Podcast
Questions and Answers
Which of the following is the primary function of the baroreceptor reflex in maintaining mean arterial pressure (MAP)?
Which of the following is the primary function of the baroreceptor reflex in maintaining mean arterial pressure (MAP)?
- Rapid, short-term adjustments to MAP (correct)
- Regulation of sodium excretion by the kidneys
- Stimulation of renin release from the kidneys
- Long-term regulation of blood volume
The renin-angiotensin-aldosterone system (RAAS) primarily contributes to the short-term regulation of mean arterial pressure (MAP).
The renin-angiotensin-aldosterone system (RAAS) primarily contributes to the short-term regulation of mean arterial pressure (MAP).
False (B)
What is the primary trigger for the release of atrial natriuretic peptide (ANP)?
What is the primary trigger for the release of atrial natriuretic peptide (ANP)?
Atrial stretch
Increased mean arterial pressure (MAP) directly increases sodium excretion through a mechanism known as ______ natriuresis.
Increased mean arterial pressure (MAP) directly increases sodium excretion through a mechanism known as ______ natriuresis.
Match the following hormones with their primary effect on mean arterial pressure (MAP):
Match the following hormones with their primary effect on mean arterial pressure (MAP):
Which of the following best describes the interaction between the cardiovascular and renal systems in maintaining mean arterial pressure (MAP)?
Which of the following best describes the interaction between the cardiovascular and renal systems in maintaining mean arterial pressure (MAP)?
The sympathetic nervous system decreases heart rate and contractility, leading to decreased mean arterial pressure (MAP).
The sympathetic nervous system decreases heart rate and contractility, leading to decreased mean arterial pressure (MAP).
What is the primary role of the vasomotor center in the medulla oblongata regarding mean arterial pressure (MAP) regulation?
What is the primary role of the vasomotor center in the medulla oblongata regarding mean arterial pressure (MAP) regulation?
______, released by endothelial cells, is a potent vasoconstrictor that increases peripheral resistance and mean arterial pressure (MAP).
______, released by endothelial cells, is a potent vasoconstrictor that increases peripheral resistance and mean arterial pressure (MAP).
Which of the following is a potential consequence of dysregulation between the cardiovascular and renal systems?
Which of the following is a potential consequence of dysregulation between the cardiovascular and renal systems?
Increased blood oxygen levels stimulate chemoreceptors, leading to increased sympathetic activity and vasoconstriction.
Increased blood oxygen levels stimulate chemoreceptors, leading to increased sympathetic activity and vasoconstriction.
Name one metabolic factor that can cause vasodilation in active tissues.
Name one metabolic factor that can cause vasodilation in active tissues.
The ability of blood vessels to constrict in response to increased pressure and dilate in response to decreased pressure is known as ______ autoregulation.
The ability of blood vessels to constrict in response to increased pressure and dilate in response to decreased pressure is known as ______ autoregulation.
Which of the following is an age-related change that can affect the regulation of mean arterial pressure (MAP)?
Which of the following is an age-related change that can affect the regulation of mean arterial pressure (MAP)?
What is the direct effect of Angiotensin II on blood vessels?
What is the direct effect of Angiotensin II on blood vessels?
ADH release decreases water reabsorption in the kidneys, decreasing blood volume.
ADH release decreases water reabsorption in the kidneys, decreasing blood volume.
Which organ produces angiotensinogen?
Which organ produces angiotensinogen?
Renin is released by the ______.
Renin is released by the ______.
Match the following blood pressure regulators with the effect they induce:
Match the following blood pressure regulators with the effect they induce:
Which of the following results from decreased parasympathetic activity?
Which of the following results from decreased parasympathetic activity?
The baroreceptor reflex is primarily effective for long-term MAP regulation.
The baroreceptor reflex is primarily effective for long-term MAP regulation.
What is the location of baroreceptors?
What is the location of baroreceptors?
