Podcast
Questions and Answers
What is one function of the cyst wall secreted by protozoa?
What is one function of the cyst wall secreted by protozoa?
- To promote rapid division
- To attract other hosts
- To help digest food
- To resist unfavorable conditions (correct)
Which of the following is a type of asexual reproduction in protozoa?
Which of the following is a type of asexual reproduction in protozoa?
- Multiple fission (correct)
- Conjugation
- Gametogony
- Syngamy
Where do protozoa primarily inhabit within their definitive host?
Where do protozoa primarily inhabit within their definitive host?
- Jejunum
- Stomach
- Duodenum
- Large intestine (correct)
Which of the following represents the infective stage of protozoa?
Which of the following represents the infective stage of protozoa?
What characterizes the ectoplasm of protozoa?
What characterizes the ectoplasm of protozoa?
Which type of sexual reproduction involves the exchange of nuclear material between organisms?
Which type of sexual reproduction involves the exchange of nuclear material between organisms?
What size range does the trophozoite stage of protozoa typically fall into?
What size range does the trophozoite stage of protozoa typically fall into?
Which organism is a common reservoir host for protozoa?
Which organism is a common reservoir host for protozoa?
What is the primary form of locomotion for amoebae?
What is the primary form of locomotion for amoebae?
Which component is NOT found inside the protoplasm of protozoa?
Which component is NOT found inside the protoplasm of protozoa?
What is the stage of protozoa characterized by a protective membrane?
What is the stage of protozoa characterized by a protective membrane?
How do ciliates primarily absorb nutrients?
How do ciliates primarily absorb nutrients?
Which of the following protozoa is primarily classified as residing in the urogenital tract?
Which of the following protozoa is primarily classified as residing in the urogenital tract?
What type of respiration do protozoa living in tissues and blood primarily use?
What type of respiration do protozoa living in tissues and blood primarily use?
Which type of nutrition involves ingesting solid particles?
Which type of nutrition involves ingesting solid particles?
Which organism is associated with the bloodstream?
Which organism is associated with the bloodstream?
Which method is used for morphological identification of E.histolytica?
Which method is used for morphological identification of E.histolytica?
What is one of the modes of transmission for this infection?
What is one of the modes of transmission for this infection?
What are Charcot-Leyden crystals associated with?
What are Charcot-Leyden crystals associated with?
Which serological test is considered the most sensitive for detecting amoebic liver abscesses?
Which serological test is considered the most sensitive for detecting amoebic liver abscesses?
What symptom is NOT commonly associated with severe cases of intestinal amebiasis?
What symptom is NOT commonly associated with severe cases of intestinal amebiasis?
Which organ is primarily affected in extra-intestinal amoebiasis due to trophozoite invasion?
Which organ is primarily affected in extra-intestinal amoebiasis due to trophozoite invasion?
What is the infectious stage of E.histolytica?
What is the infectious stage of E.histolytica?
Which of the following is a luminal amoebicide used in treatment?
Which of the following is a luminal amoebicide used in treatment?
What is the purpose of cysteine proteinases secreted by trophozoites?
What is the purpose of cysteine proteinases secreted by trophozoites?
What is the definitive host for E.histolytica?
What is the definitive host for E.histolytica?
What indicates the presence of intestinal amebiasis during a stool examination?
What indicates the presence of intestinal amebiasis during a stool examination?
Which of the following is NOT a complication of intestinal ulcers caused by amebiasis?
Which of the following is NOT a complication of intestinal ulcers caused by amebiasis?
Which diagnostic method is NOT typically used for identifying E.histolytica?
Which diagnostic method is NOT typically used for identifying E.histolytica?
What is a common preventive measure against E.histolytica infections?
What is a common preventive measure against E.histolytica infections?
What characterizes an ameboma?
What characterizes an ameboma?
How is autoinfection transmitted in amebiasis?
How is autoinfection transmitted in amebiasis?
What is the shape and size range of the cyst associated with balantidiasis?
What is the shape and size range of the cyst associated with balantidiasis?
Which of the following is NOT a mode of transmission for balantidiasis?
Which of the following is NOT a mode of transmission for balantidiasis?
What is the main component observed in the cytoplasm of the trophozoite that aids in movement and feeding?
What is the main component observed in the cytoplasm of the trophozoite that aids in movement and feeding?
