Podcast
Questions and Answers
What is the primary method to obtain a pleural fluid sample for culture in cases of pleural effusion?
What is the primary method to obtain a pleural fluid sample for culture in cases of pleural effusion?
- Ultrasound-guided aspiration
- Chest X-ray
- Bronchoscopy
- Thoracentesis (correct)
In the context of treating community-acquired pneumonia, which of the following therapies is considered for patients who are previously healthy and lack comorbidities?
In the context of treating community-acquired pneumonia, which of the following therapies is considered for patients who are previously healthy and lack comorbidities?
- Doxycycline or a macrolide (correct)
- Piperacillin-tazobactam
- Ceftazidime with Azithromycin
- Vancomycin
What treatment should be initiated if a patient with pneumonia is found to be hypoxic?
What treatment should be initiated if a patient with pneumonia is found to be hypoxic?
- External oxygen therapy (correct)
- Antibiotics only
- IV fluids
- Oral corticosteroids
Which diagnostic procedure may be necessary if the treatment for pneumonia is deemed inefficient?
Which diagnostic procedure may be necessary if the treatment for pneumonia is deemed inefficient?
What factor is NOT involved in patient stratification for pneumonia therapy?
What factor is NOT involved in patient stratification for pneumonia therapy?
What is the recommended approach for patients being prepared for the possibility of atypical infections?
What is the recommended approach for patients being prepared for the possibility of atypical infections?
What is the purpose of draining fluids in patients with pleural effusion?
What is the purpose of draining fluids in patients with pleural effusion?
Which of the following conditions would most likely require intravenous fluids for dehydration management?
Which of the following conditions would most likely require intravenous fluids for dehydration management?
Which type of pneumonia can occur in patients who have not been hospitalized or lived in a nursing home during the two weeks prior to symptom onset?
Which type of pneumonia can occur in patients who have not been hospitalized or lived in a nursing home during the two weeks prior to symptom onset?
What is a common complication associated with Hospital-acquired Pneumonia (HAP)?
What is a common complication associated with Hospital-acquired Pneumonia (HAP)?
What is a major risk factor for developing Ventilator-associated Pneumonia (VAP)?
What is a major risk factor for developing Ventilator-associated Pneumonia (VAP)?
Which organism is most commonly associated with Community-acquired Pneumonia (CAP)?
Which organism is most commonly associated with Community-acquired Pneumonia (CAP)?
Which of the following is NOT considered a general symptom of pneumonia?
Which of the following is NOT considered a general symptom of pneumonia?
Which type of pneumonia occurs more than 48 hours after hospital admission?
Which type of pneumonia occurs more than 48 hours after hospital admission?
Which of the following bacterial organisms is least likely to cause pneumonia in the community setting?
Which of the following bacterial organisms is least likely to cause pneumonia in the community setting?
What is a significant risk factor for developing pneumonia among hospitalized patients?
What is a significant risk factor for developing pneumonia among hospitalized patients?
Which combination of medications is appropriate for patients with comorbidities and recent antibiotic use?
Which combination of medications is appropriate for patients with comorbidities and recent antibiotic use?
What is the minimum duration of antimicrobial therapy for CAP once identified?
What is the minimum duration of antimicrobial therapy for CAP once identified?
Which condition is characterized by uncontrolled inflammation in the body and may lead to widespread organ failure?
Which condition is characterized by uncontrolled inflammation in the body and may lead to widespread organ failure?
Which of the following signs is NOT required to consider discontinuation of therapy?
Which of the following signs is NOT required to consider discontinuation of therapy?
What is typically required for a diagnosis of pneumonia that shows multiple lobes involved on an X-ray?
What is typically required for a diagnosis of pneumonia that shows multiple lobes involved on an X-ray?
How is ventilator-associated pneumonia (VAP) defined?
How is ventilator-associated pneumonia (VAP) defined?
Which of the following is a major criterion indicating the need for ICU admission in pneumonia patients?
Which of the following is a major criterion indicating the need for ICU admission in pneumonia patients?
Which factor is indicative of health-associated pneumonia (HCAP)?
Which factor is indicative of health-associated pneumonia (HCAP)?
What severe form of respiratory failure may occur as a result of severe pneumonia?
What severe form of respiratory failure may occur as a result of severe pneumonia?
What is the prevalence of hospital-acquired infections that are classified as HAP?
What is the prevalence of hospital-acquired infections that are classified as HAP?
Which clinical sign indicates CAP-associated instability before therapy is discontinued?
Which clinical sign indicates CAP-associated instability before therapy is discontinued?
Which laboratory finding is indicative of possible serious pneumonia severity?
Which laboratory finding is indicative of possible serious pneumonia severity?
Which of the following is not directly associated with pneumonia's complications?
Which of the following is not directly associated with pneumonia's complications?
What constitutes an inadequate response to initial pneumonia therapy?
What constitutes an inadequate response to initial pneumonia therapy?
Which clinical observation can suggest the need for further microbiologic evaluation in pneumonia?
Which clinical observation can suggest the need for further microbiologic evaluation in pneumonia?
Which option is most closely linked with the evaluation of pneumonia severity in patients?
Which option is most closely linked with the evaluation of pneumonia severity in patients?
Which antibiotics are typically used for treating Ventilator-associated pneumonia caused by Pseudomonas aeruginosa?
