What are the two types of baroreceptors?
What are the two types of baroreceptors?
How does the respiratory system regulate pH?
How does the respiratory system regulate pH?
How does the renal system regulate pH?
How does the renal system regulate pH?
What is the role of ammonia in the regulation of blood pH?
What is the role of ammonia in the regulation of blood pH?
What is the pH scale?
What is the pH scale?
Flashcards
Osmoregulation
Osmoregulation
The process of maintaining salt and water balance (osmotic balance) across membranes within the body.
Osmoreceptors
Osmoreceptors
Specialized neurons located in the hypothalamus that are sensitive to changes in osmolarity. They detect changes in the concentration of solutes in the blood.
Baroreceptors
Baroreceptors
Specialized sensory receptors located in the walls of blood vessels that detect changes in blood pressure. They help maintain blood pressure by sending signals to the brain.
ADH (Antidiuretic Hormone)
ADH (Antidiuretic Hormone)
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Renin-Angiotensin-Aldosterone System (RAAS)
Renin-Angiotensin-Aldosterone System (RAAS)
Signup and view all the flashcards
Renin
Renin
Signup and view all the flashcards
Angiotensinogen
Angiotensinogen
Signup and view all the flashcards
Angiotensin I
Angiotensin I
Signup and view all the flashcards
ACE (Angiotensin Converting Enzyme)
ACE (Angiotensin Converting Enzyme)
Signup and view all the flashcards
Angiotensin II
Angiotensin II
Signup and view all the flashcards
Homeostasis
Homeostasis
Signup and view all the flashcards
Negative Feedback
Negative Feedback
Signup and view all the flashcards
Set Point
Set Point
Signup and view all the flashcards
ADH (Antidiuretic Hormone)
ADH (Antidiuretic Hormone)
Signup and view all the flashcards
Acidosis
Acidosis
Signup and view all the flashcards
Alkalosis
Alkalosis
Signup and view all the flashcards
Renal Regulation of Blood pH
Renal Regulation of Blood pH
Signup and view all the flashcards
Bicarbonate Reabsorption
Bicarbonate Reabsorption
Signup and view all the flashcards
Hydrogen Ion Secretion
Hydrogen Ion Secretion
Signup and view all the flashcards
Ammoniagenesis
Ammoniagenesis
Signup and view all the flashcards
pH
pH
Signup and view all the flashcards
Acid
Acid
Signup and view all the flashcards
Base
Base
Signup and view all the flashcards
Buffer
Buffer
Signup and view all the flashcards
Phosphate Buffer System
Phosphate Buffer System
Signup and view all the flashcards
Bicarbonate Buffer System
Bicarbonate Buffer System
Signup and view all the flashcards
Carbonic Anhydrase
Carbonic Anhydrase
Signup and view all the flashcards
Study Notes
Renal Physiology III: Regulatory Mechanisms in the Kidney
- Renal Physiology III focuses on homeostasis in the kidney
- Includes mechanisms for osmoregulation, hormonal regulation of water and ion balance (ADH, aldosterone), and blood pH regulation.
Learning Outcomes
- Students will understand the principles of osmoregulation
- Describe how fluid volume and solute concentration are monitored and regulated by the renal system.
- Students will understand how the renal system balances pH levels in the blood.
Homeostasis & Feedback
- Homeostasis is crucial for survival and adaptation to environmental changes.
- Negative feedback mechanisms are central to maintaining homeostasis, aiming for a set point within normal ranges.
- Endotherms, like mammals, use negative feedback to maintain constant internal body temperature. Nerves in the skin detect heat and signal the brain, which triggers responses in the skin and muscles.
- Normal body temperature for endotherms is 36.1-37.2°C
- Ectotherms, like reptiles, have body temperatures that fluctuate with the external environment.
Basic Elements of Regulatory Circuits
- The regulatory circuit involves a receptor, control center, and effector.
- The receptor detects a change, and the control center sends a signal to the effector to restore homeostasis.
- Examples of parameters regulated include body temperature, blood glucose, blood pressure, fluid volume, and osmolarity(concentration of solutes in body fluids).
- Ranges for normal blood pressure are systolic <120/Diastolic <80 mmHg
- Normal ranges for blood glucose are 4-10 mmol/L
- Normal blood pH is 7.35 – 7.45
Osmolarity, Fluid Volume Interconnections
- Blood pressure is influenced by blood volume. Increased blood volume increases blood pressure
- Osmolarity is the concentration of solutes in body fluids. A balance in osmolarity is important for the function of enzymes and proteins.
- The kidneys maintain pH by excreting hydrogen ions (H+) and reabsorbing bicarbonate (HCO3-).
