Podcast
Questions and Answers
What is the primary goal of DVT management?
What is the primary goal of DVT management?
- To administer anticoagulation therapy indefinitely
- To immediately remove the clot surgically
- To dissolve the existing clot completely
- To stop the clot from getting any bigger and preventing it from breaking loose (correct)
What is the usual duration of heparin therapy for DVT management?
What is the usual duration of heparin therapy for DVT management?
- 7 days
- 3 days
- 10 days
- 5 days (correct)
What is the antidote for heparin?
What is the antidote for heparin?
- Atropine
- Protamine sulphate (correct)
- Narcan
- Vitamin K
What is the primary mechanism of action of thromboembolytic therapy?
What is the primary mechanism of action of thromboembolytic therapy?
What is the primary advantage of using low-molecular-weight heparin (LMWH) over unfractionated heparin?
What is the primary advantage of using low-molecular-weight heparin (LMWH) over unfractionated heparin?
What is the antidote for warfarin (Coumadin)?
What is the antidote for warfarin (Coumadin)?
What is the primary action of fondaparinux?
What is the primary action of fondaparinux?
What is the primary risk associated with heparin-induced thrombocytopenia (HIT)?
What is the primary risk associated with heparin-induced thrombocytopenia (HIT)?
What is the most serious complication of post-operative complications?
What is the most serious complication of post-operative complications?
What is the main reason why venous thrombi form in veins?
What is the main reason why venous thrombi form in veins?
What is Virchow's Triad?
What is Virchow's Triad?
What is the primary purpose of graduated compression stockings?
What is the primary purpose of graduated compression stockings?
What is the primary purpose of pneumatic compression devices?
What is the primary purpose of pneumatic compression devices?
What is the primary purpose of anticoagulation therapy?
What is the primary purpose of anticoagulation therapy?
What is the primary purpose of elevation of the affected limb in suspected DVT?
What is the primary purpose of elevation of the affected limb in suspected DVT?
What is the primary purpose of Homan's Sign?
What is the primary purpose of Homan's Sign?
What is the primary purpose of Duplex Ultrasonography?
What is the primary purpose of Duplex Ultrasonography?
What is the primary purpose of D-dimer blood test?
What is the primary purpose of D-dimer blood test?
What is the primary goal of thrombolytic therapy in the treatment of deep vein thrombosis?
What is the primary goal of thrombolytic therapy in the treatment of deep vein thrombosis?
When is surgical management of deep vein thrombosis indicated?
When is surgical management of deep vein thrombosis indicated?
What is the target therapeutic range for an INR when using warfarin?
What is the target therapeutic range for an INR when using warfarin?
What is the primary complication of heparin therapy?
What is the primary complication of heparin therapy?
What is the primary mechanism of action of thrombolytic therapy?
What is the primary mechanism of action of thrombolytic therapy?
Which vein is most likely to cause a pulmonary embolism?
Which vein is most likely to cause a pulmonary embolism?
What is a major risk factor for pulmonary embolism?
What is a major risk factor for pulmonary embolism?
What is the primary purpose of anticoagulation therapy monitoring?
What is the primary purpose of anticoagulation therapy monitoring?
What is the target therapeutic range for aPTT when using heparin?
What is the target therapeutic range for aPTT when using heparin?
What is the effect of a pulmonary embolism on the pulmonary vascular bed?
What is the effect of a pulmonary embolism on the pulmonary vascular bed?
What is the effect of a pulmonary embolism on the right ventricle?
What is the effect of a pulmonary embolism on the right ventricle?
What is the primary indication for catheter-directed thrombolysis?
What is the primary indication for catheter-directed thrombolysis?
What is the primary mechanism of action of warfarin?
What is the primary mechanism of action of warfarin?
What is the effect of a pulmonary embolism on gas exchange?
What is the effect of a pulmonary embolism on gas exchange?
What can occur when the workload of the right ventricle exceeds its capacity?
What can occur when the workload of the right ventricle exceeds its capacity?
What is the primary purpose of patient education for anticoagulation therapy?
What is the primary purpose of patient education for anticoagulation therapy?
