Podcast
Questions and Answers
What is the primary component of the renal corpuscle?
What is the primary component of the renal corpuscle?
- Bowman's capsule only
- Glomerulus only
- Collecting duct
- Bowman's capsule and glomerulus (correct)
Cortical nephrons make up the majority of nephrons in the human kidney.
Cortical nephrons make up the majority of nephrons in the human kidney.
True (A)
What is the primary function of the glomerulus?
What is the primary function of the glomerulus?
Filter blood plasma
The ascending limb of the loop of Henle in juxtamedullary nephrons has __________ and __________ regions.
The ascending limb of the loop of Henle in juxtamedullary nephrons has __________ and __________ regions.
Which of the following statements is true about peritubular capillaries?
Which of the following statements is true about peritubular capillaries?
The net filtration pressure (NFP) is determined only by hydrostatic pressure.
The net filtration pressure (NFP) is determined only by hydrostatic pressure.
How much blood volume do the kidneys typically receive from cardiac output at rest?
How much blood volume do the kidneys typically receive from cardiac output at rest?
Match the following components of the nephron with their functions:
Match the following components of the nephron with their functions:
Which pressure is responsible for promoting filtration in the glomerular capillaries?
Which pressure is responsible for promoting filtration in the glomerular capillaries?
Interstitial fluid hydrostatic pressure (IFHP) promotes filtration.
Interstitial fluid hydrostatic pressure (IFHP) promotes filtration.
What is primarily detected by the macula densa?
What is primarily detected by the macula densa?
What is the average glomerular filtration rate (GFR) for a young healthy adult weighing 70 kg?
What is the average glomerular filtration rate (GFR) for a young healthy adult weighing 70 kg?
Angiotensin I is converted to angiotensin II in the kidneys.
Angiotensin I is converted to angiotensin II in the kidneys.
What cells regulate the intraglomerular capillary blood flow?
What cells regulate the intraglomerular capillary blood flow?
The equation for net filtration pressure (NFP) is NFP = (CHP + IFOP) -- (_____ + IFHP).
The equation for net filtration pressure (NFP) is NFP = (CHP + IFOP) -- (_____ + IFHP).
What factors determine the glomerular filterability?
What factors determine the glomerular filterability?
The ____ pathway is particularly located at the proximal convoluted tubule and is involved in tubular reabsorption.
The ____ pathway is particularly located at the proximal convoluted tubule and is involved in tubular reabsorption.
Match the following elements with their corresponding transport method:
Match the following elements with their corresponding transport method:
The glomerular filtrate is isotonic to blood plasma and contains cell and protein complexes.
The glomerular filtrate is isotonic to blood plasma and contains cell and protein complexes.
What happens to reabsorption if the glomerular filtration rate (GFR) is too high?
What happens to reabsorption if the glomerular filtration rate (GFR) is too high?
Match the following components with their roles in the filtration process:
Match the following components with their roles in the filtration process:
What is the blood colloid osmotic pressure (BCOP)?
What is the blood colloid osmotic pressure (BCOP)?
Efferent arteriole constriction decreases glomerular filtration rate (GFR).
Efferent arteriole constriction decreases glomerular filtration rate (GFR).
What is the normal mean arterial pressure (MAP) at which GFR is 125 mL/min?
What is the normal mean arterial pressure (MAP) at which GFR is 125 mL/min?
The mechanism that provides feedback based on filtrate osmolarity is called the ______.
The mechanism that provides feedback based on filtrate osmolarity is called the ______.
Match the following pressures with their definitions:
Match the following pressures with their definitions:
What happens to GFR when mean arterial pressure (MAP) exceeds 180 mm Hg?
What happens to GFR when mean arterial pressure (MAP) exceeds 180 mm Hg?
Macula densa cells sense sodium chloride concentration in filtrate.
Macula densa cells sense sodium chloride concentration in filtrate.
What effect does increased MAP have on the afferent arterioles?
