Podcast
Questions and Answers
Which part of the pituitary gland secretes growth hormone?
Which part of the pituitary gland secretes growth hormone?
- Anterior pituitary (correct)
- Adrenal gland
- Posterior pituitary
- Hypothalamus
Which hormone is crucial for inducing labor?
Which hormone is crucial for inducing labor?
- Growth hormone
- Oxytocin (correct)
- Vasopressin
- Prolactin
Vasopressin increases water reabsorption by acting on which type of receptors?
Vasopressin increases water reabsorption by acting on which type of receptors?
- V1 receptors
- Alpha receptors
- V2 receptors (correct)
- Beta receptors
The term adenohypophysis refers to which component of the pituitary gland?
The term adenohypophysis refers to which component of the pituitary gland?
Which condition arises from a deficiency of growth hormone during childhood?
Which condition arises from a deficiency of growth hormone during childhood?
In adults, a deficiency of growth hormone can cause which of the following symptoms?
In adults, a deficiency of growth hormone can cause which of the following symptoms?
Growth hormone mainly exerts its effects through which mediator?
Growth hormone mainly exerts its effects through which mediator?
What is a common medical use for synthetic growth hormone (somatotropin) in children?
What is a common medical use for synthetic growth hormone (somatotropin) in children?
Which receptor does Bromocriptine specifically bind to in order to reduce hormone secretion?
Which receptor does Bromocriptine specifically bind to in order to reduce hormone secretion?
Bromocriptine is primarily indicated for the treatment of which type of pituitary tumor?
Bromocriptine is primarily indicated for the treatment of which type of pituitary tumor?
Oxytocin is most commonly used to achieve which physiological result during pregnancy?
Oxytocin is most commonly used to achieve which physiological result during pregnancy?
What is a recognized clinical application of oxytocin after delivery?
What is a recognized clinical application of oxytocin after delivery?
Which technique is commonly used to administer oxytocin for labor induction?
Which technique is commonly used to administer oxytocin for labor induction?
Vasopressin primarily enhances water reabsorption in the kidneys by acting on which receptor?
Vasopressin primarily enhances water reabsorption in the kidneys by acting on which receptor?
In patients with central diabetes insipidus, what condition is vasopressin used to manage?
In patients with central diabetes insipidus, what condition is vasopressin used to manage?
Desmopressin (DDAVP) mainly functions by acting on which receptors to decrease urine output in diabetes insipidus?
Desmopressin (DDAVP) mainly functions by acting on which receptors to decrease urine output in diabetes insipidus?
What is the primary indication for desmopressin therapy besides diabetes insipidus?
What is the primary indication for desmopressin therapy besides diabetes insipidus?
Which condition is a contraindication to the use of desmopressin?
Which condition is a contraindication to the use of desmopressin?
What side effect is most commonly associated with desmopressin therapy?
What side effect is most commonly associated with desmopressin therapy?
What distinguishes desmopressin from vasopressin concerning receptor selectivity?
What distinguishes desmopressin from vasopressin concerning receptor selectivity?
Which of the following is NOT an application of desmopressin in clinical settings?
Which of the following is NOT an application of desmopressin in clinical settings?
Which condition is not effectively treated using synthetic growth hormone in adults?
Which condition is not effectively treated using synthetic growth hormone in adults?
What serious side effect is most commonly associated with the use of somatotropin in children?
What serious side effect is most commonly associated with the use of somatotropin in children?
Which of the following statements about Octreotide is true?
Which of the following statements about Octreotide is true?
What distinguishes Pegvisomant from other growth hormone therapies?
What distinguishes Pegvisomant from other growth hormone therapies?
Which hormone secretion is Bromocriptine primarily intended to reduce?
Which hormone secretion is Bromocriptine primarily intended to reduce?
Which condition would somatostatin (Octreotide) not be used to treat?
Which condition would somatostatin (Octreotide) not be used to treat?
How is Pegvisomant administered for effective treatment?
How is Pegvisomant administered for effective treatment?
What is a typical side effect reported with somatostatin analogs like Octreotide?
What is a typical side effect reported with somatostatin analogs like Octreotide?
In the context of hypothyroidism, what is the primary goal of levothyroxine therapy?
In the context of hypothyroidism, what is the primary goal of levothyroxine therapy?
What is the significance of monitoring pregnant women with hypothyroidism more frequently during treatment?
What is the significance of monitoring pregnant women with hypothyroidism more frequently during treatment?
What is the recommended target range for TSH levels in patients receiving levothyroxine replacement therapy?
What is the recommended target range for TSH levels in patients receiving levothyroxine replacement therapy?
In which population is it particularly important to start with a lower dose of levothyroxine to minimize the risk of overtreatment?
In which population is it particularly important to start with a lower dose of levothyroxine to minimize the risk of overtreatment?
What common risk is associated with undertreating hypothyroidism in pregnant women?
What common risk is associated with undertreating hypothyroidism in pregnant women?
What is the recommended starting dose of levothyroxine for a patient over 50 years old with no known cardiac disease?
What is the recommended starting dose of levothyroxine for a patient over 50 years old with no known cardiac disease?
What is one of the goals of levothyroxine therapy in patients with goiter?
What is one of the goals of levothyroxine therapy in patients with goiter?
What condition can potentially arise from a significant increase in TSH levels in untreated hypothyroidism?
What condition can potentially arise from a significant increase in TSH levels in untreated hypothyroidism?
In which situation are alpha-glucosidase inhibitors specifically contraindicated?
In which situation are alpha-glucosidase inhibitors specifically contraindicated?
What is the main reason for contraindication of alpha-glucosidase inhibitors in patients with inflammatory bowel disease?
What is the main reason for contraindication of alpha-glucosidase inhibitors in patients with inflammatory bowel disease?
To achieve optimal glucose control, when should alpha-glucosidase inhibitors be administered?
To achieve optimal glucose control, when should alpha-glucosidase inhibitors be administered?
What is the approximate reduction in A1c levels achieved by alpha-glucosidase inhibitors in patients with type 2 diabetes?
What is the approximate reduction in A1c levels achieved by alpha-glucosidase inhibitors in patients with type 2 diabetes?
When treating hypoglycemia in patients taking alpha-glucosidase inhibitors, what is the preferred method?
When treating hypoglycemia in patients taking alpha-glucosidase inhibitors, what is the preferred method?
Which laboratory test should be monitored regularly in patients on alpha-glucosidase inhibitors?
Which laboratory test should be monitored regularly in patients on alpha-glucosidase inhibitors?
Why might post-meal self-monitoring of blood glucose be recommended for some patients taking alpha-glucosidase inhibitors?
Why might post-meal self-monitoring of blood glucose be recommended for some patients taking alpha-glucosidase inhibitors?
What side effect has been commonly associated with the use of alpha-glucosidase inhibitors?
What side effect has been commonly associated with the use of alpha-glucosidase inhibitors?
What potential concern is associated with the use of certain therapies regarding cancer risk?
What potential concern is associated with the use of certain therapies regarding cancer risk?
Which physiological process does SGLT2 inhibition primarily facilitate in the context of diabetes management?
Which physiological process does SGLT2 inhibition primarily facilitate in the context of diabetes management?
How do SGLT2 inhibitors impact urinary glucose levels?
How do SGLT2 inhibitors impact urinary glucose levels?
In patients with diabetes, SGLT2 inhibitors are especially beneficial for those with which accompanying health conditions?
In patients with diabetes, SGLT2 inhibitors are especially beneficial for those with which accompanying health conditions?
Which of the following best describes a common effect of DPP-4 inhibitors in relation to cancer risk?
Which of the following best describes a common effect of DPP-4 inhibitors in relation to cancer risk?
Alpha-glucosidase inhibitors should be avoided in patients with a serum creatinine level greater than what value?
Alpha-glucosidase inhibitors should be avoided in patients with a serum creatinine level greater than what value?
What is the primary mechanism through which DPP-4 inhibitors lower blood glucose in patients with type 2 diabetes?
What is the primary mechanism through which DPP-4 inhibitors lower blood glucose in patients with type 2 diabetes?
Which incretin hormones are primarily impacted by DPP-4 inhibitors?
Which incretin hormones are primarily impacted by DPP-4 inhibitors?
Which is a significant advantage of using DPP-4 inhibitors in diabetes management?
Which is a significant advantage of using DPP-4 inhibitors in diabetes management?
What adverse effect is commonly associated with the use of DPP-4 inhibitors?
What adverse effect is commonly associated with the use of DPP-4 inhibitors?
Which of the following statements best describes the effect of DPP-4 inhibitors on insulin secretion?
Which of the following statements best describes the effect of DPP-4 inhibitors on insulin secretion?
What is the key reason for monitoring patients on DPP-4 inhibitors for adverse effects?
What is the key reason for monitoring patients on DPP-4 inhibitors for adverse effects?
Which option is NOT a characteristic of DPP-4 inhibitors?
Which option is NOT a characteristic of DPP-4 inhibitors?
Which drug is favored for inhibiting the conversion of T4 to T3 in peripheral tissues?
Which drug is favored for inhibiting the conversion of T4 to T3 in peripheral tissues?
