Podcast
Questions and Answers
Why is it important to adhere to radiation safety principles despite the stealthy properties of x-rays?
Why is it important to adhere to radiation safety principles despite the stealthy properties of x-rays?
- To avoid unnecessary personnel exposure that could become biologically significant. (correct)
- To improve the image quality of x-ray scans.
- To ensure compliance with international radiation unit standards.
- To reduce the cost of radiation monitoring equipment.
Radiation exposure and radiation absorption are the same thing.
Radiation exposure and radiation absorption are the same thing.
False (B)
What factor is used to estimate the difference in biologic effectiveness of various radiation types?
What factor is used to estimate the difference in biologic effectiveness of various radiation types?
quality factor
The International System of Units, also known as ______ units, was developed in 1977 to promote universal adoption.
The International System of Units, also known as ______ units, was developed in 1977 to promote universal adoption.
In the context of radiation exposure and absorption, why do some tissues absorb radiation more effectively than others, leading to different absorbed doses?
In the context of radiation exposure and absorption, why do some tissues absorb radiation more effectively than others, leading to different absorbed doses?
Which of the following properties is NOT associated with X-rays and gamma rays?
Which of the following properties is NOT associated with X-rays and gamma rays?
The impact of electromagnetic radiation on biological systems is directly proportional to its wavelength.
The impact of electromagnetic radiation on biological systems is directly proportional to its wavelength.
What term describes the phenomenon where a negatively charged electron and a positively charged atom are created following the ejection of an electron from the atom by a photon?
What term describes the phenomenon where a negatively charged electron and a positively charged atom are created following the ejection of an electron from the atom by a photon?
The energy of electromagnetic radiation is described by the formula: Energy = Planck's constant × speed of light / ______.
The energy of electromagnetic radiation is described by the formula: Energy = Planck's constant × speed of light / ______.
Match the potential biological effects of ionization of DNA due to X-ray exposure with their descriptions:
Match the potential biological effects of ionization of DNA due to X-ray exposure with their descriptions:
Why is it crucial to minimize radiation exposure for personnel working in a radiation environment?
Why is it crucial to minimize radiation exposure for personnel working in a radiation environment?
The 'electron volt' (eV) and 'kilovoltage peak' (kVp) both measure the same physical quantity and can be used interchangeably in the context of X-ray production and application.
The 'electron volt' (eV) and 'kilovoltage peak' (kVp) both measure the same physical quantity and can be used interchangeably in the context of X-ray production and application.
If the wavelength of an EM radiation decreases by half, how does its energy change, assuming all other factors remain constant?
If the wavelength of an EM radiation decreases by half, how does its energy change, assuming all other factors remain constant?
Who is credited with the accidental discovery of X-rays?
Who is credited with the accidental discovery of X-rays?
Gamma rays are always more energetic than X-rays.
Gamma rays are always more energetic than X-rays.
What was the first known medical application of X-rays shortly after their discovery?
What was the first known medical application of X-rays shortly after their discovery?
X-rays are produced by electron interactions ______ the nucleus, while gamma rays are released from ______ the nucleus.
X-rays are produced by electron interactions ______ the nucleus, while gamma rays are released from ______ the nucleus.
Which type of electromagnetic radiation has the shortest wavelength?
Which type of electromagnetic radiation has the shortest wavelength?
As the frequency of electromagnetic radiation increases, its wavelength also increases.
As the frequency of electromagnetic radiation increases, its wavelength also increases.
What is the approximate wavelength range for visible light?
What is the approximate wavelength range for visible light?
Electromagnetic radiation is characterized by oscillating electric and magnetic fields that move in planes at ________ angles to each other.
Electromagnetic radiation is characterized by oscillating electric and magnetic fields that move in planes at ________ angles to each other.
Match the type of electromagnetic radiation with its origin:
Match the type of electromagnetic radiation with its origin:
If electromagnetic radiation has a frequency of $3 \times 10^{8}$ Hz, what is its wavelength?