Which of the following clinical symptoms is NOT typically associated with severe balantidiasis?
Which of the following clinical symptoms is NOT typically associated with severe balantidiasis?
What is the first step in the laboratory diagnosis of balantidiasis?
What is the first step in the laboratory diagnosis of balantidiasis?
Which of the following treatments is prescribed for adults suffering from balantidiasis?
Which of the following treatments is prescribed for adults suffering from balantidiasis?
What complication is associated with balantidiasis?
What complication is associated with balantidiasis?
Which structure is characteristic of the cyst's wall in balantidiasis?
Which structure is characteristic of the cyst's wall in balantidiasis?
Flashcards
Protozoa
Protozoa
Microscopic, single-celled organisms performing all life functions, with a complex internal structure and metabolism.
Protozoa Structure
Protozoa Structure
Protozoa are composed of protoplasm, enclosed by a membrane, divided into ectoplasm and endoplasm, containing nucleus, endoplasmic reticulum, food storage, and vacuoles.
Protozoa Movement
Protozoa Movement
Protozoa move using pseudopodia, cilia, flagella or undulant movement.
Trophozoite
Trophozoite
Signup and view all the flashcards
Cysts
Cysts
Signup and view all the flashcards
Protozoa Classification
Protozoa Classification
Signup and view all the flashcards
Protozoa Nutrition
Protozoa Nutrition
Signup and view all the flashcards
Protozoa Excretion
Protozoa Excretion
Signup and view all the flashcards
Amebiasis Transmission
Amebiasis Transmission
Signup and view all the flashcards
Amebiasis Pathogenesis
Amebiasis Pathogenesis
Signup and view all the flashcards
Intestinal Amebiasis Symptoms
Intestinal Amebiasis Symptoms
Signup and view all the flashcards
Amoebic Liver Abscess
Amoebic Liver Abscess
Signup and view all the flashcards
Amoebiasis Diagnosis (Microscopy)
Amoebiasis Diagnosis (Microscopy)
Signup and view all the flashcards
Asymptomatic Amebiasis
Asymptomatic Amebiasis
Signup and view all the flashcards
Intestinal Amebiasis Types
Intestinal Amebiasis Types
Signup and view all the flashcards
Extra-intestinal Amebiasis
Extra-intestinal Amebiasis
Signup and view all the flashcards
Protozoa Secretion
Protozoa Secretion
Signup and view all the flashcards
Asexual Reproduction
Asexual Reproduction
Signup and view all the flashcards
Sexual Reproduction
Sexual Reproduction
Signup and view all the flashcards
Protozoa Habitat
Protozoa Habitat
Signup and view all the flashcards
Trophozoite Stage
Trophozoite Stage
Signup and view all the flashcards
Mature Cyst
Mature Cyst
Signup and view all the flashcards
Quadrinucleate Cyst
Quadrinucleate Cyst
Signup and view all the flashcards
Protozoa Cyst Morphology
Protozoa Cyst Morphology
Signup and view all the flashcards
Amoebiasis Diagnostic Method
Amoebiasis Diagnostic Method
Signup and view all the flashcards
Amoebiasis Treatment
Amoebiasis Treatment
Signup and view all the flashcards
Amoebic Trophozoite Morphology
Amoebic Trophozoite Morphology
Signup and view all the flashcards
Amoebiasis Reservoir Host
Amoebiasis Reservoir Host
Signup and view all the flashcards
Amoebiasis Infective Stage
Amoebiasis Infective Stage
Signup and view all the flashcards
Amoebiasis Diagnostic Stage (two words)
Amoebiasis Diagnostic Stage (two words)
Signup and view all the flashcards
Sigmoidoscopy role
Sigmoidoscopy role
Signup and view all the flashcards
Amoebiasis Geographical Distribution
Amoebiasis Geographical Distribution
Signup and view all the flashcards
Balantidiasis Cyst Shape
Balantidiasis Cyst Shape
Signup and view all the flashcards
Balantidium coli Nuclei
Balantidium coli Nuclei
Signup and view all the flashcards
Balantidiasis Transmission
Balantidiasis Transmission
Signup and view all the flashcards
Balantidium coli Cyst Size
Balantidium coli Cyst Size
Signup and view all the flashcards
Balantidiasis Symptoms (Severe)
Balantidiasis Symptoms (Severe)
Signup and view all the flashcards
Balantidiasis Diagnosis
Balantidiasis Diagnosis
Signup and view all the flashcards
Balantidiasis Treatment (Adults)
Balantidiasis Treatment (Adults)
Signup and view all the flashcards
Balantidiasis complications
Balantidiasis complications
Signup and view all the flashcards
Study Notes
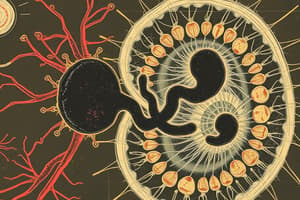
Medical Protozoology
- Protozoa are microscopic, single-celled organisms capable of all life functions.
