Podcast
Questions and Answers
What is the relationship between KE and PE in the context of blood flow?
What is the relationship between KE and PE in the context of blood flow?
- KE increases when PE decreases (correct)
- KE decreases when PE increases
- KE is independent of PE
- KE is directly proportional to PE
What is the total peripheral resistance (TPR) in the body?
What is the total peripheral resistance (TPR) in the body?
- The site where blood pressure is measured
- The collective designation for arterioles that vasoconstrict and vasodilate (correct)
- The combination of all arterioles and arteries
- The combination of all veins and venules
What happens to total pressure (TE) along the streamline according to Bernoulli?
What happens to total pressure (TE) along the streamline according to Bernoulli?
- It increases in one segment and decreases in another
- It remains constant throughout the entire streamline (correct)
- It is affected by viscosity and turbulence
- It decreases in one segment and remains the same in another
What is the effect of vasoconstriction on blood flow and pressure?
What is the effect of vasoconstriction on blood flow and pressure?
What is the driving force for blood flow between two points?
What is the driving force for blood flow between two points?
What happens to pressure (PE) in the arteriole in the given diagram?
What happens to pressure (PE) in the arteriole in the given diagram?
What is the flow (Q) in the arteriole affected by?
What is the flow (Q) in the arteriole affected by?
What is the relationship between resistance (R) and vasoconstriction?
What is the relationship between resistance (R) and vasoconstriction?
What is not accounted for in Bernoulli's principle?
What is not accounted for in Bernoulli's principle?
What is the upstream artery used for?
What is the upstream artery used for?
What is the primary function of the reservoir of mercury in the blood pressure measurement device?
What is the primary function of the reservoir of mercury in the blood pressure measurement device?
What happens to blood flow through the brachial artery when the air is blown into the cuff?
What happens to blood flow through the brachial artery when the air is blown into the cuff?
What is the primary factor that determines systolic pressure?
What is the primary factor that determines systolic pressure?
What is the function of the stethoscope in the blood pressure measurement process?
What is the function of the stethoscope in the blood pressure measurement process?
What is the effect of elastic recoil of the aorta on blood pressure?
What is the effect of elastic recoil of the aorta on blood pressure?
What is the purpose of slowly letting the air out of the cuff during blood pressure measurement?
What is the purpose of slowly letting the air out of the cuff during blood pressure measurement?
What is the relationship between blood pressure and the size and flexibility of the arteries?
What is the relationship between blood pressure and the size and flexibility of the arteries?
What is the effect of activity on blood pressure?
What is the effect of activity on blood pressure?
What is the primary factor that determines diastolic pressure?
What is the primary factor that determines diastolic pressure?
Why is it important to wrap the cuff around the upper arm during blood pressure measurement?
Why is it important to wrap the cuff around the upper arm during blood pressure measurement?
Alpha 1 receptors increase heart rate and contractility.
Alpha 1 receptors increase heart rate and contractility.
Angiotensin II decreases blood pressure.
Angiotensin II decreases blood pressure.
Nitric oxide causes vasoconstriction.
Nitric oxide causes vasoconstriction.
The sympathetic nervous system increases heart rate and contractility through beta 2 receptors.
The sympathetic nervous system increases heart rate and contractility through beta 2 receptors.
Atrial natriuretic peptide increases blood volume.
Atrial natriuretic peptide increases blood volume.
Flashcards are hidden until you start studying
Study Notes
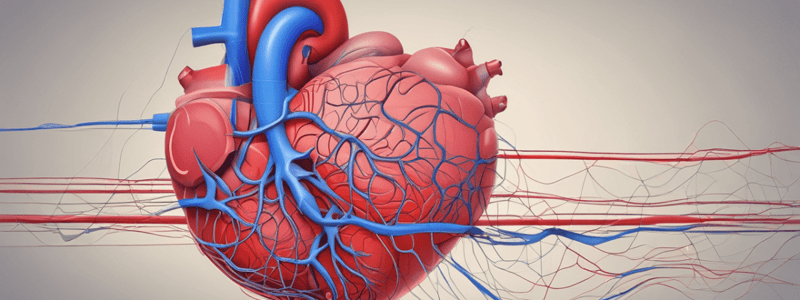
The Cardiovascular System
- The ECG (Electrocardiogram) measures the electrical activity of the heart.
