Podcast
Questions and Answers
What is the primary function of the urinary system?
What is the primary function of the urinary system?
- Production of hormones for growth and development
- Regulation of body temperature
- Absorption of nutrients from food
- Removal of wastes and regulation of water within the body (correct)
Which part of the kidney filters waste and excess fluids from the blood?
Which part of the kidney filters waste and excess fluids from the blood?
- Renal cortex
- Renal pelvis
- Renal medulla
- Bowman's capsule (correct)
What is the name of the tube that connects the kidney to the urinary bladder?
What is the name of the tube that connects the kidney to the urinary bladder?
- Ureter (correct)
- Urethra
- Renal vein
- Renal artery
What is the term for the concentration of ions in the blood?
What is the term for the concentration of ions in the blood?
What is produced by the kidneys to stimulate the production of red blood cells?
What is produced by the kidneys to stimulate the production of red blood cells?
What is the term for the muscular tube that carries urine from the urinary bladder to the outside of the body?
What is the term for the muscular tube that carries urine from the urinary bladder to the outside of the body?
What is the name of the structure that collects urine from the kidney and channels it into the renal pelvis?
What is the name of the structure that collects urine from the kidney and channels it into the renal pelvis?
What is the active form of vitamin D produced by the kidneys?
What is the active form of vitamin D produced by the kidneys?
What is the process by which solutes and fluid are forced out of the capillaries and into the glomerular capsule?
What is the process by which solutes and fluid are forced out of the capillaries and into the glomerular capsule?
Which part of the renal tubule is responsible for returning water and some solutes back into the capillaries?
Which part of the renal tubule is responsible for returning water and some solutes back into the capillaries?
What is the term for the process by which wastes, drugs, and excess ions are secreted into the renal tubule from the capillaries?
What is the term for the process by which wastes, drugs, and excess ions are secreted into the renal tubule from the capillaries?
Which structure is the site of glomerular filtration?
Which structure is the site of glomerular filtration?
What is the correct order of urine formation?
What is the correct order of urine formation?
What is the function of the loop of Henle?
What is the function of the loop of Henle?
What is the term for the entire process of urine formation?
What is the term for the entire process of urine formation?
What is the glomerular capsule also known as?
What is the glomerular capsule also known as?
What happens when stretch receptors detect stretch in the bladder wall?
What happens when stretch receptors detect stretch in the bladder wall?
What happens when somatic efferent neurons decrease their impulses?
What happens when somatic efferent neurons decrease their impulses?
Why is incontinence normal in infants?
Why is incontinence normal in infants?
At what age do toddlers typically begin toilet training?
At what age do toddlers typically begin toilet training?
What percentage of elderly adults have normal kidney function?
What percentage of elderly adults have normal kidney function?
What happens to the bladder in elderly adults?
What happens to the bladder in elderly adults?
What happens to the kidneys during pregnancy?
What happens to the kidneys during pregnancy?
Why is there an increased risk of UTI during pregnancy?
Why is there an increased risk of UTI during pregnancy?
What is the primary function of the glomerular filtration process?
What is the primary function of the glomerular filtration process?
Which of the following substances is NOT filtered into the filtrate during glomerular filtration?
Which of the following substances is NOT filtered into the filtrate during glomerular filtration?
What is the primary function of the proximal convoluted tubule in the nephron?
What is the primary function of the proximal convoluted tubule in the nephron?
What is the main solute in urine?
What is the main solute in urine?
Which hormone increases the reabsorption of water and ions in the distal convoluted tubule and collecting duct?
Which hormone increases the reabsorption of water and ions in the distal convoluted tubule and collecting duct?
What is the result of the renin-angiotensin-aldosterone system?
What is the result of the renin-angiotensin-aldosterone system?
Which of the following is NOT a characteristic of urine?
Which of the following is NOT a characteristic of urine?
What is the function of antidiuretic hormone (ADH) in the nephron?
What is the function of antidiuretic hormone (ADH) in the nephron?
What stimulates the release of ADH from the posterior pituitary?
What stimulates the release of ADH from the posterior pituitary?
What is the effect of atrial natriuretic peptide (ANP) on sodium reabsorption?
What is the effect of atrial natriuretic peptide (ANP) on sodium reabsorption?
What is the primary function of parathyroid hormone (PTH)?
What is the primary function of parathyroid hormone (PTH)?
