Podcast
Questions and Answers
What is a common causative organism of acute prostatitis?
What is a common causative organism of acute prostatitis?
- E. coli (correct)
- Streptococcus pneumoniae
- Staphylococcus aureus
- Mycobacterium tuberculosis
Which of the following is associated with benign prostatic hyperplasia (BPH)?
Which of the following is associated with benign prostatic hyperplasia (BPH)?
- Dihydrotestosterone exposure (correct)
- Increased levels of estrogen
- Chronic bacterial infections
- Complete prostate gland removal
What histopathologic finding is commonly seen in chronic bacterial prostatitis?
What histopathologic finding is commonly seen in chronic bacterial prostatitis?
- Fibrosis of the gland
- Necrosis of prostatic tissue
- Presence of many leukocytes (correct)
- Absence of inflammation
In which type of prostatitis is granulomatous reaction typically observed?
In which type of prostatitis is granulomatous reaction typically observed?
What are the common clinical symptoms of acute prostatitis?
What are the common clinical symptoms of acute prostatitis?
Which statement about benign prostatic hyperplasia (BPH) is true?
Which statement about benign prostatic hyperplasia (BPH) is true?
Which of the following conditions is considered a chronic specific prostatitis?
Which of the following conditions is considered a chronic specific prostatitis?
What type of prostatitis can be asymptomatic?
What type of prostatitis can be asymptomatic?
Which of the following symptoms is NOT associated with benign prostatic hyperplasia (BPH)?
Which of the following symptoms is NOT associated with benign prostatic hyperplasia (BPH)?
What role does age play in prostate cancer development?
What role does age play in prostate cancer development?
Which type of cancer is most commonly associated with the prostate?
Which type of cancer is most commonly associated with the prostate?
What is a common morphological characteristic of prostate tumors?
What is a common morphological characteristic of prostate tumors?
Which of the following factors is NOT considered a potential contributor to prostate cancer?
Which of the following factors is NOT considered a potential contributor to prostate cancer?
Which of the following is a common complication of chronic urinary obstruction due to BPH?
Which of the following is a common complication of chronic urinary obstruction due to BPH?
What defines the clinical diagnosis of prostate cancer?
What defines the clinical diagnosis of prostate cancer?
Which of the following statements about squamous metaplasia in the prostate is true?
Which of the following statements about squamous metaplasia in the prostate is true?
Which histological feature is indicative of prostatic carcinoma?
Which histological feature is indicative of prostatic carcinoma?
What does a lower modified Gleason score indicate about prostatic carcinoma?
What does a lower modified Gleason score indicate about prostatic carcinoma?
Which of the following descriptors best defines the architecture seen in prostatic carcinoma?
Which of the following descriptors best defines the architecture seen in prostatic carcinoma?
How is the modified Gleason score calculated?
How is the modified Gleason score calculated?
Which characteristic is NOT typically seen in prostatic carcinoma?
Which characteristic is NOT typically seen in prostatic carcinoma?
Which of the following classifications represents the least aggressive prostatic carcinoma?
Which of the following classifications represents the least aggressive prostatic carcinoma?
What type of staining is associated with amphophilic cytoplasm?
What type of staining is associated with amphophilic cytoplasm?
The presence of which feature would be atypical in normal prostate tissue?
The presence of which feature would be atypical in normal prostate tissue?
Flashcards
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH)
Non-cancerous enlargement of the prostate gland.
Prostate Cancer
Prostate Cancer
Malignant tumor of the prostate gland, most often in men over 50.
BPH Symptoms
BPH Symptoms
Frequent urination, difficulty urinating, painful urination, urinary retention.