ECG Components
- P wave: Atrial activation
- PR Interval: Onset of atrial activation to onset of ventricular activation
- QRS Complex: Ventricular activation
- QRS Duration: Duration of ventricular activation
- ST-T Wave: Ventricular re-polarization
- QT Interval: Duration of ventricular activation and recovery
- U Wave: After-depolarizations in the ventricles
Electrical and Mechanical Events
- Atrial depolarization (electrical) → Atrial contraction (mechanical)
- Ventricular depolarization (electrical) → Ventricular contraction (mechanical)
- Ventricular re-polarization (electrical) → Ventricular relaxation (mechanical)
ECG Leads
- Standard leads: I, II, and III (bipolar, detect electrical potential change in frontal plane)
- Augmented limb leads: aVR, aVL, and aVF (unipolar, detect electrical potential change in frontal plane)
Cardiac Myocyte Cycle
- Phase 0: Rapid influx of Na+ ions through "fast" channels
- Phase 1: Closing of Na+ voltage-gated channels (VGCs)
- Phase 2: Influx of Ca++ and slow efflux of K+
- Phase 3: Rapid repolarization (closing of Ca++ VGCs, efflux of K+)
- Phase 4: Unstable resting phase (influx of Na+, Ca++, and slow efflux of K+)
Cardiac Output and Other Dynamics
- Cardiac output (CO) = Heart rate (HR) x Stroke volume (SV)
- Cardiac index (CI) = CO/m²
- Starling's Law: Contractile force increases as the heart muscle stretches, but only to a point
- Preload: Stretch on the heart muscle before contraction
- Afterload: Resistance to blood flow after contraction
Intrinsic and Extrinsic Factors
- Intrinsic factors: Conduction system, functional syncytium, auto-regulation
- Extrinsic factors: Parasympathetic and sympathetic nervous systems, vascular variables
Cardiovascular Control Systems
- Key variables: Blood pressure (BP), cardiac output (CO), heart rate (HR), stroke volume (SV)
- Key equations: CO = HR x SV, CI = CO/m²
- Bernoulli's equation: Does not account for factors such as viscosity, turbulence, or gravity
Vasoconstriction, Blood Flow, and Blood Pressure
- Total peripheral resistance (TPR) beds: Arterioles that vasoconstrict and vasodilate
- Poiseuille and Bernoulli: Flow (Q), pressure (PE), and resistance (R) are related reciprocally
- Vasoconstriction increases resistance (R), decreases flow (Q), and increases pressure (PE)
Electrocardiography
- aVF (left leg) records a change in electric potential in the frontal plane
- Lead I is between the right arm and left arm electrodes, with the left arm being positive
- Lead II is between the right arm and left leg electrodes, with the left leg being positive
- Lead III is between the left arm and left leg electrodes, with the left leg being positive
- Einthoven's Triangle is a diagrammatic representation of these three leads
ECG Precordial Leads
- These six unipolar leads are located on the chest and record electric potential changes in the heart in a cross-sectional plane
- Each lead records electrical variations that occur directly under the electrode
The Cardiac Myocyte Action Potential
- Phase 0: rapid influx of Na+ via open Na+ VGCs and influx of Ca++ via Ca++ VGCs
- Phase 1: closing of Na+ VGCs and small influx of Cl-, small efflux of K+
- Phase 2: influx of Ca++ and efflux of K+ via open K+ VGCs
- Phase 3: closing of Ca++ VGCs and efflux of K+ via open K+ VGCs
- Phase 4: diastole, resting phase
Cardiac Output and Other Dynamics
- Cardiac Output (CO) = Heart Rate (HR) x Stroke Volume (SV)
- CO can be modified by both intrinsic and extrinsic variables
- Cardiac Index (CI) = CO/m2 (body surface area)
Blood Flow and Resistance
- Poiseuille's Equation: Q = ΔP/R, where Q is flow, ΔP is pressure difference, and R is resistance
- Three primary factors that determine resistance: vessel diameter (or radius), vessel length, and viscosity of the blood