What effect does increased MAP have on the afferent arterioles?
What triggers the release of NO and renin when GFR is low?
What triggers the release of NO and renin when GFR is low?
Adenosine causes vasodilation of the afferent arteriole when GFR is high.
Adenosine causes vasodilation of the afferent arteriole when GFR is high.
What is the effect of sympathetic nervous system (SNS) innervation on renal blood flow (RBF) and glomerular filtration rate (GFR)?
What is the effect of sympathetic nervous system (SNS) innervation on renal blood flow (RBF) and glomerular filtration rate (GFR)?
The primary hormone that increases afferent blood flow but decreases efferent blood flow is called ______.
The primary hormone that increases afferent blood flow but decreases efferent blood flow is called ______.
Match the following hormones with their effects on renal blood flow:
Match the following hormones with their effects on renal blood flow:
What is the main effect of angiotensin II on renal blood flow?
What is the main effect of angiotensin II on renal blood flow?
The sympathetic nervous system has a minimal effect on renal function except during fight-or-flight response.
The sympathetic nervous system has a minimal effect on renal function except during fight-or-flight response.
How does the Na-K-2CI cotransporter function under conditions of high GFR?
How does the Na-K-2CI cotransporter function under conditions of high GFR?
Flashcards are hidden until you start studying
Study Notes
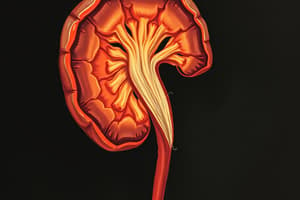
The Renal Corpuscle
- The renal corpuscle is the filtering unit of the nephron and consists of the glomerulus, a network of capillaries, enclosed by the Bowman's capsule.
- The renal corpuscle connects to convoluted tubules in the renal cortex and the loop of Henle, which extends into the medulla.
Nephron Types
- There are two types of nephrons: cortical and juxtamedullary.
- Cortical nephrons represent the majority (80%) and have a renal corpuscle located in the outer cortex.
- Juxtamedullary nephrons represent the minority (20%) and have a renal corpuscle located in the deep cortex.
- Juxtamedullary nephrons have longer loops of Henle that extend into the deep medulla, allowing for the production of very dilute or very concentrated urine.
Renal Blood Flow
- The kidneys receive a large amount of blood, approximately 20-25% of cardiac output at rest.
- 95% of this blood flow supplies the renal cortex, where the glomerulus is located.
Vascular Components of the Nephron
- Glomerulus: This is the site of blood filtration, with a high hydrostatic pressure (~55 mm Hg) driving filtration.
- Afferent Arteriole: Supplies the glomerulus with blood. It has a thick muscular wall that regulates blood flow and filtration pressure.
- Efferent Arteriole: Drains the glomerulus and branches into peritubular capillaries.
- Peritubular Capillaries: These capillaries surround the renal tubules and facilitate reabsorption and equilibrium of substances. Hydrostatic pressure is low (~13 mm Hg).
Net Filtration Pressure (NFP)
- NFP is the driving force behind glomerular filtration, determined by the balance of hydrostatic pressure and osmotic pressure.
- Starling's Law states: NFP = (CHP + IFOP) -- (PCOP + IFHP).
- Pressures favoring filtration:
- Capillary Hydrostatic Pressure (CHP)
- Interstitial Fluid Osmotic Pressure (IFOP)
- Pressures opposing filtration:
- Plasma Colloid Osmotic Pressure (PCOP)
- Interstitial Fluid Hydrostatic Pressure (IFHP)
- In glomerular capillaries, CHP is higher than PCOP, driving filtration.
- In peritubular capillaries, PCOP is higher than CHP, driving reabsorption.
Glomerular Filtration Rate (GFR)
- GFR is the rate at which fluid is filtered from the glomerular capillaries into Bowman's capsule.
- GFR is determined by the permeability and surface area of the filtration membrane and the NFP.