In what clinical scenario is Propylthiouracil (PTU) the preferred treatment?
In what clinical scenario is Propylthiouracil (PTU) the preferred treatment?
What is the typical initial maintenance dose of Methimazole for hyperthyroidism?
What is the typical initial maintenance dose of Methimazole for hyperthyroidism?
Why is Methimazole contraindicated during the first trimester of pregnancy?
Why is Methimazole contraindicated during the first trimester of pregnancy?
How long does it generally take for T4 and T3 hormone levels to decrease after initiating Methimazole treatment?
How long does it generally take for T4 and T3 hormone levels to decrease after initiating Methimazole treatment?
What is the mechanism of action of Methimazole in hyperthyroidism treatment?
What is the mechanism of action of Methimazole in hyperthyroidism treatment?
What key advantage does Propylthiouracil (PTU) have over Methimazole when treating thyroid storm?
What key advantage does Propylthiouracil (PTU) have over Methimazole when treating thyroid storm?
Why might a clinician choose Methimazole over PTU for most hyperthyroidism cases?
Why might a clinician choose Methimazole over PTU for most hyperthyroidism cases?
What role does amylin play in postprandial glucose control?
What role does amylin play in postprandial glucose control?
Which of the following is a defining feature of Type 2 Diabetes Mellitus?
Which of the following is a defining feature of Type 2 Diabetes Mellitus?
In which scenario would glucagon secretion be suppressed most effectively?
In which scenario would glucagon secretion be suppressed most effectively?
What is the typical timeframe for diagnosing gestational diabetes?
What is the typical timeframe for diagnosing gestational diabetes?
Which of the following is NOT a criterion for diagnosing diabetes?
Which of the following is NOT a criterion for diagnosing diabetes?
Which type of diabetes is characterized by the condition known as MODY?
Which type of diabetes is characterized by the condition known as MODY?
What is the main cause of secondary diabetes?
What is the main cause of secondary diabetes?
What percentage of diabetes cases are attributed to Type 1 Diabetes Mellitus?
What percentage of diabetes cases are attributed to Type 1 Diabetes Mellitus?
Which of the following therapies is considered second-line for Type 2 Diabetes Mellitus, following metformin?
Which of the following therapies is considered second-line for Type 2 Diabetes Mellitus, following metformin?
What effect does insulin have on glucose metabolism in the liver?
What effect does insulin have on glucose metabolism in the liver?
Which of the following hormones is primarily responsible for stimulating gluconeogenesis in the liver?
Which of the following hormones is primarily responsible for stimulating gluconeogenesis in the liver?
What is the primary function of Dipeptidyl peptidase-4 (DPP-4) in relation to GLP-1?
What is the primary function of Dipeptidyl peptidase-4 (DPP-4) in relation to GLP-1?
Which of the following effects is associated with glucagon-like peptide 1 (GLP-1)?
Which of the following effects is associated with glucagon-like peptide 1 (GLP-1)?
Which of the following actions does insulin perform in adipose tissue?
Which of the following actions does insulin perform in adipose tissue?
What role does glucagon play in fat metabolism?
What role does glucagon play in fat metabolism?
In response to low blood glucose levels, which hormone acts primarily to elevate glucose concentrations?
In response to low blood glucose levels, which hormone acts primarily to elevate glucose concentrations?
What factors should be considered when selecting an antidepressant for a patient?
What factors should be considered when selecting an antidepressant for a patient?
What is the primary goal of acute treatment with antidepressants in patients with depression?
What is the primary goal of acute treatment with antidepressants in patients with depression?
How long is an adequate trial period for antidepressant efficacy assessment?
How long is an adequate trial period for antidepressant efficacy assessment?
For a patient with a history of multiple serious depressive episodes, what treatment approach is suggested?
For a patient with a history of multiple serious depressive episodes, what treatment approach is suggested?
Which class of antidepressants carries the greatest risk of overdose?
Which class of antidepressants carries the greatest risk of overdose?
What are common symptoms associated with antidepressant discontinuation syndrome?
What are common symptoms associated with antidepressant discontinuation syndrome?
Which antidepressant class is predominantly prescribed for managing major depressive disorder (MDD)?
Which antidepressant class is predominantly prescribed for managing major depressive disorder (MDD)?
What is a crucial aspect when reviewing a patient's history before prescribing antidepressants?
What is a crucial aspect when reviewing a patient's history before prescribing antidepressants?
What is the likely mechanism of action for many antidepressants?
What is the likely mechanism of action for many antidepressants?
Which neurotransmitter is primarily targeted by selective serotonin reuptake inhibitors (SSRIs)?
Which neurotransmitter is primarily targeted by selective serotonin reuptake inhibitors (SSRIs)?
Why do most antidepressants require several weeks before they show effectiveness?
Why do most antidepressants require several weeks before they show effectiveness?
What does the monoamine hypothesis suggest regarding the cause of depression?
What does the monoamine hypothesis suggest regarding the cause of depression?
Which evidence supports the monoamine hypothesis of depression?
Which evidence supports the monoamine hypothesis of depression?
According to the neurotrophic hypothesis, what growth factor is often found at reduced levels in depression?
According to the neurotrophic hypothesis, what growth factor is often found at reduced levels in depression?
What is the relationship between glutamate levels and depression according to recent findings?
What is the relationship between glutamate levels and depression according to recent findings?
What is the contraindicated treatment option in cases of TCA overdose due to exacerbating arrhythmias?
What is the contraindicated treatment option in cases of TCA overdose due to exacerbating arrhythmias?
Which mechanism of action is specifically associated with serotonin-norepinephrine reuptake inhibitors (SNRIs)?
Which mechanism of action is specifically associated with serotonin-norepinephrine reuptake inhibitors (SNRIs)?
Which SNRI is recognized for its effectiveness in treating both depression and neuropathic pain?
Which SNRI is recognized for its effectiveness in treating both depression and neuropathic pain?
What is the recommended approach to SNRI dosing in patients with renal insufficiency?
What is the recommended approach to SNRI dosing in patients with renal insufficiency?
What side effect is commonly noted among patients taking SNRIs?
What side effect is commonly noted among patients taking SNRIs?
Which effect is typically observed with increased dosages of SNRIs?
Which effect is typically observed with increased dosages of SNRIs?
Why is it advised to avoid the combination of SNRIs with monoamine oxidase inhibitors (MAOIs)?
Why is it advised to avoid the combination of SNRIs with monoamine oxidase inhibitors (MAOIs)?
What additional condition is venlafaxine used to manage besides major depression?
What additional condition is venlafaxine used to manage besides major depression?
Which class of antidepressants is primarily used for treating major depressive disorder and anxiety disorders?
Which class of antidepressants is primarily used for treating major depressive disorder and anxiety disorders?
What is the primary goal of acute treatment with antidepressants for a patient experiencing depression?
What is the primary goal of acute treatment with antidepressants for a patient experiencing depression?
How long is it generally expected to take before a patient notices maximum benefits from antidepressant therapy?
How long is it generally expected to take before a patient notices maximum benefits from antidepressant therapy?
For patients who have experienced two or more serious episodes of major depressive disorder in the last five years, what treatment approach is advised?
For patients who have experienced two or more serious episodes of major depressive disorder in the last five years, what treatment approach is advised?
Which antidepressants are known to be potent inhibitors of CYP2D6, which can cause significant drug interactions?
Which antidepressants are known to be potent inhibitors of CYP2D6, which can cause significant drug interactions?
Which antidepressants are relatively free from significant drug interactions?
Which antidepressants are relatively free from significant drug interactions?
What is a serious contraindication when using selective serotonin reuptake inhibitors (SSRIs)?
What is a serious contraindication when using selective serotonin reuptake inhibitors (SSRIs)?
What are the hallmark signs of serotonin syndrome?
What are the hallmark signs of serotonin syndrome?
What is one clinical effect of antidepressants related to the neurotrophic hypothesis?
What is one clinical effect of antidepressants related to the neurotrophic hypothesis?
What hormonal dysregulation is frequently seen in patients with depression according to the neuroendocrine hypothesis?
What hormonal dysregulation is frequently seen in patients with depression according to the neuroendocrine hypothesis?
Most antidepressants work by increasing the concentration of which neurotransmitter(s) in the synaptic cleft?
Most antidepressants work by increasing the concentration of which neurotransmitter(s) in the synaptic cleft?
How do selective serotonin reuptake inhibitors (SSRIs) alleviate symptoms of depression?
How do selective serotonin reuptake inhibitors (SSRIs) alleviate symptoms of depression?
Why do antidepressants typically take several weeks to show clinical efficacy?
Why do antidepressants typically take several weeks to show clinical efficacy?
What risk is associated with antidepressant use in patients younger than 25 according to the FDA warning?
What risk is associated with antidepressant use in patients younger than 25 according to the FDA warning?
For which trimester of pregnancy is there an association between antidepressant use and low birth weight and premature delivery?
For which trimester of pregnancy is there an association between antidepressant use and low birth weight and premature delivery?
Which statement is most accurate regarding the mechanisms of antidepressants?