If electromagnetic radiation has a frequency of $3 \times 10^{8}$ Hz, what is its wavelength?
Which of the following statements accurately describes the relationship between wavelength, frequency, and velocity of electromagnetic radiation?
Which of the following statements accurately describes the relationship between wavelength, frequency, and velocity of electromagnetic radiation?
An astronomer detects electromagnetic radiation from a distant galaxy that has a wavelength of $2.1 \times 10^{-7}$ m. The source is determined to be the result of an electron energy level transition. Based on the provided information, what type of electromagnetic radiation is the astronomer most likely observing?
An astronomer detects electromagnetic radiation from a distant galaxy that has a wavelength of $2.1 \times 10^{-7}$ m. The source is determined to be the result of an electron energy level transition. Based on the provided information, what type of electromagnetic radiation is the astronomer most likely observing?
Which of the following units is used to quantify radiation exposure in the SI system?
Which of the following units is used to quantify radiation exposure in the SI system?
The roentgen is an SI unit and its use is strongly encouraged by The National Institute of Standards and Technology.
The roentgen is an SI unit and its use is strongly encouraged by The National Institute of Standards and Technology.
What is the SI unit for absorbed dose, and what is its equivalent in terms of energy absorption per unit mass?
What is the SI unit for absorbed dose, and what is its equivalent in terms of energy absorption per unit mass?
The equivalent biologic dose is measured in Sieverts (Sv) in the SI system, which is the dose in Grays (Gy) times the __________.
The equivalent biologic dose is measured in Sieverts (Sv) in the SI system, which is the dose in Grays (Gy) times the __________.
Match the following radiation quantities with their corresponding units:
Match the following radiation quantities with their corresponding units:
Why is limiting exposure to radiation important?
Why is limiting exposure to radiation important?
Explain why lead is a more efficient absorber of X-rays compared to water.
Explain why lead is a more efficient absorber of X-rays compared to water.
A new radiation shielding material boasts a unique property: instead of absorbing radiation, it converts incoming high-energy photons into harmless sound waves, which then dissipate rapidly. Assuming this material is successfully developed, how would it impact established radiation safety protocols that primarily focus on minimizing exposure and absorbed dose?
A new radiation shielding material boasts a unique property: instead of absorbing radiation, it converts incoming high-energy photons into harmless sound waves, which then dissipate rapidly. Assuming this material is successfully developed, how would it impact established radiation safety protocols that primarily focus on minimizing exposure and absorbed dose?
Who is credited with the discovery of X-rays?
Who is credited with the discovery of X-rays?
What is the primary difference between X-rays and gamma rays concerning their origin?
What is the primary difference between X-rays and gamma rays concerning their origin?
Roentgen was awarded the first Nobel Prize for Physics in recognition of his discovery of _________.
Roentgen was awarded the first Nobel Prize for Physics in recognition of his discovery of _________.
Which of the following imaging modalities is referred to as the 'workhorse' of veterinary imaging?
Which of the following imaging modalities is referred to as the 'workhorse' of veterinary imaging?
What was the initial observation that led Roentgen to deduce the existence of X-rays?
What was the initial observation that led Roentgen to deduce the existence of X-rays?
Match the following terms with their correct description:
Match the following terms with their correct description:
Insanely difficult: Considering the historical context, what specific characteristic of early X-ray use contributed most significantly to both its rapid adoption and subsequent health concerns?
Insanely difficult: Considering the historical context, what specific characteristic of early X-ray use contributed most significantly to both its rapid adoption and subsequent health concerns?
Which statement regarding characteristic X-rays is correct?
Which statement regarding characteristic X-rays is correct?
Which statement regarding the properties of X-rays is incorrect?
Which statement regarding the properties of X-rays is incorrect?
Which statement regarding the target of an X-ray tube is correct?
Which statement regarding the target of an X-ray tube is correct?