Prostate Cancer Symptoms
Prostate Cancer Symptoms
Signup and view all the flashcards
Digital Rectal Exam (DRE)
Digital Rectal Exam (DRE)
Signup and view all the flashcards
Prostate Specific Antigen (PSA)
Prostate Specific Antigen (PSA)
Signup and view all the flashcards
Transurethral Resection of Prostate (TURP)
Transurethral Resection of Prostate (TURP)
Signup and view all the flashcards
Microscopic Prostate Appearance
Microscopic Prostate Appearance
Signup and view all the flashcards
Acute Prostatitis
Acute Prostatitis
Signup and view all the flashcards
Common Causative Organisms (Acute Prostatitis)
Common Causative Organisms (Acute Prostatitis)
Signup and view all the flashcards
Chronic Prostatitis (Non-Specific)
Chronic Prostatitis (Non-Specific)
Signup and view all the flashcards
BPH Pathogenesis
BPH Pathogenesis
Signup and view all the flashcards
BPH Morphology (Gross)
BPH Morphology (Gross)
Signup and view all the flashcards
Chronic Specific Granulomatous Prostatitis
Chronic Specific Granulomatous Prostatitis
Signup and view all the flashcards
Chronic Non-Specific Granulomatous Prostatitis
Chronic Non-Specific Granulomatous Prostatitis
Signup and view all the flashcards
Prostatic Carcinoma
Prostatic Carcinoma
Signup and view all the flashcards
Gleason Score
Gleason Score
Signup and view all the flashcards
Modified Gleason Score
Modified Gleason Score
Signup and view all the flashcards
Gleason 6 or Less
Gleason 6 or Less
Signup and view all the flashcards
Gleason 7
Gleason 7
Signup and view all the flashcards
Gleason 8
Gleason 8
Signup and view all the flashcards
Gleason 9 or 10
Gleason 9 or 10
Signup and view all the flashcards
Prostatic Carcinoma Microscopic Features
Prostatic Carcinoma Microscopic Features
Signup and view all the flashcards
Study Notes
Diseases of Male Genital Organs - Prostatic Disorders
- Prostate disorders are common in men, including inflammation (prostatitis), enlarged prostate (benign prostatic hyperplasia (BPH)), and prostate cancer.
Disorders of the Prostate Gland (DPG)
- Common prostate disorders include inflammation (prostatitis), enlarged prostate (BPH), and prostate cancer.
Acute Prostatitis
- The infection-causing organism reaches the prostate from the posterior urethra.
- Common causative organisms include gonococci, E. coli, Klebsiella, Proteus, and Pseudomonas.
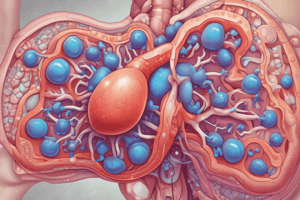
Prostate Gland
- Located between the bladder and the penis.
- Diagram shows its anatomical position relative to surrounding structures like the bladder, urethra, and testicles.
Morphology (Acute Prostatitis)
- Grossly, the prostate gland is enlarged, swollen, and tender.
- Microscopically, there is infiltration of prostatic tissue by many polymorphnuclear leucocytes.
- Edema and vascular dilation are also observed.
Clinically (Acute Prostatitis)
- Symptoms may include fever, chills, body aches, nausea, vomiting, dysuria (painful urination), frequent or urgent need to urinate, difficulty urinating, weak urine stream, and lower abdominal pain, sometimes with tenderness to the prostate.
Chronic Prostatitis (non-specific)
- May be asymptomatic or associated with pain in the genital area, lower abdomen, or lower back, alongside dysuria.
- Men with chronic bacterial prostatitis often have recurring urinary tract infections (UTIs).
- Examination of prostatic secretions after massage reveals many leukocytes.
- Histopathologic diagnosis isn't crucial; most cases develop gradually without prior acute prostatitis.
Chronic Specific Granulomatous Prostatitis
- Includes conditions like Tuberculosis (TB) and schistosomiasis.
Chronic Non-Specific Granulomatous Prostatitis
- Relatively common.
- A reaction to secretions from ruptured prostatic ducts and acini.
- Microscopic examination shows a granulomatous reaction.
Benign Prostatic Hyperplasia (BPH)
- Highly prevalent after age 50 and increases with age.
- The precise cause is unknown but linked to dihydrotestosterone (DHT) exposure in aging men, triggering certain prostate cell proliferation, leading to gland enlargement.
Morphology (BPH)
- Grossly, the gland is enlarged with nodules of varying sizes.
- The urethra lumen is often compressed, becoming narrow.
- The median lobe may protrude into the bladder, leading to obstruction.
- The common method of examining the enlarged gland for gross assessment was once a one-piece prostatectomy, but this is less common now.
Microscopic (BPH)
- Transurethral resection of the prostate (TURP) is usually performed for microscopic analysis.