Which statement is most accurate regarding the mechanisms of antidepressants?
What is the primary composition of Humalog Mix 75/25?
What is the primary composition of Humalog Mix 75/25?
Combination insulin products are typically designed to control which types of blood glucose levels?
Combination insulin products are typically designed to control which types of blood glucose levels?
The Glargine/Lixisenatide combination insulin therapy functions primarily through which mechanism?
The Glargine/Lixisenatide combination insulin therapy functions primarily through which mechanism?
Inhaled insulin (Afrezza) is primarily utilized for which condition?
Inhaled insulin (Afrezza) is primarily utilized for which condition?
What is a major contraindication for administering inhaled insulin?
What is a major contraindication for administering inhaled insulin?
Inhaled insulin is associated with a boxed warning for which specific condition?
Inhaled insulin is associated with a boxed warning for which specific condition?
What is recognized as the most common adverse effect related to insulin therapy?
What is recognized as the most common adverse effect related to insulin therapy?
Which insulin-related complication is known to cause significant weight gain?
Which insulin-related complication is known to cause significant weight gain?
Which transporter is primarily responsible for glucose uptake in skeletal muscle and adipose tissue?
Which transporter is primarily responsible for glucose uptake in skeletal muscle and adipose tissue?
What impact does insulin have on protein metabolism in skeletal muscle?
What impact does insulin have on protein metabolism in skeletal muscle?
In which tissue does insulin primarily enhance triglyceride storage?
In which tissue does insulin primarily enhance triglyceride storage?
What occurs to protein catabolism levels in the body when insulin levels rise?
What occurs to protein catabolism levels in the body when insulin levels rise?
How does insulin influence triglyceride and VLDL synthesis?
How does insulin influence triglyceride and VLDL synthesis?
Which organ is crucial for insulin-mediated glycogen synthesis?
Which organ is crucial for insulin-mediated glycogen synthesis?
What is the primary metabolic function of insulin in the liver?
What is the primary metabolic function of insulin in the liver?
What effect does insulin have on glycogen synthesis in skeletal muscle under its influence?
What effect does insulin have on glycogen synthesis in skeletal muscle under its influence?
What is the primary role of tracking 'time in range' (TIR) in diabetes management?
What is the primary role of tracking 'time in range' (TIR) in diabetes management?
Which parameter describes the duration that glucose levels exceed the target range?
Which parameter describes the duration that glucose levels exceed the target range?
Which benefit does continuous glucose monitoring (CGM) provide for diabetes management?
Which benefit does continuous glucose monitoring (CGM) provide for diabetes management?
What significant function does continuous glucose monitoring (CGM) serve in managing diabetes?
What significant function does continuous glucose monitoring (CGM) serve in managing diabetes?
Which metric evaluates the effectiveness of glucose levels being maintained within a target range?
Which metric evaluates the effectiveness of glucose levels being maintained within a target range?
Which group of patients would benefit most from the use of continuous glucose monitoring (CGM)?
Which group of patients would benefit most from the use of continuous glucose monitoring (CGM)?
What is a significant consideration for healthcare providers when assessing self-monitoring of blood glucose (SMBG) supplies?
What is a significant consideration for healthcare providers when assessing self-monitoring of blood glucose (SMBG) supplies?
What is the most common misconception about continuous glucose monitoring (CGM)?
What is the most common misconception about continuous glucose monitoring (CGM)?
Which hormone primarily works to lower the plasma glucose levels after meal intake?
Which hormone primarily works to lower the plasma glucose levels after meal intake?
Which condition is NOT an indication for insulin therapy?
Which condition is NOT an indication for insulin therapy?
Which enzyme plays a crucial role in the degradation of GLP-1?
Which enzyme plays a crucial role in the degradation of GLP-1?
What is one significant advantage of using recombinant DNA technology for insulin production?
What is one significant advantage of using recombinant DNA technology for insulin production?
Which of the following is a major effect of insulin on adipose tissue?
Which of the following is a major effect of insulin on adipose tissue?
What occurs to triglyceride levels in the presence of high insulin levels?
What occurs to triglyceride levels in the presence of high insulin levels?
Which hormone is secreted by the pancreas that raises blood glucose levels?
Which hormone is secreted by the pancreas that raises blood glucose levels?
What is the main metabolic action of insulin in the liver?
What is the main metabolic action of insulin in the liver?
Which GLP-1 agonist should be used cautiously in patients with renal insufficiency due to risk of gastrointestinal side effects?
Which GLP-1 agonist should be used cautiously in patients with renal insufficiency due to risk of gastrointestinal side effects?
What major side effect of pramlintide therapy leads to a boxed warning?
What major side effect of pramlintide therapy leads to a boxed warning?
What is the effect of pramlintide on postprandial glucose levels?
What is the effect of pramlintide on postprandial glucose levels?
How should mealtime insulin doses be adjusted when starting pramlintide therapy?
How should mealtime insulin doses be adjusted when starting pramlintide therapy?
In which patients is pramlintide indicated?
In which patients is pramlintide indicated?
What is the primary route of administration for pramlintide?
What is the primary route of administration for pramlintide?
Pramlintide is an analog of which natural hormone?
Pramlintide is an analog of which natural hormone?
What secondary effect does pramlintide have aside from reducing postprandial glucose levels?
What secondary effect does pramlintide have aside from reducing postprandial glucose levels?
What is a major limitation of Carbidopa/Levodopa therapy compared to dopamine agonists in Parkinson's treatment?
What is a major limitation of Carbidopa/Levodopa therapy compared to dopamine agonists in Parkinson's treatment?
Which of the following effects is specifically associated with the use of dopamine agonists in Parkinson's disease?
Which of the following effects is specifically associated with the use of dopamine agonists in Parkinson's disease?
What is a primary action of MAO-B inhibitors in the management of Parkinson's disease?
What is a primary action of MAO-B inhibitors in the management of Parkinson's disease?
Why is nausea a common side effect of MAO-B inhibitors?
Why is nausea a common side effect of MAO-B inhibitors?
Which statement about COMT inhibitors in Parkinson's therapy is accurate?
Which statement about COMT inhibitors in Parkinson's therapy is accurate?
What significant risk is associated with the use of Tolcapone as a COMT inhibitor?
What significant risk is associated with the use of Tolcapone as a COMT inhibitor?
Which characteristic is primarily observed with the side effects of COMT inhibitors?
Which characteristic is primarily observed with the side effects of COMT inhibitors?
What therapeutic benefit does Rasagiline, a MAO-B inhibitor, offer beyond its mechanism of action?
What therapeutic benefit does Rasagiline, a MAO-B inhibitor, offer beyond its mechanism of action?
COMT inhibitors are primarily used in combination with which other drug class to enhance their effectiveness?
COMT inhibitors are primarily used in combination with which other drug class to enhance their effectiveness?
Which of the following drugs specifically acts as an adenosine A2A receptor antagonist to help manage Parkinson's disease?
Which of the following drugs specifically acts as an adenosine A2A receptor antagonist to help manage Parkinson's disease?
What is a common side effect directly related to the use of adenosine A2A receptor antagonists?
What is a common side effect directly related to the use of adenosine A2A receptor antagonists?
In Parkinson's disease treatment, amantadine is used as an adjunct therapy for which specific symptoms?
In Parkinson's disease treatment, amantadine is used as an adjunct therapy for which specific symptoms?
What unique side effect is specifically associated with amantadine treatment?
What unique side effect is specifically associated with amantadine treatment?
Which symptom of Parkinson's disease is effectively targeted by antimuscarinic drugs?
Which symptom of Parkinson's disease is effectively targeted by antimuscarinic drugs?
What common side effect is experienced by patients taking antimuscarinics?
What common side effect is experienced by patients taking antimuscarinics?
Amantadine was originally developed for the treatment of which viral infection?
Amantadine was originally developed for the treatment of which viral infection?
What effect does acetylcholine have as dopamine levels decrease in Parkinson's disease?
What effect does acetylcholine have as dopamine levels decrease in Parkinson's disease?
In the context of the basal ganglia, what is the primary role of dopamine?
In the context of the basal ganglia, what is the primary role of dopamine?
What occurs to the inhibitory pathway of the basal ganglia in Parkinsonism due to dopamine deficiency?
What occurs to the inhibitory pathway of the basal ganglia in Parkinsonism due to dopamine deficiency?
Which symptom is primarily due to an imbalance between dopamine and acetylcholine in Parkinson's disease?
Which symptom is primarily due to an imbalance between dopamine and acetylcholine in Parkinson's disease?
Which neurotransmitter imbalance is crucial for the manifestation of Parkinson's disease?
Which neurotransmitter imbalance is crucial for the manifestation of Parkinson's disease?
What role does GABA play in the pathophysiology of motor dysfunction associated with Parkinsonism?
What role does GABA play in the pathophysiology of motor dysfunction associated with Parkinsonism?
In Parkinson's disease, how does a deficiency of dopamine influence GABAergic signaling?
In Parkinson's disease, how does a deficiency of dopamine influence GABAergic signaling?
What is the primary treatment goal for managing Parkinsonism?
What is the primary treatment goal for managing Parkinsonism?