Angiotensin-converting enzyme (ACE) converts angiotensin I into angiotensin ______.
Angiotensin-converting enzyme (ACE) converts angiotensin I into angiotensin ______.
Match each hormone to its effect:
Match each hormone to its effect:
Which hormone stimulates the hypothalamus to increase thirst?
Which hormone stimulates the hypothalamus to increase thirst?
Increased blood volume leads to decreased MAP.
Increased blood volume leads to decreased MAP.
What is the effect of increased MAP on sodium excretion?
What is the effect of increased MAP on sodium excretion?
The primary regulator of blood volume is the ______.
The primary regulator of blood volume is the ______.
Match the nerve to its effect:
Match the nerve to its effect:
Which of the following is released from the adrenal medulla?
Which of the following is released from the adrenal medulla?
Nitric oxide (NO) is a potent vasoconstrictor.
Nitric oxide (NO) is a potent vasoconstrictor.
What stimulates chemoreceptors?
What stimulates chemoreceptors?
The ______ integrates information from baroreceptors, chemoreceptors, and emotional centers to influence cardiovascular and renal function.
The ______ integrates information from baroreceptors, chemoreceptors, and emotional centers to influence cardiovascular and renal function.
Match the reflex with the related conditions:
Match the reflex with the related conditions:
During exercise, which reflex helps to increase heart rate and vasoconstriction?
During exercise, which reflex helps to increase heart rate and vasoconstriction?
Renal function typically improves with age, enhancing the kidneys' ability to regulate blood volume and blood pressure.
Renal function typically improves with age, enhancing the kidneys' ability to regulate blood volume and blood pressure.
Name one condition that may result in excessive RAAS activity.
Name one condition that may result in excessive RAAS activity.
Heart failure can lead to compensatory activation of the ______, resulting in fluid retention and increased MAP.
Heart failure can lead to compensatory activation of the ______, resulting in fluid retention and increased MAP.
Match the following elements of the RAAS with their function:
Match the following elements of the RAAS with their function:
What effect does increased ANP levels have on renin?
What effect does increased ANP levels have on renin?
Which of the following is NOT a direct effect of Angiotensin II that contributes to increased Mean Arterial Pressure (MAP)?
Which of the following is NOT a direct effect of Angiotensin II that contributes to increased Mean Arterial Pressure (MAP)?
The baroreceptor reflex is primarily a long-term regulator of Mean Arterial Pressure (MAP).
The baroreceptor reflex is primarily a long-term regulator of Mean Arterial Pressure (MAP).
How do the kidneys directly respond to an increase in Mean Arterial Pressure (MAP) to help regulate blood volume?
How do the kidneys directly respond to an increase in Mean Arterial Pressure (MAP) to help regulate blood volume?
The autonomic nervous system influences blood pressure regulation; more specifically, the ______ nervous system increases heart rate, contractility, and vasoconstriction.
The autonomic nervous system influences blood pressure regulation; more specifically, the ______ nervous system increases heart rate, contractility, and vasoconstriction.
Flashcards
Baroreceptors
Baroreceptors
Detect changes in MAP; decreased MAP increases sympathetic activity; increased MAP increases parasympathetic activity.
Baroreceptor Location
Baroreceptor Location
Located in the carotid sinus and aortic arch. They detect changes in mean arterial pressure (MAP).
Baroreceptor Reflex Speed
Baroreceptor Reflex Speed
Rapid response to MAP changes; primarily for short-term regulation.