Which statement regarding protective lead aprons and gloves is incorrect?
Which statement regarding protective lead aprons and gloves is incorrect?
Which statement regarding X-rays and gamma rays is incorrect?
Which statement regarding X-rays and gamma rays is incorrect?
The X-ray tube is moved from an FFD of 40 inches to an FFD of 60 inches. At 40 inches, a technique of 10 mAs and 70 kVp was suitable. Which milliamperage value would most likely result in a comparable exposure at the new distance of 60 inches?
The X-ray tube is moved from an FFD of 40 inches to an FFD of 60 inches. At 40 inches, a technique of 10 mAs and 70 kVp was suitable. Which milliamperage value would most likely result in a comparable exposure at the new distance of 60 inches?
What is the definition of the grid ratio?
What is the definition of the grid ratio?
Pregnant radiation workers are not allowed to have any occupational radiation exposure.
Pregnant radiation workers are not allowed to have any occupational radiation exposure.
Which statement regarding photoelectric and Compton interactions is true?
Which statement regarding photoelectric and Compton interactions is true?
If the mAs is changed from 10 to 20, what will be the effect on the X-rays?
If the mAs is changed from 10 to 20, what will be the effect on the X-rays?
Which statement regarding X-ray production is correct?
Which statement regarding X-ray production is correct?
Characteristic X-rays are produced as part of:
Characteristic X-rays are produced as part of:
Which of the following statements pertaining to the use of a grid in a film-screen radiography system is CORRECT?
Which of the following statements pertaining to the use of a grid in a film-screen radiography system is CORRECT?
Which statement is correct?
Which statement is correct?
Which statement regarding photon absorption processes is correct?
Which statement regarding photon absorption processes is correct?
You are going to radiograph the thorax of a dog. You need 10 mAs. Which of the following combinations of mA and time would be the most preferable to use in terms of avoiding any artifacts? Assume that your X-ray machine will allow you to select any of these combinations.
You are going to radiograph the thorax of a dog. You need 10 mAs. Which of the following combinations of mA and time would be the most preferable to use in terms of avoiding any artifacts? Assume that your X-ray machine will allow you to select any of these combinations.
The responsibility to alert the practice manager or radiation supervisor that the employee is pregnant rests with the:
The responsibility to alert the practice manager or radiation supervisor that the employee is pregnant rests with the:
Flashcards
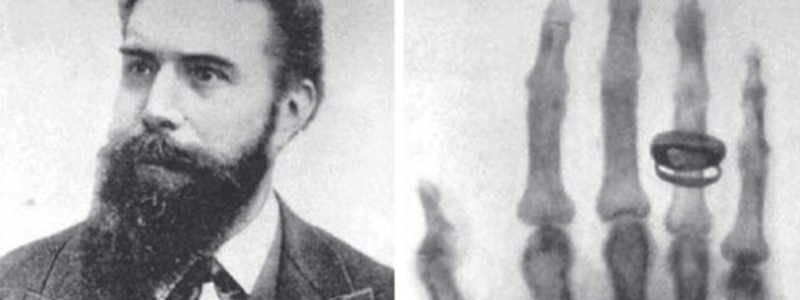
Wilhelm Conrad Roentgen
Wilhelm Conrad Roentgen
German physicist who discovered x-rays on November 8, 1895.
X-rays
X-rays
Electromagnetic radiation discovered by Roentgen, used for medical imaging.
Angiography
Angiography
Using x-rays to visualize blood vessels.