Which antibiotics are typically used for treating Ventilator-associated pneumonia caused by Pseudomonas aeruginosa?
What is a significant risk factor for the development of Hospital-acquired pneumonia?
What is a significant risk factor for the development of Hospital-acquired pneumonia?
Which of the following conditions does NOT increase the risk for drug-resistant pathogens in pneumonia?
Which of the following conditions does NOT increase the risk for drug-resistant pathogens in pneumonia?
What factor would necessitate the addition of an anti-MRSA agent during pneumonia treatment?
What factor would necessitate the addition of an anti-MRSA agent during pneumonia treatment?
Which complication might arise from pneumonia that involves the lung structure?
Which complication might arise from pneumonia that involves the lung structure?
What is a common misconception about the use of corticosteroids in pneumonia treatment?
What is a common misconception about the use of corticosteroids in pneumonia treatment?
Which underlying disease is often associated with a higher risk of pneumonia complications?
Which underlying disease is often associated with a higher risk of pneumonia complications?
Which of the following would NOT be classified as a wrong diagnosis-related complication in pneumonia?
Which of the following would NOT be classified as a wrong diagnosis-related complication in pneumonia?
Study Notes
Definition and Classification
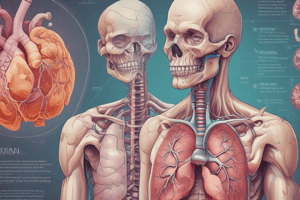
- Pneumonia is an infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus.
- Classified by the setting of acquisition:
- Community-Acquired Pneumonia (CAP): Develops in patients not recently hospitalized or residing in nursing homes.
- Hospital-Acquired Pneumonia (HAP): Occurs 48 hours or more after admission, not incubating at the time.
- Other types include:
- Ventilator-Associated Pneumonia (VAP)
- Health-Associated Pneumonia (HCAP)
Pathogens
- Bacterial: Includes anaerobic bacteria, intracellular pathogens, and multiple gram-positive and gram-negative bacteria.
- Common agents: Streptococcus pneumoniae (30-40%), Staphylococcus aureus, Haemophilus influenzae (2-11%), and Legionella pneumophila (1-16%).
- Viral: Examples include RSV, CMV, influenza, and herpes viruses.
- Fungal: Involves fungi as causative agents.
- Protozoal: Notable agents include Pneumocystis Carinii and Toxoplasma.
- Rickettsial: Includes organisms responsible for Typhus and Q Fever.
Clinical Picture
- General Symptoms: Malaise, fever, rigors, myalgia, fatigue, body aches, loss of appetite.
- Specific Symptoms: Cough, sputum production, dyspnea, pleuritic chest pain, hemoptysis.
- General Signs: Cyanosis, herpes labialis, tachypnea (resp >20 breaths/min), tachycardia.
- Local Findings: Signs of lung consolidation (e.g., bronchial breathing, crepitations), pleural rub in dry pleuritis.
Diagnosis
- Diagnostic methods may include:
- Serologic Testing: For atypical bacteria and viruses.
- Urinary Antigen Tests: For Legionella pneumophila and Streptococcus pneumoniae.
- Invasive Procedures: Bronchoscopy may be warranted if treatments fail; thoracentesis for pleural effusion sampling.
- Imaging: Chest X-ray is crucial for diagnosis and assessing pneumonia extent; CT scans can provide additional details.
Management
- Empirical therapy initiated according to established guidelines until culture results are available.
- Consider atypical infections in treatment plans.
- Patient stratification based on:
- ICU needs
- Preexisting cardiopulmonary conditions
- Other risk factors.
Treatment Protocols
- For Previously Healthy Patients: Use macrolides (e.g., Azithromycin) or doxycycline.
- For Patients with Comorbidities:
- Respiratory fluoroquinolone (e.g., Levofloxacin, Moxifloxacin).
- Combination therapy of a B-lactam with a macrolide.
- For severe cases, add vancomycin or linezolid.
Treatment Duration
- Minimum treatment duration of 5 days, with discharge criteria including:
- Afebrile for 48-72 hours.
- No more than one CAP-associated instability sign.
- Stable vital signs and ability to maintain oral intake.
Complications
- Severe potential complications include:
- Empyema, lung abscess, respiratory failure, sepsis.
- Extra thoracic complications like arthritis, meningitis, and renal failure.
Prognosis Indicators
- Pneumonia Severity Score influenced by:
- Elevated blood urea.
- White blood cell count extremes (<4000 or >30000).
- Low serum albumin (<3.5 gm).
- Multiple affected lobes on X-ray.
Evaluation Process
- Requires clinical, laboratory, and radiographic evaluations to confirm diagnosis and rule out complications.
- Additional microbiologic evaluation necessary in cases of suspected resistant pathogens or special risk factors (like diabetes or COPD).
Key Considerations
- Focus on avoiding misdiagnosis and considering drug-resistant organisms.
- Be aware of chronic conditions that may affect treatment adequacy and pneumonia resolution.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz will help you understand pneumonia by defining its classifications and clinical manifestations. You will explore various types of pneumonia, including bacterial, viral, and fungal, and identify management plans for both Hospital-Acquired Pneumonia (HAP) and Community-Acquired Pneumonia (CAP). Test your knowledge and enhance your understanding of this important respiratory condition.