Renin Release
Renin Release
Signup and view all the flashcards
Renin Function
Renin Function
Signup and view all the flashcards
Angiotensin-Converting Enzyme (ACE)
Angiotensin-Converting Enzyme (ACE)
Signup and view all the flashcards
Angiotensin II Effects
Angiotensin II Effects
Signup and view all the flashcards
Aldosterone Function
Aldosterone Function
Signup and view all the flashcards
ADH (Antidiuretic Hormone) Function
ADH (Antidiuretic Hormone) Function
Signup and view all the flashcards
RAAS Response Time
RAAS Response Time
Signup and view all the flashcards
ANP (Atrial Natriuretic Peptide) Release
ANP (Atrial Natriuretic Peptide) Release
Signup and view all the flashcards
ANP Effects
ANP Effects
Signup and view all the flashcards
ANP's Effect on Sodium
ANP's Effect on Sodium
Signup and view all the flashcards
Overall Effect of ANP
Overall Effect of ANP
Signup and view all the flashcards
Kidney's Blood Volume Regulation
Kidney's Blood Volume Regulation
Signup and view all the flashcards
Pressure Natriuresis
Pressure Natriuresis
Signup and view all the flashcards
Pressure Diuresis
Pressure Diuresis
Signup and view all the flashcards
Kidneys and RAAS
Kidneys and RAAS
Signup and view all the flashcards
Cardiovascular System's Role
Cardiovascular System's Role
Signup and view all the flashcards
Renal System's Role
Renal System's Role
Signup and view all the flashcards
Kidneys as MAP Regulator
Kidneys as MAP Regulator
Signup and view all the flashcards
Sympathetic Nervous System
Sympathetic Nervous System
Signup and view all the flashcards
Parasympathetic Nervous System
Parasympathetic Nervous System
Signup and view all the flashcards
Autonomic Nervous System Integration
Autonomic Nervous System Integration
Signup and view all the flashcards
Epinephrine and Norepinephrine
Epinephrine and Norepinephrine
Signup and view all the flashcards
Endothelin
Endothelin
Signup and view all the flashcards
Nitric Oxide (NO)
Nitric Oxide (NO)
Signup and view all the flashcards
Causes of Hypertension
Causes of Hypertension
Signup and view all the flashcards
Heart Failure and MAP
Heart Failure and MAP
Signup and view all the flashcards
Renal Failure and MAP
Renal Failure and MAP
Signup and view all the flashcards
Chemoreceptors
Chemoreceptors
Signup and view all the flashcards
Chemoreceptor Stimulation
Chemoreceptor Stimulation
Signup and view all the flashcards
Effects of Chemoreceptor Reflex
Effects of Chemoreceptor Reflex
Signup and view all the flashcards
Hypothalamus
Hypothalamus
Signup and view all the flashcards
Metabolic Factors
Metabolic Factors
Signup and view all the flashcards
Myogenic Autoregulation
Myogenic Autoregulation
Signup and view all the flashcards
Short-Term Control Mechanisms
Short-Term Control Mechanisms
Signup and view all the flashcards
Long-Term Control Mechanisms
Long-Term Control Mechanisms
Signup and view all the flashcards
Baroreceptor Sensitivity
Baroreceptor Sensitivity
Signup and view all the flashcards
Renal Function as you age
Renal Function as you age
Signup and view all the flashcards
Baroreceptor Reflex during exercise
Baroreceptor Reflex during exercise
Signup and view all the flashcards
Long term regulation during exercise
Long term regulation during exercise
Signup and view all the flashcards
Hypothalamus & CNS
Hypothalamus & CNS
Signup and view all the flashcards
Medulla Oblongata
Medulla Oblongata
Signup and view all the flashcards
Hypothalamus & CNS
Hypothalamus & CNS
Signup and view all the flashcards
Study Notes
- The renal and cardiovascular systems collaborate to maintain mean arterial pressure (MAP) through various interconnected mechanisms
- These systems regulate blood volume, cardiac output, and peripheral resistance to ensure adequate tissue perfusion
Baroreceptor Reflex
- Baroreceptors, located in the carotid sinus and aortic arch, detect changes in MAP
- When MAP decreases, baroreceptors reduce their firing rate, leading to increased sympathetic activity and decreased parasympathetic activity