Source of X-rays vs. Gamma rays
Source of X-rays vs. Gamma rays
Signup and view all the flashcards
Electromagnetic (EM) Radiation
Electromagnetic (EM) Radiation
Signup and view all the flashcards
Nuclear imaging
Nuclear imaging
Signup and view all the flashcards
Wavelength
Wavelength
Signup and view all the flashcards
Roentgen's Wife's Hand
Roentgen's Wife's Hand
Signup and view all the flashcards
Radio Waves
Radio Waves
Signup and view all the flashcards
Microwaves
Microwaves
Signup and view all the flashcards
Infrared Radiation
Infrared Radiation
Signup and view all the flashcards
Visible Light
Visible Light
Signup and view all the flashcards
Ultraviolet Radiation
Ultraviolet Radiation
Signup and view all the flashcards
Gamma Rays
Gamma Rays
Signup and view all the flashcards
Wavelength (λ)
Wavelength (λ)
Signup and view all the flashcards
Primary X-Ray Beam Exposure
Primary X-Ray Beam Exposure
Signup and view all the flashcards
Exposure vs. Absorption
Exposure vs. Absorption
Signup and view all the flashcards
Quality Factor
Quality Factor
Signup and view all the flashcards
CGS and SI Units
CGS and SI Units
Signup and view all the flashcards
3 Radiation Measures
3 Radiation Measures
Signup and view all the flashcards
Photon
Photon
Signup and view all the flashcards
X-Ray Properties
X-Ray Properties
Signup and view all the flashcards
EM Radiation Energy Formula
EM Radiation Energy Formula
Signup and view all the flashcards
Electron Volt (eV)
Electron Volt (eV)
Signup and view all the flashcards
Ionization
Ionization
Signup and view all the flashcards
Ion Pair
Ion Pair
Signup and view all the flashcards
Potential effects of X-Rays
Potential effects of X-Rays
Signup and view all the flashcards
Kilovoltage Peak (kVp)
Kilovoltage Peak (kVp)
Signup and view all the flashcards
Neutral Atom Charge
Neutral Atom Charge
Signup and view all the flashcards
Radiation Weighting Factor
Radiation Weighting Factor
Signup and view all the flashcards
Weighting Factor of 1
Weighting Factor of 1
Signup and view all the flashcards
Alpha Particle Weighting
Alpha Particle Weighting
Signup and view all the flashcards
Goal of Radiology
Goal of Radiology
Signup and view all the flashcards
X-rays and Gamma rays
X-rays and Gamma rays
Signup and view all the flashcards
Light and Radio Waves
Light and Radio Waves
Signup and view all the flashcards
Radiation Protection Measures
Radiation Protection Measures
Signup and view all the flashcards
Radiation Exposure
Radiation Exposure
Signup and view all the flashcards
Coulombs per Kilogram (C/kg)
Coulombs per Kilogram (C/kg)
Signup and view all the flashcards
Absorbed Dose
Absorbed Dose
Signup and view all the flashcards
Gray (Gy)
Gray (Gy)
Signup and view all the flashcards
Rad
Rad
Signup and view all the flashcards
Weighting Factor
Weighting Factor
Signup and view all the flashcards
Sievert (Sv)
Sievert (Sv)
Signup and view all the flashcards
rem
rem
Signup and view all the flashcards
Study Notes
- X-rays were discovered in 1895 by Wilhelm Conrad Roentgen and were immediately used for medical purposes like angiography, diagnosis, and treatment.
- Roentgen was awarded the first Nobel Prize for Physics in 1901 for this discovery.
- Despite advances in diagnostic ultrasound, computed tomography, and magnetic resonance imaging, conventional radiography remains a key element in veterinary imaging.
Basic Properties of X-Rays
- Both x-rays and gamma rays are electromagnetic radiation, differentiated by their source.
- X-rays come from electron interactions outside the nucleus.
- Gamma rays are released from inside the nucleus of unstable atoms that have excess energy.
- The energy level of a gamma ray depends on the amount of energy released by an unstable atom.
- The energy of an x-ray is relative to the energy of the electron interacting with an atom.
- Radiopharmaceuticals in nuclear imaging emit gamma rays with energy similar to x-rays used in diagnostic imaging.
Electromagnetic (EM) Radiation
- EM radiation includes radio waves, radar, microwaves, and visible light in addition to x-rays and gamma rays.