- Three physical barriers ensure selective filtration:
- Glomerular capillary wall with pores between endothelial cells
- Basement membrane composed of collagen and glycoproteins, which repel plasma proteins
- Podocytes, mobile foot processes that form filtration slits
- Factors influencing glomerular filterability:
- Molecular weight: Size-exclusion is the primary factor.
- Charge of the molecule: The negative charge of the basement membrane and podocytes repels anions.
- Average GFR for a healthy adult is 125 mL/min or 180 L/day (36 times blood volume).
GFR Regulation
- Maintaining a constant GFR is crucial for homeostasis.
- High GFR reduces reabsorption.
- Low GFR leads to excessive reabsorption and inadequate waste product excretion.
- Three mechanisms regulate GFR:
- Renal Autoregulation:
- This mechanism maintains a constant RBF and GFR despite variations in arterial blood pressure (from 80 to 180 mm Hg).
- Two mechanisms contribute to autoregulation:
- Myogenic mechanism: This is a stretch response where increased MAP triggers vasoconstriction of the afferent arteriole, reducing GFR. Conversely, decreased MAP induces vasodilation, increasing GFR.
- Tubuloglomerular feedback mechanism: This mechanism utilizes macula densa cells, which sense the filtrate osmolarity and adjust glomerular resistance. High GFR results in high NaCI in the filtrate, triggering adenosine release and vasoconstriction. Low GFR results in low NaCI, activating NO release and vasodilation.
- Neural Regulation:
- The sympathetic nervous system via norepinephrine can alter glomerular resistance.
- Maximal SNS activation can induce significant vasoconstriction and reduce GFR, usually seen in fight-or-flight situations or after hemorrhage.
- Moderate SNS activation causes minor vasoconstriction, reducing RBF and increasing blood volume and pressure due to fluid retention.
- Hormonal Regulation:
- Atrial Natriuretic Peptide (ANP): Increases afferent blood flow and reduces efferent blood flow, leading to increased GFR but no change in RBF.
- Angiotensin II: Decreases afferent blood flow and significantly reduces efferent blood flow, causing reduced RBF with maintained or slightly reduced GFR.
- Angiotensin II regulation by tubuloglomerular feedback:
- Reduced GFR triggers renin release from the juxtaglomerular cells.
- Renin converts angiotensinogen to angiotensin I.
- Angiotensin-converting enzyme (ACE) converts angiotensin I to II in the lungs.
- Angiotensin II causes vasoconstriction of both afferent and efferent arterioles.
- Overall, reduced RBF but maintained or slightly increased GFR due to increased perfusion pressure.
- Renal Autoregulation:
Fine-Tuning of Filtration
- Intraglomerular mesangial cells fine-tune filtration by regulating intraglomerular capillary blood flow.
- These cells contract in response to angiotensin II, ANP, ADH, NO, and capillary stretch, decreasing surface area for filtration and reducing GFR.
Tubular Reabsorption
- Reabsorption of filtered substances is a highly selective process, reclaiming almost all glucose and 99.5% of filtered salts.
- Only excess sugars, salts, and waste products escape reabsorption.
- Reabsorption occurs via two pathways:
- Paracellular pathway: This pathway is primarily present in the proximal convoluted tubule, allowing for passive movement of substances between cells.
- Transcellular pathway: This pathway is more prominent in the distal tubules and collecting ducts due to the increased necessity for selectivity and fine-tuning.
- Methods of Transport:
- Active Transport: This energy-requiring process transports substances like Na+, H+, K+, Ca2+, and Mg2+ against their concentration gradient.
- Secondary Active Transport: This process utilizes the energy generated by active transport of one substance to move another substance. Examples include glucose, amino acids, H+, and Cl-, often with Na+ as the cotransporter molecule.
- Pinocytosis (active process): This mechanism involves engulfing filtered proteins into the cell via small vesicles.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.