- Amoebas have a complex internal structure:
- Food vacuole
- Pseudopodia
- Plasmagel
- Plasmasol
- Ectoplasm
- Endoplasm
- Uroid
- Contractile vacuole
- Water vacuole
- Protozoa have a relatively complex internal structure and carry out complex metabolic activities.
- Protozoa's body consists of:
- Protoplasm, enclosed by a cell membrane
- Divided into outer ectoplasm and inner endoplasm,
- Nucleus, endoplasmic reticulum
- Food storage granules, contractile and digestive vacuoles.
- The nucleus contains clumped or dispersed chromatin.
- Locomotion by:
- Pseudopodia (amoebae)
- Cilia (ciliates)
- Flagella (flagellates)
- Undulant movement (sporozoa).
Life Cycle Stages of Protozoa
- Trophozoites: actively feed and multiply.
- Cysts: have a protective membrane, allow protozoa to survive outside the host, usually have resistant walls.
Classification of Protozoa
- Small Intestine: Giardia lamblia
- Large intestine: Entamoeba histolytica
- Blood: Plasmodium species
- Tissue: Toxoplasma gondii
- Urogenital: Trichomonas vaginalis
Nutrition
- Liquid food: Absorption through the body surface.
- Solid particles:
- Pinocytosis (liquid form)
- Phagocytosis (using pseudopodia).
- Cytostome (flagellates or sporozoa, ciliates, amoeba)
Excretion
- Excretion through contractile vacuoles rupturing to outside.
- Some waste products are deposited in cytoplasm.
- In sporozoa, waste is excreted as pigment.
Respiration
- Aerobic: Protozoa living in tissues and blood.
- Anaerobic: Protozoa living in the intestine lumen.
Secretion
- Protozoa secrete digestive ferments, pigments.
- Lytic enzymes help tissue lysis.
- Toxins.
- Cyst walls allow resistance from unfavorable conditions, transfer to other hosts without destruction.
Reproduction
- Asexual reproduction:
- Simple fission: nucleus and cytoplasm divide into equal parts, forming two cells.
- Multiple fission: nucleus divides first into several parts, cytoplasm divides forming several small daughter cells.
- Sexual reproduction:
- Conjugation: exchange of nuclear material between two organisms
- Gametogony: formation of male and female gametes, their union to form zygote.
Entamoeba histolytica
-
Geographical distribution: worldwide, areas with poor sanitation
-
Habitat: large intestine (caecum, colonic flexures, sigmoidorectal region).
-
Definitive host: Man
-
Reservoir host: Dogs, pigs, rats, monkeys
-
Infective stage: Mature cyst
-
Diagnostic stage: cyst and trophozoite
-
Trophozoite Size: 20µm (15-60μm)
-
Shape: Irregular
-
Cytoplasm: Differentiated into ectoplasm, endoplasm
-
Ectoplasm: Clear with a finger-like pseudopodia
-
Endoplasm: Granular, with nucleus, karyosome small and central
-
Spherical nucleus
-
Peripheral chromatin, uniform size, arranged on the inner surface of nuclear membrane
-
Food vacuoles: may contain RBCs (no bacteria)
-
Mature cyst (Quadrinucleate) Size: 15 um (10 - 20 um)
-
Shape: Rounded with thick cyst wall
-
Contents: one to four nuclei, glycogen vacuoles, chromatoid bodies
Mode of Transmission
- Contaminated foods or drinks containing mature cysts.
- Handling food by infected food handlers.
- Flies and cockroaches that carry cysts to exposed food.
- Autoinfection (faeco-oral or hand-to-mouth infection).