- EM radiation contains electric and magnetic fields oscillating in orthogonal planes described by frequency and wavelength.
- EM radiation velocity matches the speed of light, correlating inversely with frequency per the formula V = fλ (velocity = frequency x wavelength).
- X-rays and gamma rays possess particle-like attributes i.e. photons defined as a discrete bundle of EM radiation.
Properties of X-Rays and Gamma Rays
- Exhibit no charge or mass.
- Travel at the speed of light as invisible entities that cannot be felt
- Follow straight paths, undeterred by magnetic fields
- Able to permeate matter, cause fluorescence in certain substances
- Able to expose photographic emulsions
- Able to ionize atoms
Energy Measurement
- Electromagnetic radiation energy equals Planck's constant times speed of light divided by wavelength, therefore the energy is inversely proportional to wavelength.
- An electron volt (eV) measures electromagnetic radiation energy and is gained when one electron accelerates through a 1V potential difference.
- X-rays of just 15 eV energylevel are capable of ionizing atoms.
- Ionization, induced by x-rays in radiography, is when an electron is ejected from an atom that creates an ion pair.
- X-ray interaction with a person may lead to DNA ionization, which can cause mutations, fetal issues, disease susceptibility, cancer, and cataracts.
Radiation Protection
- Minimizing personnel exposure in radiation environments and minimizing patient ionization during imaging procedures can reduce the risk of side effects.
- Biological injury risk from x-rays or gamma rays is greater because the wavelength of visible light is 10,000 times longer than the wavelength of x-rays
- Radio waves are an even longer wavelength.
- Light and radio waves do not produce tissue ionization or DNA damage due to lower energy levels.
- Microwaves may cause biological damage through tissue heating but do not lead to molecular ionization.
Radiation Diagnostic Goals
- Aim is to obtain maximal diagnostic information while minimizing radiation exposure to the patient, personnel, and public by adhering to safety guidelines and using PPE as necessary to mitigate the risks associated with ionizing radiation.
- Digital radiography improves the image while safe radiation practices are disregarded due to the low cost and minimal time to retake.
Concepts and Units
- Radiation exposure and absorption differ, with some tissues absorbing radiation more effectively.
- Biological effect of absorbed dosage can be influenced by radiation type and energy, estimated by a weighting or quality factor.
- Radiation concepts originally measured in the CGS system, were updated in 1977 with the International System of Units (SI units) for universal adoption.
Radiation Exposure
- Radiation exposure is based on the amount of ionization produced in the air quantified by the electrical charge resulting from the ionization
- Coulombs per kilogram of air (C/kg) in SI units, this is sometimes measured in roentgens
- One roentgen equals a charge of 2.58 C/kg in air.
Absorbed Dose
- The x-ray absorption efficiency varies by material.
- The SI unit is gray (Gy), where 1 Gy is 1 joule/kg of absorbed radiation.
- The obsolete unit, rad, equates to 100 ergs/g of tissue, or 100 rads to one gray.
- Exposure to 1 roentgen equals roughly 0.9 cGy or 0.9 rad of absorption in soft tissue such as muscle while more efficient absorption of x-rays in bone results in 1 roentgen exposure.
- Differential x-ray absorption amongst tissues is the basis for radiographic contrast that decreases as photon energy increases.
Dose Equivalent
- Equivalent doses vary in biological effect when giving the same absorbed dose in Gy from different radiation since damage is greater from particulate radiation.
- Difference in biological damage from equal radiation dosages estimated by a weighting factor is used in cases of high ionizing particles like alpha particles.
- Equivalent dosage unit is the sievert (Sv), with Sv derived from multiplying the absorbed dose in Gy and the weighting factor.
- The earlier unit dose equivalency of radiation equivalent in man, or rem is the product of absorbed dose in rads and the weighting factor, and because 1 Gy = 100 rads, 1 Sv = 100 rem.