Which symptom is least likely to improve with dopaminergic therapy in Parkinson's disease?
Which symptom is least likely to improve with dopaminergic therapy in Parkinson's disease?
Which of the following is a common side effect of amantadine in Parkinson's disease treatment?
Which of the following is a common side effect of amantadine in Parkinson's disease treatment?
What is the mechanism of action of amantadine in Parkinson's disease?
What is the mechanism of action of amantadine in Parkinson's disease?
Which medication used for essential tremor is associated with sedation as a side effect?
Which medication used for essential tremor is associated with sedation as a side effect?
Which type of tremor is more commonly treated with beta-blockers such as propranolol?
Which type of tremor is more commonly treated with beta-blockers such as propranolol?
Which antimuscarinic drug is commonly used in the treatment of Parkinson's tremor?
Which antimuscarinic drug is commonly used in the treatment of Parkinson's tremor?
What is the first-line treatment for essential tremor?
What is the first-line treatment for essential tremor?
Which of the following is an aggravating factor for essential tremor?
Which of the following is an aggravating factor for essential tremor?
What is the primary mechanism of action for dopamine agonists like pramipexole and ropinirole?
What is the primary mechanism of action for dopamine agonists like pramipexole and ropinirole?
What distinguishes Ropinirole from other dopamine agonists in terms of receptor specificity?
What distinguishes Ropinirole from other dopamine agonists in terms of receptor specificity?
Which condition may be a consequence of high doses of selegiline?
Which condition may be a consequence of high doses of selegiline?
What unique delivery method does rotigotine utilize in therapeutic applications?
What unique delivery method does rotigotine utilize in therapeutic applications?
Which neurotransmitter system does Safinamide primarily interact with besides monoamine oxidase-B inhibition?
Which neurotransmitter system does Safinamide primarily interact with besides monoamine oxidase-B inhibition?
Which neurological effect is commonly associated with dopamine agonists like pramipexole?
Which neurological effect is commonly associated with dopamine agonists like pramipexole?
What characteristic feature sets Rasagiline apart from other MAO-B inhibitors?
What characteristic feature sets Rasagiline apart from other MAO-B inhibitors?
Which side effect is least likely to occur with the administration of rotigotine?
Which side effect is least likely to occur with the administration of rotigotine?
What imaging study is most effective for demonstrating cortical hypometabolism in Alzheimer's disease?
What imaging study is most effective for demonstrating cortical hypometabolism in Alzheimer's disease?
Which of the following is a major sign observed in MRI scans of Alzheimer's disease patients?
Which of the following is a major sign observed in MRI scans of Alzheimer's disease patients?
Which class of drugs is specifically designed to increase acetylcholine levels in the brains of Alzheimer's patients?
Which class of drugs is specifically designed to increase acetylcholine levels in the brains of Alzheimer's patients?
What is the average life expectancy for individuals exhibiting symptoms of Alzheimer's disease?
What is the average life expectancy for individuals exhibiting symptoms of Alzheimer's disease?
In relation to Alzheimer's disease, what is a predominant cause of mortality associated with the progression of the condition?
In relation to Alzheimer's disease, what is a predominant cause of mortality associated with the progression of the condition?
Which of the following drugs is classified as a reversible cholinesterase inhibitor for treating Alzheimer's disease?
Which of the following drugs is classified as a reversible cholinesterase inhibitor for treating Alzheimer's disease?
What serious side effect resulted in the market withdrawal of tacrine for Alzheimer's treatment?
What serious side effect resulted in the market withdrawal of tacrine for Alzheimer's treatment?
Which pathological feature is recognized as an early indicator in the progression of Alzheimer's disease?
Which pathological feature is recognized as an early indicator in the progression of Alzheimer's disease?
What receptor does Memantine block in the treatment of Alzheimer's disease?
What receptor does Memantine block in the treatment of Alzheimer's disease?
In which stage of Alzheimer's disease is Memantine most indicated for treatment?
In which stage of Alzheimer's disease is Memantine most indicated for treatment?
Which atypical antipsychotic is specifically indicated for managing psychosis in Alzheimer's disease?
Which atypical antipsychotic is specifically indicated for managing psychosis in Alzheimer's disease?
What is a frequent side effect associated with NMDA receptor blockers like Memantine?
What is a frequent side effect associated with NMDA receptor blockers like Memantine?
When should Alzheimer's medications, including Memantine, be tapered off?
When should Alzheimer's medications, including Memantine, be tapered off?
What is the principal drug class utilized for cognitive enhancement in Alzheimer's disease treatment?
What is the principal drug class utilized for cognitive enhancement in Alzheimer's disease treatment?
What condition could warrant the cessation of Alzheimer's medication?
What condition could warrant the cessation of Alzheimer's medication?
In which stage of Alzheimer's disease is Memantine primarily added to the treatment regimen?
In which stage of Alzheimer's disease is Memantine primarily added to the treatment regimen?
Which class of medications is recommended to be avoided in Alzheimer's disease due to their negative impact on cognition?
Which class of medications is recommended to be avoided in Alzheimer's disease due to their negative impact on cognition?
After how many months of showing no desired effects should Alzheimer's medications generally be tapered off?
After how many months of showing no desired effects should Alzheimer's medications generally be tapered off?
Which receptor type is Memantine known to act upon in relation to Alzheimer's treatment?
Which receptor type is Memantine known to act upon in relation to Alzheimer's treatment?
What factor is essential for addressing insulin resistance in Alzheimer's patients?
What factor is essential for addressing insulin resistance in Alzheimer's patients?
What is the most appropriate initial course of action if an Alzheimer's patient has no improvement after starting treatment?
What is the most appropriate initial course of action if an Alzheimer's patient has no improvement after starting treatment?
Which type of toxicity is particularly managed within the multifactorial approach to promoting brain health in Alzheimer's patients?
Which type of toxicity is particularly managed within the multifactorial approach to promoting brain health in Alzheimer's patients?
Which method is most frequently utilized to evaluate cognitive decline in Alzheimer's patients?
Which method is most frequently utilized to evaluate cognitive decline in Alzheimer's patients?
What primary biomarkers are utilized for diagnosing Alzheimer's disease?
What primary biomarkers are utilized for diagnosing Alzheimer's disease?
Which type of toxicity is specifically targeted in the multi-factorial approach for managing Alzheimer's patients?
Which type of toxicity is specifically targeted in the multi-factorial approach for managing Alzheimer's patients?
What MoCA score range is indicative of normal cognitive function?
What MoCA score range is indicative of normal cognitive function?
A MoCA score of 19-25 suggests which level of cognitive decline?
A MoCA score of 19-25 suggests which level of cognitive decline?
What constitutes a statistically significant improvement on the MoCA scale for Alzheimer’s treatment?
What constitutes a statistically significant improvement on the MoCA scale for Alzheimer’s treatment?
What is the primary conclusion of the ReCODE program regarding Alzheimer's treatment effectiveness?
What is the primary conclusion of the ReCODE program regarding Alzheimer's treatment effectiveness?
What is the central focus of the ReCODE protocol in Alzheimer's disease management?
What is the central focus of the ReCODE protocol in Alzheimer's disease management?
What particular strategy is emphasized as part of optimizing brain health in Alzheimer's patients?
What particular strategy is emphasized as part of optimizing brain health in Alzheimer's patients?
Which stage of cognitive decline is most related to a MoCA score of 19-25?
Which stage of cognitive decline is most related to a MoCA score of 19-25?
What is the primary mechanism by which Alzheimer's disease drugs aim to treat symptoms?
What is the primary mechanism by which Alzheimer's disease drugs aim to treat symptoms?
Which of the following is associated with a higher incidence of Alzheimer's disease?
Which of the following is associated with a higher incidence of Alzheimer's disease?
What distinguishes tau protein in the context of Alzheimer's disease pathology?
What distinguishes tau protein in the context of Alzheimer's disease pathology?
Which specific gene variant is particularly linked to the genetic risk of developing Alzheimer's disease?
Which specific gene variant is particularly linked to the genetic risk of developing Alzheimer's disease?
What age range has the highest prevalence of Alzheimer's disease?
What age range has the highest prevalence of Alzheimer's disease?
What biological marker is crucial for diagnosing Alzheimer's disease?
What biological marker is crucial for diagnosing Alzheimer's disease?
Which factor is notably correlated with neuronal death in Alzheimer’s disease?
Which factor is notably correlated with neuronal death in Alzheimer’s disease?
Which neurotransmitter's activity is primarily reduced in Alzheimer's disease?
Which neurotransmitter's activity is primarily reduced in Alzheimer's disease?
Which imaging technique is specifically required to diagnose glucose uptake impairment in Alzheimer's patients?
Which imaging technique is specifically required to diagnose glucose uptake impairment in Alzheimer's patients?
Which class of drugs is typically effective for managing agitation in Alzheimer's disease?
Which class of drugs is typically effective for managing agitation in Alzheimer's disease?
What is considered a non-pharmacologic strategy for managing behavioral symptoms in Alzheimer's patients?
What is considered a non-pharmacologic strategy for managing behavioral symptoms in Alzheimer's patients?