What is the effect of erythropoietin on red blood cell production?
What is the effect of erythropoietin on red blood cell production?
What is the role of the kidneys in vitamin D activation?
What is the role of the kidneys in vitamin D activation?
What is the function of the internal urethral sphincter?
What is the function of the internal urethral sphincter?
What is the effect of the detrusor muscle contraction on urination?
What is the effect of the detrusor muscle contraction on urination?
What is the effect of increased blood acidity on the kidney?
What is the effect of increased blood acidity on the kidney?
What happens to the bladder's capacity during pregnancy?
What happens to the bladder's capacity during pregnancy?
Why do elderly adults experience incontinence?
Why do elderly adults experience incontinence?
What is the normal frequency of voiding in newborns?
What is the normal frequency of voiding in newborns?
What happens to the kidneys during pregnancy?
What happens to the kidneys during pregnancy?
What is the reason for the increased risk of UTI during pregnancy?
What is the reason for the increased risk of UTI during pregnancy?
What is the effect of the external urethral sphincter relaxing and opening?
What is the effect of the external urethral sphincter relaxing and opening?
At what age do toddlers typically begin to develop control of the external urethral sphincter?
At what age do toddlers typically begin to develop control of the external urethral sphincter?
What is the percentage of elderly adults with normal kidney function?
What is the percentage of elderly adults with normal kidney function?
What happens to the nephrons in elderly adults?
What happens to the nephrons in elderly adults?
What is the effect of impulses from the brain on the external urethral sphincter?
What is the effect of impulses from the brain on the external urethral sphincter?
Flashcards are hidden until you start studying
Study Notes
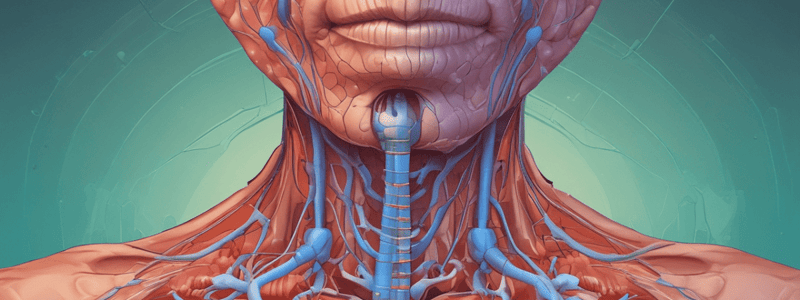
The Urinary System
- The urinary system consists of the kidneys, ureters, bladder, and urethra
- The kidneys filter waste and excess fluids from the blood and regulate electrolyte levels
- The ureters carry urine from the kidneys to the bladder
- The bladder stores urine until it is eliminated from the body through the urethra
The Kidney
- The kidney has three main parts: the renal cortex, renal medulla, and renal pelvis
- The renal cortex is the outer layer of the kidney and contains the glomeruli
- The renal medulla is the inner layer of the kidney and contains the nephrons
- The renal pelvis is the funnel-shaped structure that collects urine from the nephrons
The Nephron
- The nephron is the functional unit of the kidney and consists of the renal corpuscle, proximal convoluted tubule, loop of Henle, and distal convoluted tubule
- The renal corpuscle, also known as Bowman's capsule, is the site of glomerular filtration
- The proximal convoluted tubule reabsorbs water and solutes from the filtrate
- The loop of Henle is responsible for concentrating the urine
- The distal convoluted tubule and collecting duct refine the concentration of the urine
Urine Formation
- Urine formation involves three processes: glomerular filtration, tubular reabsorption, and tubular secretion
- Glomerular filtration occurs when the blood pressure forces water and solutes out of the capillaries and into the glomerular capsule
- Tubular reabsorption occurs when the proximal convoluted tubule reabsorbs water and solutes from the filtrate
- Tubular secretion occurs when the distal convoluted tubule and collecting duct secrete waste products and excess ions into the urine
Hormonal Influences
- Aldosterone stimulates the kidneys to reabsorb sodium and water, increasing blood volume and blood pressure
- Antidiuretic hormone (ADH) stimulates the kidneys to reabsorb water, reducing urine production and increasing blood volume
- Atrial natriuretic peptide (ANP) inhibits the reabsorption of sodium, increasing urine production and reducing blood volume
- Parathyroid hormone (PTH) increases calcium reabsorption in the kidneys, regulating blood calcium levels
Other Functions of the Kidney
- The kidney produces erythropoietin, which stimulates the production of red blood cells in response to low oxygen levels
- The kidney activates vitamin D, which is essential for calcium absorption and bone health
- The kidney helps regulate blood pH by secreting hydrogen ions and reabsorbing bicarbonate ions
The Bladder and Urethra
- The bladder is a muscular sac that stores urine until it is eliminated from the body