- Increased sympathetic activity causes vasoconstriction, increased heart rate, and increased cardiac contractility, raising MAP
- Decreased parasympathetic activity further contributes to increased heart rate
- Conversely, when MAP increases, baroreceptor firing increases, leading to decreased sympathetic activity and increased parasympathetic activity
- This response causes vasodilation, decreased heart rate, and decreased cardiac contractility, lowering MAP
- The baroreceptor reflex is a rapid response, primarily effective for short-term MAP regulation
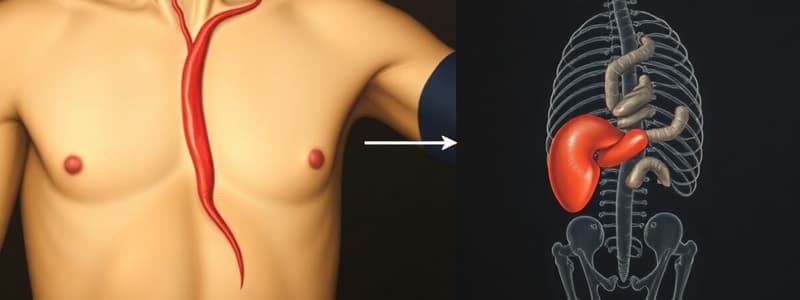
Renin-Angiotensin-Aldosterone System (RAAS)
- The kidneys play a crucial role in long-term MAP regulation through the RAAS
- When MAP decreases, the kidneys release renin
- Renin converts angiotensinogen (produced by the liver) into angiotensin I
- Angiotensin-converting enzyme (ACE), primarily in the lungs, converts angiotensin I into angiotensin II
- Angiotensin II has multiple effects that increase MAP:
- Vasoconstriction: Angiotensin II is a potent vasoconstrictor, increasing peripheral resistance
- Aldosterone release: Angiotensin II stimulates the adrenal cortex to release aldosterone
- ADH release: Angiotensin II stimulates the posterior pituitary to release antidiuretic hormone (ADH)
- Thirst stimulation: Angiotensin II stimulates the hypothalamus to increase thirst
- Aldosterone increases sodium reabsorption in the kidneys, leading to increased water retention and blood volume
- ADH increases water reabsorption in the kidneys, further increasing blood volume
- Increased blood volume increases cardiac output and MAP
- The RAAS is a slower response compared to the baroreceptor reflex, but it is essential for long-term MAP control
Atrial Natriuretic Peptide (ANP)
- Atrial natriuretic peptide (ANP) is released by the atria of the heart in response to atrial stretch, which occurs with increased blood volume
- ANP has effects that decrease MAP:
- Vasodilation: ANP promotes vasodilation, decreasing peripheral resistance
- Sodium excretion: ANP increases sodium excretion by the kidneys, leading to increased water loss and decreased blood volume
- Renin inhibition: ANP inhibits renin release, reducing the production of angiotensin II and aldosterone
- By reducing blood volume and peripheral resistance, ANP lowers MAP
Renal Regulation of Blood Volume
- The kidneys regulate blood volume by controlling the excretion of water and sodium
- Increased blood volume leads to increased MAP, while decreased blood volume leads to decreased MAP
- The kidneys respond to changes in MAP through several mechanisms:
- Pressure natriuresis: Increased MAP directly increases sodium excretion
- Pressure diuresis: Increased MAP directly increases water excretion
- RAAS modulation: As described above, the kidneys adjust renin release based on MAP
Interaction between Systems
- The cardiovascular and renal systems continuously interact to maintain MAP within a narrow range
- The baroreceptor reflex provides rapid, short-term adjustments to MAP
- The RAAS and ANP provide slower, long-term adjustments to blood volume and vascular resistance
- The kidneys act as the primary regulator of blood volume, which is a critical determinant of MAP
- These systems are also influenced by other factors, such as the autonomic nervous system, hormones, and local factors
Autonomic Nervous System
- The autonomic nervous system (ANS) plays a significant role in regulating both the cardiovascular and renal systems
- The sympathetic nervous system increases heart rate, contractility, and vasoconstriction, leading to increased MAP
- It also stimulates renin release from the kidneys
- The parasympathetic nervous system decreases heart rate and has minimal direct effects on blood vessels, leading to decreased MAP