Which antipsychotic medication is recommended for managing psychosis in Alzheimer's patients?
Which antipsychotic medication is recommended for managing psychosis in Alzheimer's patients?
What medication is frequently added during the moderate stages of Alzheimer's disease?
What medication is frequently added during the moderate stages of Alzheimer's disease?
Why should drugs with anticholinergic effects be avoided in Alzheimer's treatment?
Why should drugs with anticholinergic effects be avoided in Alzheimer's treatment?
Which class of medications should be avoided in Alzheimer's patients due to their sedative effects?
Which class of medications should be avoided in Alzheimer's patients due to their sedative effects?
Which factor is essential for managing insulin resistance in Alzheimer's disease?
Which factor is essential for managing insulin resistance in Alzheimer's disease?
What should be monitored to ensure better outcomes in Alzheimer's patients?
What should be monitored to ensure better outcomes in Alzheimer's patients?
What is the primary goal of the ReCODE program in Alzheimer's disease?
What is the primary goal of the ReCODE program in Alzheimer's disease?
Which cognitive assessment tool was utilized in the ReCODE program?
Which cognitive assessment tool was utilized in the ReCODE program?
After 12 months of intervention in the ReCODE program, what was a significant finding?
After 12 months of intervention in the ReCODE program, what was a significant finding?
What is the primary purpose of Caprylidene in the treatment of Alzheimer's?
What is the primary purpose of Caprylidene in the treatment of Alzheimer's?
In Alzheimer's patients, what alternative energy source does Caprylidene provide due to impaired glucose uptake?
In Alzheimer's patients, what alternative energy source does Caprylidene provide due to impaired glucose uptake?
Which diagnostic tool is applied to identify decreased glucose uptake in Alzheimer's patients before using Caprylidene?
Which diagnostic tool is applied to identify decreased glucose uptake in Alzheimer's patients before using Caprylidene?
Which behavioral symptom is commonly observed in advanced Alzheimer's disease?
Which behavioral symptom is commonly observed in advanced Alzheimer's disease?
What is the primary mechanism of action for reversible cholinesterase inhibitors in Alzheimer's disease?
What is the primary mechanism of action for reversible cholinesterase inhibitors in Alzheimer's disease?
Which imaging technique is most effective for visualizing metabolic activity in the brain related to Alzheimer's disease?
Which imaging technique is most effective for visualizing metabolic activity in the brain related to Alzheimer's disease?
What condition is commonly associated with complications leading to death in Alzheimer's patients?
What condition is commonly associated with complications leading to death in Alzheimer's patients?
What structural change is typically observed on MRI scans in patients with Alzheimer's disease?
What structural change is typically observed on MRI scans in patients with Alzheimer's disease?
Which of the following is considered a significant adverse effect of tacrine that led to its market removal?
Which of the following is considered a significant adverse effect of tacrine that led to its market removal?
What is the duration range of life expectancy commonly observed after the onset of Alzheimer's disease symptoms?
What is the duration range of life expectancy commonly observed after the onset of Alzheimer's disease symptoms?
Which cholinesterase inhibitor is known to be available in a transdermal patch formulation?
Which cholinesterase inhibitor is known to be available in a transdermal patch formulation?
What is the primary pathological hallmark that typically appears first in the progression of Alzheimer's disease?
What is the primary pathological hallmark that typically appears first in the progression of Alzheimer's disease?
Which atypical antipsychotic is most effective for managing psychosis in Alzheimer's disease?
Which atypical antipsychotic is most effective for managing psychosis in Alzheimer's disease?
What is the primary pharmacological class utilized for cognitive enhancement in Alzheimer's disease?
What is the primary pharmacological class utilized for cognitive enhancement in Alzheimer's disease?
At what stage of Alzheimer's disease is Memantine typically introduced in treatment?
At what stage of Alzheimer's disease is Memantine typically introduced in treatment?
Which class of medications is contraindicated in the treatment of Alzheimer's disease due to cognitive side effects?
Which class of medications is contraindicated in the treatment of Alzheimer's disease due to cognitive side effects?
What factor is essential for managing insulin resistance in Alzheimer's patients?
What factor is essential for managing insulin resistance in Alzheimer's patients?
Which method is widely used for assessing cognitive decline in patients with Alzheimer's?
Which method is widely used for assessing cognitive decline in patients with Alzheimer's?
Which strategy is least favorable for enhancing brain health in Alzheimer's patients?
Which strategy is least favorable for enhancing brain health in Alzheimer's patients?
What is identified as a form of toxicity addressed in the management of Alzheimer's disease?
What is identified as a form of toxicity addressed in the management of Alzheimer's disease?
What type of toxicity is specifically managed within the multi-factorial approach for Alzheimer's patients?
What type of toxicity is specifically managed within the multi-factorial approach for Alzheimer's patients?
A Montreal Cognitive Assessment (MoCA) score of 26-30 is indicative of what cognitive status?
A Montreal Cognitive Assessment (MoCA) score of 26-30 is indicative of what cognitive status?
Which score improvement on the MoCA scale is considered statistically significant for Alzheimer's treatment?
Which score improvement on the MoCA scale is considered statistically significant for Alzheimer's treatment?
What is the primary outcome of the ReCODE program in early Alzheimer's treatment?
What is the primary outcome of the ReCODE program in early Alzheimer's treatment?
Which treatment strategy is essential in the ReCODE protocol for addressing Alzheimer's?
Which treatment strategy is essential in the ReCODE protocol for addressing Alzheimer's?
A MoCA score between 19-25 typically suggests which cognitive condition?
A MoCA score between 19-25 typically suggests which cognitive condition?
What is a key focus in the cognitive assessment of Alzheimer's patients using MoCA?
What is a key focus in the cognitive assessment of Alzheimer's patients using MoCA?
What improvement must patients show on the MoCA scale to indicate a meaningful change in treatment effectiveness?
What improvement must patients show on the MoCA scale to indicate a meaningful change in treatment effectiveness?
What is the primary goal of treating ADHD for optimal patient functionality?
What is the primary goal of treating ADHD for optimal patient functionality?
Which medication is generally regarded as the first-line therapy for managing ADHD symptoms?
Which medication is generally regarded as the first-line therapy for managing ADHD symptoms?
Which subtype of ADHD encapsulates the presence of inattention, hyperactivity, and impulsivity in an individual?
Which subtype of ADHD encapsulates the presence of inattention, hyperactivity, and impulsivity in an individual?
In adult ADHD, which symptom is more prevalent compared to hyperactivity?
In adult ADHD, which symptom is more prevalent compared to hyperactivity?
Which nonpharmacologic treatment has been specifically approved for children diagnosed with ADHD?
Which nonpharmacologic treatment has been specifically approved for children diagnosed with ADHD?
What is a defining difference in ADHD symptoms observed between children and adults?
What is a defining difference in ADHD symptoms observed between children and adults?
For adults managing ADHD, which treatment modality provides benefits but is less effective than stimulants?
For adults managing ADHD, which treatment modality provides benefits but is less effective than stimulants?
Which subtype of ADHD is primarily associated with persistent difficulties in attention without the complication of hyperactivity?
Which subtype of ADHD is primarily associated with persistent difficulties in attention without the complication of hyperactivity?
What potential adverse effect is associated with the use of atomoxetine?
What potential adverse effect is associated with the use of atomoxetine?
What is the mechanism of action of stimulant medications used for ADHD?
What is the mechanism of action of stimulant medications used for ADHD?
What is the first-line recommendation for treating ADHD in children aged 6-18 years?
What is the first-line recommendation for treating ADHD in children aged 6-18 years?
What is the significant duration required as a washout period when changing from stimulants to MAOIs?
What is the significant duration required as a washout period when changing from stimulants to MAOIs?
Which age group is recommended to start ADHD treatment with behavioral therapy instead of medication?
Which age group is recommended to start ADHD treatment with behavioral therapy instead of medication?
Which class of drugs poses a risk of hypertensive crisis when used alongside stimulant medications?
Which class of drugs poses a risk of hypertensive crisis when used alongside stimulant medications?
What is the time frame during which atomoxetine reaches its full therapeutic effect?
What is the time frame during which atomoxetine reaches its full therapeutic effect?
What is the second-line treatment for ADHD when stimulant medications do not provide sufficient benefit?
What is the second-line treatment for ADHD when stimulant medications do not provide sufficient benefit?
Which medication is specifically known as a norepinephrine reuptake inhibitor used to treat ADHD?
Which medication is specifically known as a norepinephrine reuptake inhibitor used to treat ADHD?
What is one of the safety advantages of using atomoxetine over traditional stimulants for ADHD management?
What is one of the safety advantages of using atomoxetine over traditional stimulants for ADHD management?
In patients using atomoxetine, monitoring of which organ's function is advised?
In patients using atomoxetine, monitoring of which organ's function is advised?
Alpha-2 agonists like clonidine and guanfacine are primarily indicated for what specific ADHD symptoms?
Alpha-2 agonists like clonidine and guanfacine are primarily indicated for what specific ADHD symptoms?
What is a notable adverse effect linked to the use of alpha-2 agonists like clonidine?