- The urethra is the tube that carries urine from the bladder to the outside of the body
- The internal urethral sphincter is an involuntary muscle that relaxes to allow urine to flow
- The external urethral sphincter is a voluntary muscle that can be controlled to delay urination
Micturition
- Micturition is the process of urination, which involves the relaxation of the internal and external urethral sphincters and the contraction of the bladder wall
Developmental Changes Across the Lifespan
- Newborns have incomplete bladder control and may urinate frequently
- Toddlerhood is a time of toilet training, during which the child learns to control the external urethral sphincter
- In older adults, the kidneys shrink, and the bladder loses tone, leading to incontinence and increased frequency of urination
- During pregnancy, the kidneys enlarge, and the ureters become dilated, leading to increased urine retention and risk of UTIs
The Urinary System
- The urinary system consists of the kidneys, ureters, bladder, and urethra
- The kidneys filter waste and excess fluids from the blood and regulate electrolyte levels
- The ureters carry urine from the kidneys to the bladder
- The bladder stores urine until it is eliminated from the body through the urethra
The Kidney
- The kidney has three main parts: the renal cortex, renal medulla, and renal pelvis
- The renal cortex is the outer layer of the kidney and contains the glomeruli
- The renal medulla is the inner layer of the kidney and contains the nephrons
- The renal pelvis is the funnel-shaped structure that collects urine from the nephrons
The Nephron
- The nephron is the functional unit of the kidney and consists of the renal corpuscle, proximal convoluted tubule, loop of Henle, and distal convoluted tubule
- The renal corpuscle, also known as Bowman's capsule, is the site of glomerular filtration
- The proximal convoluted tubule reabsorbs water and solutes from the filtrate
- The loop of Henle is responsible for concentrating the urine
- The distal convoluted tubule and collecting duct refine the concentration of the urine
Urine Formation
- Urine formation involves three processes: glomerular filtration, tubular reabsorption, and tubular secretion
- Glomerular filtration occurs when the blood pressure forces water and solutes out of the capillaries and into the glomerular capsule
- Tubular reabsorption occurs when the proximal convoluted tubule reabsorbs water and solutes from the filtrate
- Tubular secretion occurs when the distal convoluted tubule and collecting duct secrete waste products and excess ions into the urine
Hormonal Influences
- Aldosterone stimulates the kidneys to reabsorb sodium and water, increasing blood volume and blood pressure
- Antidiuretic hormone (ADH) stimulates the kidneys to reabsorb water, reducing urine production and increasing blood volume
- Atrial natriuretic peptide (ANP) inhibits the reabsorption of sodium, increasing urine production and reducing blood volume
- Parathyroid hormone (PTH) increases calcium reabsorption in the kidneys, regulating blood calcium levels
Other Functions of the Kidney
- The kidney produces erythropoietin, which stimulates the production of red blood cells in response to low oxygen levels
- The kidney activates vitamin D, which is essential for calcium absorption and bone health
- The kidney helps regulate blood pH by secreting hydrogen ions and reabsorbing bicarbonate ions
The Bladder and Urethra
- The bladder is a muscular sac that stores urine until it is eliminated from the body
- The urethra is the tube that carries urine from the bladder to the outside of the body
- The internal urethral sphincter is an involuntary muscle that relaxes to allow urine to flow
- The external urethral sphincter is a voluntary muscle that can be controlled to delay urination
Micturition
- Micturition is the process of urination, which involves the relaxation of the internal and external urethral sphincters and the contraction of the bladder wall
Developmental Changes Across the Lifespan
- Newborns have incomplete bladder control and may urinate frequently
- Toddlerhood is a time of toilet training, during which the child learns to control the external urethral sphincter
- In older adults, the kidneys shrink, and the bladder loses tone, leading to incontinence and increased frequency of urination
- During pregnancy, the kidneys enlarge, and the ureters become dilated, leading to increased urine retention and risk of UTIs
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.