What is the primary goal of pharmacological therapy in the management of pulmonary embolism?
What is the primary goal of pharmacological therapy in the management of pulmonary embolism?
Which of the following is NOT a contraindication for thrombolytic therapy?
Which of the following is NOT a contraindication for thrombolytic therapy?
What is the primary advantage of using low-molecular-weight heparin (LMWH) over unfractionated heparin in the prevention of DVT?
What is the primary advantage of using low-molecular-weight heparin (LMWH) over unfractionated heparin in the prevention of DVT?
Which of the following is a complication of hemorrhage?
Which of the following is a complication of hemorrhage?
What is the primary goal of nursing interventions in the management of hemorrhage?
What is the primary goal of nursing interventions in the management of hemorrhage?
Which of the following is a sign of hemorrhage?
Which of the following is a sign of hemorrhage?
What is the primary goal of thrombolytic therapy in the management of pulmonary embolism?
What is the primary goal of thrombolytic therapy in the management of pulmonary embolism?
Which of the following is a classification of hemorrhage?
Which of the following is a classification of hemorrhage?
What is the primary advantage of using heparin in the prevention of DVT?
What is the primary advantage of using heparin in the prevention of DVT?
Which of the following is a WHO grading of hemorrhage?
Which of the following is a WHO grading of hemorrhage?
Flashcards are hidden until you start studying
Study Notes
Post-Operative Complications: Hemorrhage and Deep Vein Thrombosis
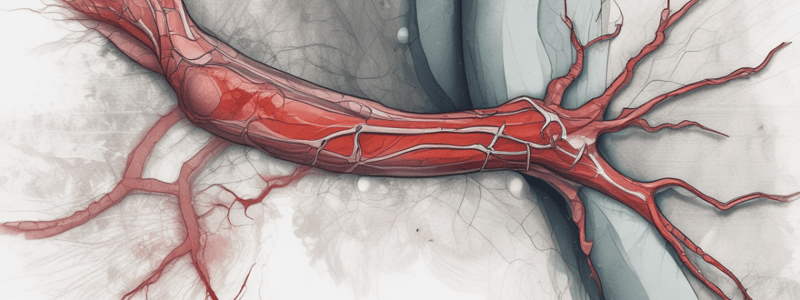
Deep Vein Thrombosis (DVT)
- Blood clot in a deep vein, most serious complication
- Clot can dislodge and travel to the lungs, a medical emergency
- Range in size from 1 mm in diameter to a mass that can completely obstruct the vein
- Deep veins are thin walled and run parallel to arteries with unidirectional flow back to the heart
Venous Thrombus (Clot)
- Composed of RBC, WBC, Platelets, Fibrin, and a tail-like appendage
- Tail grows or propagates in the direction of blood flow
- Likes valves of veins where venous stasis occurs
- Can occlude lumen
Contributing Factors (Virchow's Triad)
- Stasis of the blood/alterations in blood flow
- Endothelial injury/vessel wall injury
- Altered blood coagulability
Predisposing Factors for DVT
- Venous Stasis:
- Bedrest, bedridden, immobilization
- Obesity
- History of varicosities
- Heart failure/shock
- Veins dilated with certain medications
- Spinal cord injury (SCI)
- Age
- Surgery (past 3 months)
- Anesthesia
- Cast
- Driving/flying
- Vessel Wall Injury:
- Fractures and dislocations
- Diseases of veins
- Trauma
- Chemical irritation
- Central venous catheters
- Repetitive motion injury
- Altered Blood Coagulability:
- Blood dyscrasia
- Oral contraceptives (OCP)
- Hormone replacement therapy (HRT)
- Polycythemias
- Deficient blood volume
- Stress response
- Others:
- Pregnancy
- Cancer
- Smoking
- Height
- Family history
- History of DVT + PE
Upper Extremity Venous Thrombosis
- Less common than lower extremity
- Reasons: IV catheters, disease states, trauma, dialysis catheters, central lines, and effort thrombosis
Prophylaxis (Prevention)
- Doctor's orders
- Anticoagulation:
- Unfractionated Heparin (UFH) or Low Molecular Weight Heparin (LMWH)
- Can decrease risk of DVT by up to 50%
- Mechanical:
- Intermittent pneumatic compression device
- Graduated compression stockings
Clinical Manifestations
- Superficial Veins:
- Pain/tenderness
- Redness
- Warmth
- Most dissolve spontaneously
- Deep Vein Thrombosis (DVT):
- No symptoms to nonspecific
- Tenderness affected limb
- Pain
- Edema/Swelling
- Discoloration or redness
- Increased skin temperature
- Superficial veins prominent
Suspected DVT
- Report immediately
- Nurse can elevate leg but avoid pressure on suspected thrombus area
- No massage area
- Homan's Sign on calf pain or dorsiflexion contraindicated when DVT suspected
Diagnostics
- Duplex Ultrasonography
- D-dimer Blood Test
- Contrast Venography
- MRI/CT
Goal of DVT Management
- Stop the clot from getting any bigger
- Prevent the clot from breaking loose and causing a pulmonary embolism (PE)
- Reduce the chance of deep vein thrombosis again
- Prevent Post-Thrombotic Syndrome (PTS)
Treatment Options
- Pharmacological Therapy:
- Anticoagulant Therapy
- Thromboembolytic Therapy
- Surgical Management:
- Thrombectomy
- Catheter-Directed Thrombolysis
- IVC filter
- Ligation, clips
Anticoagulation Agents
- Unfractionated Heparin (UFH)
- Prevent extension or development of new thrombi
- Intermittent or continuous IV infusion for 5 days
- Low Molecular Weight Heparin (LMWH)
- Used for some DVTs, prevents extension or new thrombi
- Longer half-life, given SQ, decreased risk of HIT
- Fondaparinux (Arixtra)
- Synthetic inhibitor of factor Xa
- Treats and prevents DVT and PE
- No reversal agent, never causes HIT
Anticoagulation Therapy Monitoring
- Bleeding
- Thrombocytopenia
- Heparin induced thrombocytopenia (HIT)
- Regular monitoring of blood levels, counts, and INR
Teaching
- Self-injections – site and technique
- Avoid injury
- Signs and symptoms to report
- Medications interactions
- Diet
- Routine monitoring required
- Communicate anticoagulation to all other HCP
Client Comfort and Healing
- Adjuncts to therapy: activity, elevation, warm moist packs, analgesics
- Walking preferred over sitting/standing
- Bed exercises
- Hydration
Pulmonary Embolism (PE)
- Collection of particulate matter (solids, liquid, gaseous) enters systemic venous circulation and lodges in pulmonary vessels
- Obstructs pulmonary circulation causing impaired gas exchange, constriction of regional blood vessels, and bronchioles
- Decreases oxygenation
- Can be fatal
- Caused by blood clot, foreign body, tumor, fat emboli, amniotic fluid, pus
PE Risk Factors
- Immobilization/paralyzed
- Surgery
- Trauma
- Increased blood coagulation
- History of varicose vein(s)
- Obesity, smoking, pregnancy, OCP, CHF, stroke
- History
- Age
- Septic
- Cancer + therapy
PE Pathway
- Deep veins of the legs
- Most lethal from femoral or iliac veins
- Right side of heart and upper extremities
- Pelvic veins
Signs and Symptoms (PE)
- Dyspnea
- Tachypnea
- Tachycardia
- Chest pain/chest wall tenderness
- Syncope
- Diaphoresis
- Anxiety/apprehension
- Cough/hemoptysis
- Hemoptysis
Diagnostic Tests and Assessment
- Computed tomographic pulmonary angiography
- Ventilation-perfusion scan (V/Q)
- Pulmonary angiography
- MRI
- CXR
- ECG
- Peripheral vascular studies
- ABG's
Interventions
- Goals: increase alveolar gas exchange, improve tissue perfusion, get rid of embolism, prevent complications
- Pharmacological Therapy:
- Anticoagulation
- Thrombolytics
- Surgical Management:
- Embolectomy
- Clips
- Filter
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.