Radiation Safety Principles
- Principles are based on preventing unnecessary radiation exposure for workers and the public, with the understanding that some low-level exposure is permissible for workers without leading to major abnormalities or disease.
- Adverse effects can be classified as deterministic (threshold with dose-related severity) or stochastic (random, no threshold, dose-independent severity).
- Maximum permissible dose (MPD) is the safe radiation amount for an individual or organ although radiation will have some effect.
International Commission on Radiological Protection (ICRP)
- The ICRP is an independent organization focusing on safety from ionizing radiation providing recommendations and guidance published quarterly.
- The dose limit for radiation workers that avoids stochastic effects is 20 mSv/year, averaging over 5 years, with no single year exceeding 50 mSv, and quarterly exposure not greater than 12.5 mSv.
National Council on Radiation Protection (NCRP)
- The NCRP chartered by Congress in 1964 develops radiation protection recommendations and cooperates with ICRP
- The whole-body limit avoiding stochastic effects for radiation workers is 50 mSv per year and lifetime accumulation not exceeding 10 mSv x age in years with no occupational exposure below 18 years of age
Nuclear Regulatory Commission (NRC)
- The NRC defines federal exposure standards in the United States adopting a maximum annual radiation dose to workers as 50 mSv per year, mirroring the NCRP guidelines.
- The limit for pregnant radiation workers monthly is 0.5 mSv for embryo or fetus and a notification to the supervison is required.
- General radiation exposure limit for the public excluding medical use is 1 mSv per year.
Radiation Exposure
- The public is exposed to natural and man-made radiation.
- Medical procedures accounted for nearly half of the total radiation exposure of the U.S. population in 2006, with a revised breakdown highlighting changes in medical imaging exposure sources.
- Background radiation exposure levels depends on geographic location.
Practical Considerations
- Technologists acting as radiation workers should understand risks, training in patient positioning and in equipment operation as well as proper PPE use, and ALARA principles regarding distance, time, and shielding.
- Personnel distance from the x-ray tube should expand as much as possible to reduce radiation dosage, although shielding is still important.
Distance
- Exposure dose decreases by the square of the distance, meaning doubling distance reduces exposure by a factor of 4.
- Personnel body parts should avoid the primary beam, even when wearing protective aprons and gloves as well as using chemical restraint and sandbags to vacate prior to exposure.
- Effective beam collimation increases distance and minimizes radiation exposure and also increases the distance of the technologist from the primary x-ray beam.
Time
- Time should be reduced by sedation or anesthesia for uncooperative patients plus rotating technical staff to reduce personal exposure levels.
- Retake examinations increase personnel dose with likelihood increasing with greater digital imaging.
Shielding
- State building codes mandate structural shielding to safeguard personnel and the public against radiation exposure.
- PPE i.e. lead-impregnated aprons, gloves, thyroid shields, and eyeglasses, provide effective radiation worker protection, however not used consistently as protective aprons and gloves are designed for use in the x-ray room are usually 0.5 mm Pb equivalent.
- Aprons and gloves should be placed on racks, and visually inspected annually.
Radiation Supervisor Responsibilities:
- The radiation safety program depends on a well-defined radiation supervisor role
- This is a member of the technical staff that optimizes image integrity while reducing occupational exposure,
- Key qualities for a radiation safety supervisor include establishing/supervising written plans, periodic reviews to ensure regulations, training employees, and overseeing radiation surveys with corrective measures.
- Perform equipment checks, assess unusual exposures, educate personnel about radiation protection.
Personnel Dose Monitoring
- Monitoring assesses radiation safety, discloses improper habits, and detects exposure incidents.
- Radiation badges are used consististing of a plastic holder containing radiation-sensitive aluminum oxide or lithium fluoride crystals able to trap energized electrons and relate it to the amount of exposure
- Badges should be analyzed at least quarterly, or monthly during pregnancy.
- Wear only in the controlled areas of the workplace not during personal exams, on the upper or lower torso, and exchange if wearing.