What is a notable adverse effect linked to the use of alpha-2 agonists like clonidine?
Why are clonidine and guanfacine sometimes used alongside stimulant medications?
Why are clonidine and guanfacine sometimes used alongside stimulant medications?
Bupropion primarily influences which neurotransmitter systems relevant to ADHD?
Bupropion primarily influences which neurotransmitter systems relevant to ADHD?
What is a critical contraindication for prescribing bupropion?
What is a critical contraindication for prescribing bupropion?
What is the primary neurotransmitter target of viloxazine in its action as an ADHD medication?
What is the primary neurotransmitter target of viloxazine in its action as an ADHD medication?
Which age group is eligible for viloxazine therapy in the treatment of ADHD?
Which age group is eligible for viloxazine therapy in the treatment of ADHD?
What is a primary cardiovascular effect that can result from viloxazine use?
What is a primary cardiovascular effect that can result from viloxazine use?
Which of the following neurotransmitters is predominantly affected by stimulant medications such as amphetamines?
Which of the following neurotransmitters is predominantly affected by stimulant medications such as amphetamines?
What is the preferred approach for managing a case of stimulant overdose?
What is the preferred approach for managing a case of stimulant overdose?
Which symptom is least likely to be associated with stimulant overdose?
Which symptom is least likely to be associated with stimulant overdose?
What condition is commonly linked to the withdrawal from stimulant drugs?
What condition is commonly linked to the withdrawal from stimulant drugs?
What adverse effect is most commonly associated with the abuse of stimulant medications?
What adverse effect is most commonly associated with the abuse of stimulant medications?
What serious potential side effect of atomoxetine requires monitoring?
What serious potential side effect of atomoxetine requires monitoring?
Which adverse effect is reported to be more prevalent in children taking atomoxetine?
Which adverse effect is reported to be more prevalent in children taking atomoxetine?
What crucial parameter should be monitored regularly in patients treated with atomoxetine?
What crucial parameter should be monitored regularly in patients treated with atomoxetine?
In which situation is combination therapy particularly employed for ADHD management?
In which situation is combination therapy particularly employed for ADHD management?
Which two categories of medications are frequently used together in ADHD treatment regimens?
Which two categories of medications are frequently used together in ADHD treatment regimens?
What is the primary objective of implementing combination therapy in ADHD?
What is the primary objective of implementing combination therapy in ADHD?
How long does it generally take for atomoxetine to exhibit noticeable therapeutic effects?
How long does it generally take for atomoxetine to exhibit noticeable therapeutic effects?
Which of the following non-stimulant medications is specifically indicated for ADHD treatment?
Which of the following non-stimulant medications is specifically indicated for ADHD treatment?
Flashcards are hidden until you start studying
Study Notes
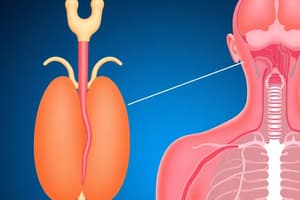
Overview of Pituitary and Hypothalamic Hormones
- Growth hormone (GH) is secreted by the anterior pituitary.
- Oxytocin is critical for inducing labor and controlling uterine bleeding.
- Vasopressin increases water reabsorption in the kidneys via V2 receptors.
Pituitary Hormones
- Adenohypophysis refers to the anterior pituitary.
- The posterior pituitary (neurohypophysis) secretes oxytocin.
- Growth hormone promotes tissue growth and regulates metabolism of proteins and carbohydrates.
Growth Hormone - Function and Deficiency
- Growth hormone deficiency in childhood can result in dwarfism.
- In adults, deficiency leads to muscle wasting and fatigue.
- Insulin-like growth factor-1 (IGF-1) mediates the effects of growth hormone.
Synthetic Growth Hormone - Somatotropin
- Somatotropin is used to treat pituitary dwarfism and growth failure in children.
- Serious side effect of somatotropin in children includes pseudotumor cerebri.
- In adults, somatotropin helps manage AIDS-related wasting syndrome.
Growth Hormone Inhibitors
- Somatostatin (Octreotide) inhibits the release of growth hormone.
- Octreotide is used in the treatment of acromegaly.
- Common side effects of somatostatin analogs include diarrhea and gallstones.
Growth Hormone Inhibitors - Pegvisomant
- Pegvisomant (Somavert) treats acromegaly.
- It acts as a growth hormone receptor antagonist.
- Administered via subcutaneous injection.
Dopamine Agonists - Bromocriptine
- Bromocriptine reduces secretion of growth hormone and prolactin.
- It binds to D2 receptors to achieve this effect.
- Primarily used for treating prolactinoma.
Oxytocin - Mechanism and Use
- Oxytocin primarily induces uterine contractions during pregnancy.
- After delivery, it helps control postpartum hemorrhage.
- Oxytocin is administered intravenously for labor induction.
Vasopressin - Mechanism of Action
- Vasopressin increases kidney water reabsorption through V2 receptors.
- Used to treat excessive water loss in central diabetes insipidus.
- Stimulating V1 receptors can help manage esophageal varices.
Vasopressin Analog - Desmopressin (DDAVP)
- Desmopressin acts on V2 receptors to reduce urine output in diabetes insipidus.
- Clinically, it treats central diabetes insipidus and nocturnal enuresis.
- Side effect of desmopressin therapy may include hyponatremia.
Vasopressin and Desmopressin - Clinical Applications
- Desmopressin is also effective in treating von Willebrand disease.
- Hyponatremia is a contraindication for desmopressin use.
- Desmopressin has greater selectivity for V2 receptors compared to vasopressin, minimizing vasoconstriction effects.
Intracellular T3 Production
- Impaired production of intracellular T3, while extracellular T3 levels remain unchanged.
- Reverse T3 (rT3) is the inactive form that C.Labs measures.
- T3 production in the body is not entirely halted.
Goals of Hypothyroidism Therapy
- Primary goal of levothyroxine therapy is to normalize TSH secretion.
- In patients with goiter, levothyroxine aims to reduce the size of the goiter.
- Recommended target TSH range for levothyroxine therapy is 0.5-2.5 µU/ml.
Hypothyroid Therapy in Special Populations
- Elderly patients with cardiovascular disease require a lower initial dose of levothyroxine to prevent overtreatment.
- Increased thyroid hormone demands during pregnancy necessitate more frequent monitoring of pregnant women with hypothyroidism.
- Common risk of inadequate treatment during pregnancy includes fetal developmental delays.
Levothyroxine Dosage and Dosing Considerations
- Recommended starting dose of levothyroxine for patients over 50 years old without cardiac disease is 50 mcg/day.
- More conservative levothyroxine dosing in older patients is critical to reduce risks of cardiac events.
- Propylthiouracil (PTU) inhibits conversion of T4 to T3 in peripheral tissues and is preferred in thyroid storm conditions.
Methimazole Overview
- Typical maintenance dose of methimazole for hyperthyroidism treatment is 5-15 mg daily.
- Methimazole is contraindicated during the first trimester of pregnancy due to the risk of fetal hypothyroidism and birth defects.
- It typically takes 2-3 weeks for T4 and T3 levels to drop post-initiation of methimazole therapy.
Thioamides - Mechanism of Action
- Methimazole inhibits thyroid hormone synthesis by blocking iodination of tyrosine.
- PTU is noted for its ability to inhibit both thyroid hormone synthesis and peripheral conversion of T4 to T3.
Methimazole (Tapazole®)
- Methimazole is typically favored over PTU in hyperthyroidism cases due to its potency and less frequent dosing requirement.
Alpha-Glucosidase Inhibitors - Clinical Pearls
- Alpha-glucosidase inhibitors should be taken with the first bite of a meal to optimize glucose control.
- They can reduce A1c levels by 0.7-0.8% in type 2 diabetes patients.
- Hypoglycemia management with these inhibitors necessitates the use of glucose tablets or gels rather than sucrose sources.
Alpha-Glucosidase Inhibitors - Monitoring
- Regular monitoring of liver function tests (LFTs) is essential for patients on alpha-glucosidase inhibitors.
- Assessment of post-meal blood glucose may be necessary to gauge postprandial glucose control.
- These inhibitors should be avoided for individuals with serum creatinine levels exceeding 2 mg/dL.
DPP-4 Inhibitors - Mechanism of Action
- DPP-4 inhibitors primarily stimulate insulin secretion while inhibiting glucagon secretion in type 2 diabetes patients.
- They increase levels of incretin hormones GIP and GLP-1, leading to improved glycemic control.
DPP-4 Inhibitors - Adverse Effects
- DPP-4 inhibitors are linked to potential promotion of cellular invasion in certain cancers.
SGLT2 Inhibitors - Mechanism of Action
- SGLT2 inhibitors block glucose reabsorption in the kidneys, increasing its excretion in urine.
- They provide significant benefits for patients with chronic kidney disease (CKD) and heart failure.
Overview of Oral Agents for Diabetes
- Metformin is the first-line therapy for Type 2 Diabetes Mellitus.
- Metformin enhances glucose uptake in muscle and fat, reducing insulin resistance.