Life Cycle
- Excystation in small intestine.
- Trophozoite in large intestines.
- Multiplication.
- Cyst formation (mono-nucleated, bi-nucleated, quadri-nucleated.)
- Extraintestinal spread (liver, lung, brain).
Pathogenesis and Symptomatology
- Trophozoites secrete cysteine proteinases to invade extracellular matrix, host cell lysis and necrosis forming flask-shaped ulcers.
- Amoeba spread from intestine to liver through portal circulation.
- Ulcers may be complicated by secondary bacterial infections with necrosis, sloughing, perforation, peritonitis.
Clinical Pictures
- Asymptomatic infections (cyst passers)
- Symptomatic infections:
- Intestinal amebiasis (dysenteric or non-dysenteric colitis) -incubation period (1 week to 4 weeks)
- Clinical picture depends on parasite virulence factors and host immune response.
- Dysentery and diarrhea (up to 10 bowel movements).
- In severe cases: profuse diarrhea, fever, dehydration, electrolyte imbalance.
- Ameboma: chronic granulomatous lesion in the cecum or rectosigmoid junction.
- Extraintestinal amebiasis:
- Liver, lung, brain abscesses.
- Skin Involvement (amebic cutis).
Diagnosis
-
Clinical and laboratory
- Microscopic: detects trophozoites (loose stools) or cysts (formed stools)
- Direct smear of fresh stool samples.
- Concentration methods (increase parasite detection).
- Permanent stained smear (trichrome or iron hematoxylin).
- Charcot-Leyden crystals (eosinophilic protein).
- Sigmoidoscopy: visualize ulcer or trophozoites (in aspirate or biopsy).
- Microscopic: detects trophozoites (loose stools) or cysts (formed stools)
-
Indirect: serodiagnosis (anti-amoebic antibody tests) including:
- Immunofluorescent antibody tests (IFAT)
- Indirect haemagglutination assays (IHAs)
- Radioimmunoassay (RIA).
- Enzyme-linked immunosorbent assays (ELISAs)
-
Stool antigen
-
Molecular diagnosis
- Radiological investigations (ultrasound or CT) detect complications.
Treatment
- Medical treatment:
- Metronidazole (Flagyl) or Tinidazole (Fasigyn)
- Diloxanide furoate or Paromomycin, Luminal amoebicides (diloxanide furoate and iodoquinol).
- Surgical treatment: rupturing abscess, intestinal perforation, and appendicitis.
Prevention and Control
- Treatment of patients and carriers.
- Proper washing of vegetables.
- Sanitary sewer systems.
- Avoid using human excreta as fertilizer.
- Fly control.
- Personal hygiene measures
Balantidium coli
-
Geographical distribution: worldwide, areas where pigs are raised and sanitation is inadequate.
-
Habitat: large intestine (caecum, colon).
-
Definitive host: Man.
-
Reservoir host: Pigs, less common monkey.
-
Infective stage: Mature cyst.
-
Diagnostic stage: cyst and trophozoite.
-
Trophozoite size: 60 × 45 µm, largest protozoon of man; Ovoid, tapers.
-
Covered with cilia.
-
Cytostome that extends to 1/3 of the body length.
-
Macronucleus (hyaline mass), micronucleus (small, spherical).
-
Granular cytoplasm, contractile vacuoles, food vacuoles (ingested microbes).
-
Cyst size: 52 to 55 μm.
-
Shape: Subspherical to oval.
-
Two nuclei (macronucleus and micronucleus)
-
Cytoplasm: granular, one or two contractile vacuoles
-
Double cyst wall. row of cilia between cyst wall layers.
-
Mode of transmission: similar to Entamoeba histolytica.
-
Life cycle: Multiplication by transverse binary fission, forming two young trophozoites. Cysts, excystation, multiplication, trophozoites in large and small intestine, pass in feces then to environment.
-
Complications: haemorrhage, secondary bacterial infection, appendicitis, intestinal perforation, and peritonitis.
-
Diagnosis: history, clinical picture, laboratory tests (stool examination, direct smear, concentration methods, permanent stains). Colonoscopy/sigmoidoscopy with biopsy.
-
Treatment: Tetracycline (adults 500 mg orally x 4 times daily for 10 days).
-
Prevention: care in handling pigs in pig farms, slaughter houses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.