- Vessel diameter is the most important factor quantitatively and physiologically
Bernoulli's Principle
- Kinetic energy and pressure energy can be interconverted, so total energy remains unchanged
- Total pressure is constant along a streamline
- Low pressure in one segment increases pressure in another connected segment
- KE (kinetic energy) and PE (pressure energy) are related reciprocally: if one increases, the other must decrease
Vasoconstriction, Blood Flow, and Blood Pressure
- Total Peripheral Resistance (TPR) beds are arterioles of the body
- Vasoconstriction increases resistance, decreases flow, and increases pressure
- Vasodilation decreases resistance, increases flow, and decreases pressure
Evaluating Blood Pressure
- Blood pressure is measured using a cuff and mercury column
- Systolic Pressure is measured when blood flow first returns (first heard pulse)
- Diastolic Pressure is measured when the pulse sound disappears (elastic recoil of the Aorta)
- Blood pressure is influenced by activity, temperature, diet, emotional state, posture, physical state, and medication use
The Cardiovascular System Physiology
ECG
- The cardiovascular system consists of the aorta, systemic circulation, pulmonary circulation, and heart
- The heart undergoes isovolumetric contraction, isovolumetric relaxation, ventricular ejection, and rapid inflow phases
Phases of the Nodal Action Potential
- Phase 4: unstable rest or pacemaker potential, caused by an influx of sodium (Na+) and calcium (Ca++) ions
- Phase 0: rapid depolarization, caused by a large influx of Ca++ ions
- Phase 3: repolarization, caused by a slow efflux of potassium (K+) ions
Phases of the Cardiac Myocyte Action Potential
- Phase 0: rapid depolarization, caused by an influx of Na+ ions
- Phase 1: caused by the closure of "fast" Na+ channels and a small influx of chloride (Cl-) ions
- Phase 2: plateau phase, caused by an influx of Ca++ and an efflux of K+ ions
- Phase 3: repolarization, caused by a slow efflux of K+ ions
Cardiac Output and Other Dynamics
- Cardiac output (CO) = heart rate (HR) x stroke volume (SV)
- CO can be modified by intrinsic and extrinsic factors
- Starling's Law: contractile force increases as the heart muscle stretches, but only up to a point
- Poiseuille's Equation: Q = ∆P/R, where Q is flow, ∆P is pressure difference, and R is resistance
Autonomic Receptors
- Alpha 1: vasoconstriction (VC) in total peripheral resistance (TPR) beds
- Alpha 2: inhibits norepinephrine (NE) release
- Beta 1: increases heart rate and contractility
- Beta 2: vasodilation (VD) in TPR beds
Key Biochemical Players in Cardiovascular Control
- Acetylcholine (ACH): decreases heart rate
- Aldosterone (ALD): increases sodium absorption and blood volume, leading to increased blood pressure
- Angiotensin II (AGII): increases vasoconstriction and blood pressure
- Atrial natriuretic peptide (ANP): increases sodium loss and decreases blood volume, leading to decreased blood pressure
- Anti-diuretic hormone (ADH/AVP): increases water absorption and vasoconstriction
- Epinephrine (EP): increases vasoconstriction, heart rate, and contractility
- Nitric oxide (NO): vasodilation and increased tissue perfusion
- Renin: increases conversion of angiotensinogen to AGII
Cardiovascular Control Systems
- Intrinsic factors that influence heart operation: SA node, contractility, and intercalated disks
- Extrinsic factors that influence heart operation: parasympathetic nervous system (PNS), sympathetic nervous system (SNS), preload, and afterload
- Intrinsic factors that influence vascular operation: endothelial cells, metabolic by-products, myogenic auto-regulation, and elasticity of great arteries
- Extrinsic factors that influence vascular operation: neural and hormonal factors
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.