- Insulin is the primary hormone responsible for lowering blood glucose levels.
Regulation of Blood Glucose
- Glucagon, secreted by pancreatic alpha cells, increases plasma glucose levels.
- Glucagon-like peptide 1 (GLP-1) increases insulin secretion.
- Dipeptidyl peptidase-4 (DPP-4) is the enzyme that breaks down GLP-1.
Hormone Action - Insulin
- Insulin activates GLUT-4 transporter for glucose uptake in muscle and adipose tissue.
- Glucose is converted to triglycerides for storage in adipose tissue under insulin influence.
- Insulin inhibits gluconeogenesis in the liver.
Hormone Action - Glucagon and Amylin
- Glucagon promotes glycogenolysis to increase blood glucose levels.
- Amylin, co-secreted with insulin, reduces appetite and delays gastric emptying.
- Amylin suppresses glucagon secretion to help control postprandial glucose levels.
Diabetes Mellitus - Overview
- Type 1 Diabetes Mellitus is characterized by autoimmune destruction of beta cells.
- Insulin resistance in Type 2 Diabetes Mellitus is primarily caused by a sedentary lifestyle and poor diet.
- Around 90% of diabetes cases are Type 2 Diabetes Mellitus.
Secondary and Gestational Diabetes
- Secondary diabetes can result from conditions like pancreatectomy.
- Gestational diabetes is most commonly diagnosed during the second or third trimester.
- Maturity-Onset Diabetes of the Young (MODY) is associated with secondary diabetes.
Screening for Diabetes
- A fasting plasma glucose (FPG) of ≥ 126 mg/dL is a criterion for diabetes diagnosis.
- An A1c of ≥ 6.0% also indicates diabetes.
Neurotrophic Hypothesis of Antidepressants
- Antidepressants increase Brain-Derived Neurotrophic Factor (BDNF) levels, promoting neurogenesis.
- Elevated cortisol levels are frequently observed in depression due to hormonal dysregulation.
Antidepressant Mechanisms
- Most antidepressants increase serotonin and norepinephrine concentrations in the synaptic cleft.
- Selective serotonin reuptake inhibitors (SSRIs) alleviate depression by blocking serotonin reuptake into presynaptic neurons.
- Antidepressants generally take weeks to show efficacy due to required BDNF synthesis time.
FDA Warning on Antidepressants
- Increased risk of suicidality (suicidal thoughts and behaviors) in patients under 25 using antidepressants.
- Antidepressant use during the first trimester of pregnancy is associated with low birth weight and premature delivery.
Monoamine Hypothesis
- Depression is proposed to be related to deficiencies in serotonin, norepinephrine, and dopamine.
- Evidence supporting this hypothesis includes the effect of reserpine, a monoamine-depleting drug that can induce depression.
- Glutamate levels are elevated in the cerebrospinal fluid of depressed patients.
Types and Mechanisms of Antidepressants
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) work by inhibiting the reuptake of serotonin and norepinephrine.
- Duloxetine (Cymbalta) is indicated for both depression and neuropathic pain.
- Venlafaxine is also used to treat social anxiety disorder in addition to depression.
SNRI Pharmacokinetics and Side Effects
- SNRIs are metabolized by the cytochrome P450 enzyme system.
- Dose reductions are necessary for patients with renal insufficiency.
- Hypertension is a common side effect of SNRIs, especially at higher doses.
Selection of Antidepressants
- When selecting an antidepressant, consider indication, cost, availability, adverse effects, drug interactions, and patient history.
- Selective serotonin reuptake inhibitors (SSRIs) are the most prescribed class for major depressive disorder (MDD) and anxiety disorders.
Clinical Indications for Antidepressants
- The goal of acute treatment is to achieve full remission of depressive symptoms.
- A trial of antidepressant therapy should last 8-12 weeks to evaluate efficacy.
- Long-term antidepressant therapy is recommended for patients with multiple serious MDD episodes in the past 5 years.
Antidepressant Discontinuation and Side Effects
- Tricyclic antidepressants (TCAs) carry the highest risk of fatal overdose.
- Dizziness and paresthesias are common symptoms of antidepressant discontinuation syndrome.
- Certain antidepressants are more likely to cause severe withdrawal symptoms if stopped abruptly.
Drug Interactions and Contraindications
- Paroxetine and fluoxetine are potent inhibitors of CYP2D6, leading to potential drug interactions.
- Citalopram and sertraline have fewer significant drug interactions.
- Using SSRIs with MAOIs poses a serious risk of serotonin syndrome.
Serotonin Syndrome
- Hallmark signs of serotonin syndrome include changes in consciousness, autonomic instability, and neuromuscular abnormalities.
Combination Insulin Products
- Typical composition of Humalog Mix 75/25: 75% insulin lispro protamine, 25% insulin lispro.
- Used to control both fasting and postprandial glucose levels.
Glargine/Lixisenatide Combination
- Combines long-acting insulin with a GLP-1 receptor agonist.
Inhaled Insulin (Afrezza)
- Primarily controls postprandial hyperglycemia.
- Major contraindication: COPD or asthma.
- Carries a boxed warning for acute bronchospasm in asthma or COPD sufferers.
Insulin Adverse Effects
- Most common adverse effect: hypoglycemia.
- Lipohypertrophy is a complication associated with excessive weight gain.
- Preventing insulin-induced hypoglycemia involves providing appropriate meal timing for insulin administration.
Regulation of Blood Glucose
- Alpha cells of the pancreas secrete glucagon.
- GLP-1 hormone attenuates plasma glucose spikes post-meal.
- DPP-4 enzyme is responsible for breaking down GLP-1.
Insulin - Indications and Production
- Indicated for Type 1, Type 2, secondary diabetes, and gestational diabetes.
- Modern insulin is produced using recombinant DNA technology.
- Recombinant insulin reduces the risk of antibody formation and allergic reactions compared to animal-based insulins.
Insulin Effects on the Body
- Affects skeletal muscle, adipose tissue, and the liver.
- Promotes glucose storage in the liver as glycogen.
- Increases triglyceride synthesis and VLDL formation.
Insulin Degradation and Metabolism
- GLUT4 transporter mediates glucose uptake in skeletal muscle and adipose tissue.
- Insulin increases protein synthesis in skeletal muscle and decreases protein catabolism in the body.
- Adipose tissue is responsible for storing triglycerides under the influence of insulin.
Continuous Glucose Monitoring (CGM)
- Purpose: provides real-time glucose levels and trends for diabetes management.
- Beneficial for patients using multiple daily insulin injections.
- Time in range (TIR) indicates the percentage of time glucose levels stay within target range.
Amylin Analog (Pramlintide)
- Analog of amylin, indicated for Type 1 and Type 2 diabetes patients already on insulin.
- Major side effect: severe hypoglycemia, leading to a boxed warning.
- Mechanism: slows gastric emptying and reduces postprandial glucose spikes. Administered via subcutaneous injection.
Carbidopa/Levodopa and Side Effects
- Long-term Carbidopa/Levodopa therapy commonly results in Dyskinesia as a side effect.
Dopamine Agonists
- A significant advantage of dopamine agonists over levodopa is their lower incidence of dyskinesia.
- Pramipexole is identified as a dopamine agonist used in treatment.
- Dopamine agonists are particularly effective in managing on-off phenomena in Parkinson's disease.
MAO-B Inhibitors
- MAO-B inhibitors function by inhibiting the breakdown of dopamine in the brain.
- A frequent side effect of MAO-B inhibitors is nausea.
- Rasagiline is noted for its neuroprotective properties among MAO-B inhibitors.
COMT Inhibitors
- Tolcapone is associated with hepatotoxicity.
- The primary role of COMT inhibitors is to reduce motor fluctuations in patients with Parkinson's disease.
- A harmless and typical side effect of COMT inhibitors is red-brown discoloration of urine.
Combination Therapies
- COMT inhibitors are most often used in conjunction with Levodopa/Carbidopa.
Adenosine A2A Antagonists
- Istradefylline acts as an adenosine A2A receptor antagonist for Parkinson's disease treatment.
- A common side effect of adenosine A2A receptor antagonists is dyskinesias.
- The mechanism of action involves blocking adenosine receptors, leading to improved motor function.
Amantadine
- Amantadine serves as adjunctive therapy specifically for managing dyskinesias in Parkinson's disease.
- A unique side effect linked to amantadine is livedo reticularis.
- Originally, amantadine was used to treat influenza.
Antimuscarinics
- Antimuscarinics mainly target the symptom of tremors in Parkinson's disease.
- A common side effect of antimuscarinic drugs is memory impairment.
- The role of acetylcholine in Parkinson's disease is that it becomes overactive when dopamine levels decrease.
Basal Motor Pathway
- In the basal ganglia, dopamine primarily inhibits cholinergic neurons.
- In Parkinsonism, the inhibitory pathway of the basal ganglia becomes overactive due to a deficiency of dopamine.
- An imbalance between dopamine and acetylcholine leads to the symptom of tremors.
Parkinsonism Pathophysiology
- Critical neurotransmitter imbalance in Parkinson's disease involves dopamine and acetylcholine.