- Nodules consist of hyperplastic glands and fibromuscular stroma, often with gland dilation and cyst formation.
- Areas of squamous metaplasia and infarcts might occasionally occur.
Clinical Effects and Complications of BPH
- Frequent urination, especially at night (nocturia).
- Difficulty initiating or stopping urination stream.
- Acute urinary retention episodes.
- Chronic urinary tract infections due to urinary stasis (slowed urine flow).
- Urinary bladder hypertrophy and hydronephrosis (kidney infection) are potential complications of prolonged obstruction.
Carcinoma of the Prostate
- Among the most common malignant tumors in men.
- Predominantly affects men over 50.
- Unrelated to benign prostatic hyperplasia (BPH).
- Almost all prostate cancers are adenocarcinomas, with other rare types including small cell neuroendocrine carcinoma, large cell carcinoma, transitional cell carcinoma, and sarcomas.
Etiology (Prostate Cancer)
- Cause is unknown but multiple factors may play a role:
- Increasing age, usually after age 55.
- Higher incidence among Black men compared to White men.
- High testosterone levels.
- Genetic factors.
- Environmental factors (geographic variations).
- Prostatic intraepithelial neoplasia (PIN)
Clinical Diagnosis (Prostate Cancer)
- Based on patient symptoms, a digital rectal exam (DRE), blood tests (prostate-specific antigen (PSA)), and a urinalysis.
Symptoms of Prostate Cancer
- Difficulty initiating or stopping urine flow, weak urine stream.
- Frequent urination, especially at night.
- Pain or burning during urination and ejaculation.
- Blood in the urine or semen.
- Persistent pain in the back, hips, or pelvis.
Digital Rectal Exam (DRE)
- A physical examination method used to assess the prostate gland through the rectum.
Morphology (Prostate Cancer)
- Tumor usually arises from the periphery of the gland, frequently situated in the posterior section, and sometimes doesn't encompass the entire gland.
- Forms nodular masses (single or multiple), displaying a yellowish-gray, homogeneous cut surface.
Microscopic (Prostate Cancer)
- Clinical and radiological features are usually not specific enough for diagnostic criteria.
- Nontargeted biopsies are frequently performed to assess elevated serum prostate-specific antigen (PSA) levels.
- Most prostate cancers are adenocarcinomas, ranging from well-differentiated to undifferentiated forms.
- Key microscopic characteristics aiding diagnosis include: presence of closely packed small glands, absence of basal layer at points in the glands, infiltrative architecture (loss of polarity), large hyperchromatic nuclei, prominent nucleoli, amphophilic cytoplasm (staining with both acid and basic dyes), circumferential perineural invasion, presence of intraluminal contents like crystalloids, blue mucin, or pink amorphous materials.
Grading of the Tumor (Prostate Cancer)
- Based on the modified Gleason score (replacement for the previous 5-point system).
- Focuses on overall glandular patterns and cellular atypia (assessed via low power microscopy), without considering cytologic details present in higher power microscopy.
- Modified Gleason score is determined by adding the numerical values of the two most prevalent grades and is helpful in assessing how likely the cancer will spread. Lower grade indicates slower growth and less aggressive nature.
Staging of the Tumor (Prostate Cancer)
- Based on the TNM staging system.
- Stage T1: Cancer discovered incidentally during transurethral resection of the prostate (TURP). Further subdivided into T1a, T1b, and T1c.
- Stage T2: Cancer confined to the prostate gland.
- Stage T3a and T3b: Shows extra-prostatic extension, possibly involving the seminal vesicles.
- Stage T4: Directly invades adjacent organs.
Prognosis (Prostate Cancer)
- Based on the tumor's grading and staging.
- Grade 5 (Gleason 9 or 10) is the worst prognosis group.
- T1 and T2 are usually treated via surgery and radiotherapy, with approximately a 90% 15-year survival rate.
- Advanced tumors with metastasis generally have a worse prognosis.
Prostate Specific Antigen (PSA)
- Used in diagnosis and management of prostate carcinoma.
- A product of the prostatic epithelium.
- Normal serum PSA level is roughly 4 ng/mL.
- Organ-specific, but not cancer-specific.
- Monitoring PSA levels aids in assessing therapy response and disease progression.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.