- The ANS integrates signals from baroreceptors, chemoreceptors, and higher brain centers to coordinate cardiovascular and renal responses
Hormonal Influences
- Several hormones, in addition to those already mentioned (angiotensin II, aldosterone, ADH, and ANP), influence MAP
- Epinephrine and norepinephrine, released from the adrenal medulla, increase heart rate, contractility, and vasoconstriction, leading to increased MAP
- Endothelin, released by endothelial cells, is a potent vasoconstrictor, increasing peripheral resistance and MAP
- Nitric oxide (NO), also released by endothelial cells, is a vasodilator, decreasing peripheral resistance and MAP
Clinical Significance
- Dysregulation of the interaction between the cardiovascular and renal systems can lead to various clinical conditions
- Hypertension (high blood pressure) can result from excessive RAAS activity, increased sympathetic activity, or impaired renal function
- Heart failure can lead to decreased cardiac output and compensatory activation of the RAAS, resulting in fluid retention and increased MAP
- Renal failure can impair the kidneys' ability to regulate blood volume and blood pressure, leading to hypertension or hypotension
Chemoreceptor Reflex
- Chemoreceptors in the carotid and aortic bodies detect changes in blood oxygen, carbon dioxide, and pH levels
- Decreased oxygen, increased carbon dioxide, or decreased pH stimulate chemoreceptors, leading to increased sympathetic activity
- Increased sympathetic activity causes vasoconstriction, increased heart rate, and increased respiratory rate, which helps to restore normal blood gas levels and MAP
- The chemoreceptor reflex is particularly important during conditions such as hypoxia or hypercapnia
Central Nervous System (CNS) Control
- Higher brain centers, such as the hypothalamus and medulla oblongata, play a crucial role in regulating MAP
- The hypothalamus integrates information from various sources, including baroreceptors, chemoreceptors, and emotional centers, to influence cardiovascular and renal function
- The medulla oblongata contains the vasomotor center, which controls sympathetic and parasympathetic outflow to the heart and blood vessels
- These CNS centers ensure that MAP is maintained at an appropriate level to meet the body's needs
Local Control Mechanisms
- In addition to systemic mechanisms, local factors can also influence blood vessel diameter and blood flow
- Metabolic factors, such as oxygen, carbon dioxide, lactic acid, and adenosine, can cause vasodilation in active tissues, increasing blood flow to meet metabolic demands
- Myogenic autoregulation refers to the ability of blood vessels to constrict in response to increased pressure and dilate in response to decreased pressure, helping to maintain constant blood flow
- These local control mechanisms work in conjunction with systemic mechanisms to ensure adequate tissue perfusion
Integration of Short-Term and Long-Term Control
- Short-term control mechanisms, such as the baroreceptor and chemoreceptor reflexes, provide rapid adjustments to MAP in response to acute changes
- Long-term control mechanisms, such as the RAAS and renal regulation of blood volume, provide sustained adjustments to MAP over days or weeks
- These systems work together to maintain MAP within a narrow range and ensure adequate tissue perfusion
- For example, during exercise, the baroreceptor reflex helps to increase heart rate and vasoconstriction, while long-term adjustments in blood volume help to sustain these changes
Age-Related Changes
- The ability of the cardiovascular and renal systems to regulate MAP can decline with age
- Baroreceptor sensitivity may decrease, leading to blunted responses to changes in blood pressure
- Renal function may decline, impairing the kidneys' ability to regulate blood volume and blood pressure
- These age-related changes can increase the risk of hypertension and other cardiovascular diseases
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.