The Kidneys Role in Regulation
- Kidneys respond to changes in blood pressure and osmolarity by adjusting excretion/reabsorption of water, sodium and other electrolytes.
- The antidiuretic hormone (ADH) is involved.
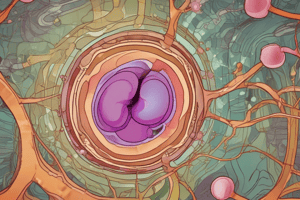
Osmoregulation
- Osmoregulation is the process of maintaining salt and water balance across cell membranes.
- Osmoreceptors, baroreceptors, ADH, and the renin-angiotensin-aldosterone system play crucial roles in osmoregulation.
Ion/Water Transport: The Receptors
- Sodium concentration and water volume are monitored and regulated , despite not having direct sodium-sensing receptors.
- Osmolality and volume changes are indirectly detected by osmoreceptors and baroreceptors,respectively.
Osmoreceptors
- Specialized neurons located in the hypothalamus detect changes in osmolarity.
- In a hypertonic (high osmolarity) environment, water moves out of the cell, causing it to shrink. This increases nervous signals, triggering ADH release.
- In an isotonic or hypotonic environment, the cell is unaffected.
Signals Generated by Osmoreceptors
- Osmoreceptors signal ADH release from neurons in the hypothalamus.
- ADH, also called vasopressin, is a peptide hormone that regulates water reabsorption in the kidneys.
- ADH increases water permeability in the collecting ducts and collecting ducts through aquaporins, resulting in concentrated urine.
H/Vasopressin Regulation
- Excess water—decreased osmolarity—results in lower ADH secretion, decreasing water permeability and increasing water excretion.
- Dehydration—increased osmolarity—causes increased ADH secretion, increasing water permeability and water reabsorption.
Ion/Water Transport: Baroreceptors
- Baroreceptors are specialized pressure sensors in blood vessels, monitoring blood pressure.
- Two types of baroreceptors exist, high-pressure and low-pressure. High-pressure baroreceptors are in the carotid sinus and aortic arch. Low-pressure baroreceptors are located in the large veins of the heart, the pulmonary vasculature, and the juxtaglomerular cells of the kidneys.
- High-pressure receptors detect rapid changes in blood pressure; low-pressure receptors monitor changes in blood volume over time.
Short-Term and Long-Term Adjustments
- Short-term adjustments relate to cardiac output and resistance, influenced by the autonomic nervous system.
- Long-term adjustments involve total blood volume, regulating mechanisms like urine output, and thirst,
- HP Baroreceptors sense a lack of stretching of the artery walls which stimulates quick adjustments to maintain blood pressure.
Renin-Angiotensin-Aldosterone System (RAAS)
- The RAAS is a crucial system for maintaining blood volume and systemic vascular resistance
- Key triggers for RAAS are loss of blood volume, drop in blood pressure, and specific changes in the kidney (drop in filtration rate).
- This involves a series of enzymatic reactions in which the final product, aldosterone, triggers sodium retention in the kidneys, which in turn leads to water retention and an increase in blood pressure.
Activation of RAAS
- JG cells are activated by sympathetic nerve fibers and low pressure baroreceptors
- Macula densa cells, cells detect changes in salt concentration from the filtrate.
- The three signals trigger a series of reactions involved in maintaining balance in blood pressure, total blood volume and blood pressure.
Angiotensin-Aldosterone System Explained
- Renin is released into the blood, converting angiotensinogen into angiotensin I.
- Angiotensin I is converted into angiotensin II by ACE, causing vasoconstriction of the afferent and efferent arterioles, decreasing glomerular filtration rate, and increasing blood pressure
- Angiotensin II also stimulates the adrenal cortex to release aldosterone. This hormone increases water reabsorption and sodium retention in the kidneys.
- These combined effects help restore blood volume and blood pressure.
The Kidney and pH Balance (Overview)
- The kidneys are responsible for long-term pH balance, distinct from the respiratory system's short-term response.
- Kidneys reabsorb bicarbonate (HCO3-) and secrete hydrogen ions (H+) to regulate blood pH levels (7.35 – 7.45).
- These processes involve various cellular mechanisms within the nephrons.
Key Points
- Blood pH, pressure, volume, and osmolarity are interconnected and regulated by the kidneys.
- Osmoreceptors in the hypothalamus monitor osmolarity.
- Baroreceptors detect changes in blood pressure.
- RAAS responds to fluctuations in blood pressure and volume.
- The respiratory system and kidneys regulate blood pH, with the kidneys playing a longer-term role.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.