Safety Rules
- Only required personnel may be present
- No one under 18 and all pregnant women must leave the x-ray room during the process
- All assistants should operate on a rotational schedule for minimal exposure
- Tools like sandbags and sponges ought to replace manual restraint whenever possible for safety.
- Personnel body parts must stay out of the main path of radiation at all times
Production of X-Rays
- X-rays production requires accelerating high-speed electrons in a controlled environment
- This is completed through an anode with positive chargers, cathode with negatively charged fliaments, within a vacuüm inside a glass tube to prevent interactions along the filament.
- The more current, the more electrons passing through the filament
- Voltage difference is modified with a kilovoltage peak (kVp) command on x-ray control panel affecting output energy.
Energy Production
- X-rays produced by mechanisms: Collisional interactions (hitting orbital electron from target atom) or radiative interaction (electron passes near nucleus slowing and releasing energy.
- The former produces a small fraction of x-rays, with specific energy linked to binding energy which are termed characteristic x-rays and are specific, but are not the most powerful.
- The latter produces bremsstrahlung (braking) radiation, has a large spectrum, happens frequently,
- The highest possible energy x-ray has KeV equals kilovoltage peak voltage,
Key Differences in Concepts
- Kilo electron volts or KeV is a measurement of energy.
- Kilovoltage peak or kVp is a measurement of voltage.
- Alternating current needs transformers for 120 Kilovolts.
- In the former, 1 KeV is the same as 1000 eV
- When the target alternates between positive and negative, rectification removes negative phases.
- The target is always + with respect to the filament
Heat and Focus
- Most of the electron energy striking the target converts to heat, targets should thus have a high melting point and a wide surface to dissipate heat
- Focal spot is the spot on target with electrons and impacts detail, with angling improving radiation
- X-ray tubes tend to have small filaments, that lower mA
M.A.
- Number of electrons impacts the radiation
- The timer impacts the duration that source flows, or voltage to get to the target
- Milliampere, or mAs, seconds quantify radiation and equate to the seconds lightbulb shines
- The generator then increases output from cyclic current by manipulation
- These increase X-ray energy and create a 6 pulse with rectification.
High Frequency Generators
- High Frequency Generators are the best at what they do, voltage is nearly constant.
- X-ray energy is produced highly ineficiently, with lots of it being converted to heat
- As such, the target must be high melting point and able to withstand heat
How Radiation Works
- Five components: direct scatter, photoelectric effect, secondary scatter, pair production, or direct disintegration -
- Each of these requires an understanding of how a proton works with matter and how film is affected.
- Coherent scattering causes a photon to contact an atom and change its direction, but overall the energy output is minimal
- Photoelectric effect describes when the X-ray source interacts with a tissue electron, leading the X-Ray and its energy to being entirely consumed.
- Compton scattering strikes electron of peripheral shell atom and the original proton scatters
Making a Radiograph
- Beam of x-ray must contain filter that is less energetic
- Beam shape must be configured for size, collimated
- Some x-rays must penetrate and go through, to produce a radiograph
- Depending on structure and patient traits, the beam strikes and records output
Measurement of Film
- All depends on how the silver absorbs and reacts to certain light forms, whether through halide or otherwise
- Most films depend on how the mAs affects and strikes the film relative to the kVp for setting, as distances are relevant by inverse squared law
- To measure, use the formula I1/I2 = (d2/d1)^2
- You will need to control motion to allow short times,
Focal Control
- Also consider if there is a penumbral effect from a diffused focal
- More efficient film may lead to enhanced light
- Intensifying screens may also be a help
- Grids are useful and helpful
- Grid depends on rectangular flat plate that is either absorptive, lead, or material
- They depend on lead strips, angle to periphery
- Must work within FFD, range must be accurate
- Film contrast often varies but depends on mA and kVp
- Radiographic contrast is from a wide variation in thickness, density
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.