- GABA becomes overactive due to excess acetylcholine, contributing to motor dysfunction.
- Dopamine deficiency increases inhibitory control of muscles, exacerbating motor symptoms.
Treatment Goals in Parkinsonism
- The primary treatment objective in Parkinsonism is to increase dopaminergic neurotransmission.
- A D2 and D3 receptor agonist is crucial in dopaminergic therapy for Parkinson's disease.
Essential Tremor
- Essential tremor is characterized by fine motor movement during intentional actions.
- Beta-blockers serve as the first-line treatment for managing essential tremor.
- Factors such as caffeine can exacerbate essential tremor symptoms.
Additional Treatments for Essential Tremor
- If beta-blockers are ineffective, Topiramate can be utilized for essential tremor.
- Primidone is associated with sedation as a side effect when treating essential tremor.
- Postural tremor is the type commonly treated with beta-blockers like propranolol.
Overview of Alzheimer’s Disease and Treatment
- Main focus of pharmaceutical treatment: Prevent breakdown of acetylcholine (ACh) in the synapse.
- Risk factors for Alzheimer's: Notable link to African American ethnicity.
- Pathological hallmark: Amyloid plaque deposition is a key feature of Alzheimer's disease.
Alzheimer's Disease Risk Factors
- Genetic risk: ApoE4 gene significantly increases the likelihood of developing Alzheimer's.
- Gender susceptibility: Females are more at risk compared to males.
- Age factor: Individuals aged 65 and older are predominantly affected by Alzheimer's disease.
Pathogenesis of Alzheimer's Disease
- Neurofibrillary tangles are formed by Tau protein.
- Neuronal death often caused by excitotoxicity and oxidative stress.
- Acetylcholine levels are decreased, impacting cognitive function.
Diagnosis of Alzheimer's Disease
- Key biomarkers: Amyloid-beta and tau levels in cerebrospinal fluid assist in diagnosis.
- Imaging studies: PET scans reveal cortical hypometabolism; MRIs often show hippocampal atrophy.
Treatment Strategies for Alzheimer's Disease
- Drug class used: Reversible cholinesterase inhibitors, such as Donepezil, enhance ACh levels.
- Life expectancy post-symptom onset: Typically 6 to 12 years.
- Common cause of death: Complications arising from immobility.
Reversible Cholinesterase Inhibitors
- Donepezil is a primary reversible cholinesterase inhibitor.
- Rivastigmine is notable for its patch formulation.
- Tacrine was removed from the market due to hepatotoxicity concerns.
Alzheimer's Disease Pathogenesis Revisited
- Amyloid plaques appear earlier in the disease progression than neurofibrillary tangles.
- Neurofibrillary tangles are related to microtubules.
- Memantine, used in treatment, is an NMDA receptor antagonist effective in moderate to severe stages, with dizziness as a common side effect.
Clinical Tips for Treatment
- Taper off medications during end-of-life care or significant side effects.
- Severe side effects or an MMSE score below 10 signal the need to discontinue medications.
- Medications should be tapered off after no improvement is observed for 3 to 6 months.
NMDA Blockers
- Memantine functions as an NMDA receptor antagonist.
- Safety profile includes dizziness as the most reported side effect.
- Typically indicated for moderate to severe Alzheimer's stages.
Cognitive Assessment and Evaluation
- Most common assessment tool: MMSE (Mini-Mental State Examination).
- MoCA scores: A score of 26-30 is considered normal; 19-25 suggests mild cognitive impairment (MCI).
- Statistically significant improvement is defined as an increase of more than 3 points on the MoCA scale.
Conclusion of ReCODE Program
- ReCODE program aims for a personalized and multi-factorial approach to Alzheimer's treatment.
- It can stabilize or improve cognitive function in the early stages but is not a cure for the disease.
- Emphasizes comprehensive strategies beyond medication, including lifestyle decisions and toxicity management.
Alzheimer's Disease Imaging and Diagnosis
- PET scans are effective in showing cortical hypometabolism in Alzheimer's disease.
- MRI reveals hallmark findings like hippocampal atrophy, an early indicator of Alzheimer’s.
- Key diagnostic tools include MRI and PET scans to assess glucose uptake impairment and amyloid plaques.
Alzheimer's Disease Pathogenesis
- Amyloid plaques appear earlier than neurofibrillary tangles and are crucial in diagnosis.
- Neurofibrillary tangles are associated with microtubules, disrupting neuronal function.
- Diagnosis often requires MRI for imaging glucose uptake impairment.
Alzheimer's Disease Treatment
- Reversible cholinesterase inhibitors, such as Donepezil, augment acetylcholine in the brain.
- Memantine is typically used in the moderate to severe stages of the disease.
- Complications of immobility are common causes of death in Alzheimer’s patients.
Behavioral Symptoms and Management
- SSRIs, specifically Citalopram, are commonly prescribed for agitation in Alzheimer’s.
- Cognitive-behavioral therapy serves as a typical non-pharmacologic approach for managing behavioral symptoms.
- Risperidone is recommended for managing psychosis in Alzheimer’s patients.
Cognitive Assessments
- The Montreal Cognitive Assessment (MoCA) is favored for cognitive evaluation, with scores of 26-30 considered normal.
- A score of 19-25 indicates mild cognitive impairment (MCI).
- Statistically significant improvement in treatment is marked by increases of more than 3 points on the MoCA scale.
Current Treatment Strategies
- Certain medications, especially those with anticholinergic properties, should be avoided due to potential cognitive decline.
- Physical exercise is crucial for managing factors like insulin resistance in Alzheimer's patients.
- Multi-factorial approaches address issues like heavy metal toxicity, focusing on optimizing brain health.
ReCODE Program Insights
- The ReCODE program aims to improve cognitive and metabolic functions in Alzheimer’s patients.
- Cognitive stabilization or improvement was noted in participants after 12 months.
- The program emphasizes a personalized, multi-factorial treatment approach rather than solely pharmaceutical interventions.
Caprylidene's Role
- Caprylidene provides ketone bodies as an alternative energy source in Alzheimer's treatment, particularly when glucose uptake is impaired.
- It is identified as a therapeutic option when MRI shows decreased glucose uptake.
Conclusion
- The comprehensive approach to Alzheimer’s treatment includes cognitive enhancement via cholinesterase inhibitors and personalized strategies to tackle various cognitive and metabolic needs.
- Heavy metal toxicity management is an essential component of optimizing brain health for Alzheimer's patients.
Treatment Goals for ADHD
- Primary goal: Reduce symptoms to enable functioning in all environments.
- Stimulants are the first-line therapy for ADHD.
- ADHD combined type includes symptoms of inattention, hyperactivity, and impulsivity.
Types and Symptoms of ADHD
- Common adult symptom: Inattention.
- ADHD predominantly inattentive type characterized by difficulty focusing without hyperactivity.
- Hyperactivity is more prevalent in childhood, while inattention is more dominant in adulthood.
Nonpharmacologic Treatments
- EndeavorRx is an approved game-based device for treating ADHD in children.
- Cognitive Behavioral Therapy (CBT) beneficial for adults but less effective than stimulants.
- Key component of treatment includes patient and family education.
Stimulant Therapy
- Stimulant medications are recommended first-line treatments for children aged 6-18.
- Atomoxetine serves as a second-line treatment if stimulants are ineffective.
- Behavioral therapy should be the first approach for children aged 4-5.
Drug Interactions in Stimulant Therapy
- Monoamine oxidase inhibitors (MAOIs) should not be used with stimulants due to hypertensive crisis risk.
- Combining methylphenidate with clonidine can lead to increased cardiovascular effects.
- A 14-day washout period is required when switching between stimulants and MAOIs.
Atomoxetine Overview
- Atomoxetine (Strattera) works by inhibiting norepinephrine reuptake.
- Possible adverse effect includes hepatotoxicity.
- It may take up to 4 weeks for atomoxetine to demonstrate full efficacy.
Non-Stimulants
- Atomoxetine is the only non-stimulant approved for ADHD treatment.
- Common adverse effects of atomoxetine include hepatotoxicity and gastrointestinal upset.
- Liver function should be regularly monitored in patients prescribed atomoxetine.
Alpha-2 Agonists
- Clonidine and guanfacine target hyperactivity and impulsivity in ADHD.
- Sedation is a common side effect associated with alpha-2 agonists.
- Used in combination with stimulants to reduce hyperactivity and provide sedation.
Bupropion and Viloxazine
- Bupropion primarily affects dopamine and norepinephrine; contraindicated in seizure disorders.
- Viloxazine (Qelbree) is approved for ages 6 and older, inhibits norepinephrine reuptake with potential side effects including increased blood pressure and heart rate.
Stimulant Abuse and Dependence
- Common adverse effect of stimulant abuse: tremors and cardiac arrhythmias.
- Signs of withdrawal may include mental depression and lethargy.
- Stimulants predominantly affect dopamine and norepinephrine systems.
Stimulant Overdose Management
- Recommended treatment includes supportive care and controlling seizures in overdose situations.
- Hypertensive crisis is the most common cardiovascular complication.
- Bradycardia is not a symptom of stimulant overdose.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.