Podcast
Questions and Answers
What is the primary function of the parathyroid glands?
What is the primary function of the parathyroid glands?
- Regulating pituitary hormone secretion
- Enhancing neuromuscular excitability
- Producing vitamin D
- Exclusive control of calcium metabolism (correct)
How does the parathyroid gland regulate calcium levels?
How does the parathyroid gland regulate calcium levels?
- By releasing hormones that inhibit calcium absorption
- By directly sensing calcium levels in the blood (correct)
- By stimulating the release of vitamin D
- By responding to pituitary hormone signals
What is the effect of unregulated calcium on the muscular system?
What is the effect of unregulated calcium on the muscular system?
- Muscle cramps and weakness (correct)
- Increased muscle strength and contraction
- Enhanced neuromuscular excitability
- Reduced bone resorption
What is the primary cause of secondary hyperparathyroidism?
What is the primary cause of secondary hyperparathyroidism?
What is the effect of hyperparathyroidism on bone health?
What is the effect of hyperparathyroidism on bone health?
What is the primary symptom of hyperparathyroidism related to the nervous system?
What is the primary symptom of hyperparathyroidism related to the nervous system?
What is the role of the bones in calcium metabolism?
What is the role of the bones in calcium metabolism?
What is the effect of parathyroid hormone on calcium levels?
What is the effect of parathyroid hormone on calcium levels?
What is the effect of PTH on calcium reabsorption in the renal system?
What is the effect of PTH on calcium reabsorption in the renal system?
What is the cause of secondary hyperparathyroidism?
What is the cause of secondary hyperparathyroidism?
What is the effect of PTH on vitamin D production in the kidneys?
What is the effect of PTH on vitamin D production in the kidneys?
What is the treatment for severe hypercalcemia due to primary hyperparathyroidism?
What is the treatment for severe hypercalcemia due to primary hyperparathyroidism?
What is the effect of low PTH levels on bone resorption?
What is the effect of low PTH levels on bone resorption?
What is the complication of hypoparathyroidism?
What is the complication of hypoparathyroidism?
What is the effect of PTH on phosphate excretion in the renal system?
What is the effect of PTH on phosphate excretion in the renal system?
What is the effect of PTH on calcium levels in the extracellular fluid?
What is the effect of PTH on calcium levels in the extracellular fluid?
Study Notes
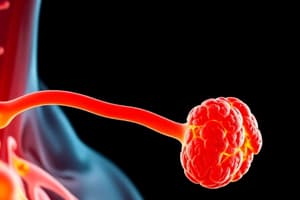
Parathyroid Glands
- 4 tiny glands with rich blood supply, interact with blood calcium
- Exclusive for calcium metabolism
- Produce hormones PTH
- Measurement of PTH in blood indicates its function
- Control calcium in blood and bones
Calcium Function
- Provides electrical energy for the nervous system
- Conducts electricity in the nervous system
- Stabilizes neuromuscular excitability, making nerves less sensitive to stimuli
- Provides energy for cells to contract in the muscular system
- Strengthens skeletal system by making bones strong
- Bones serve as calcium storage system
Hyperparathyroidism
- Excess PTH secretion
- Causes increased bone resorption/osteoporosis, hypercalcemia, and hypercalciuria
- Types: Primary and Secondary
- Primary: Tumor of parathyroid gland, failure, or chronic renal failure
- Secondary: Compensatory response to hypocalcemia often due to chronic renal failure
Primary Hyperparathyroidism
- Caused by parathyroid adenoma (one or more glands)
- Leads to increased skeletal resorption, release of Ca2+ and Pi from bone
- Increases Ca2+ and Pi absorption from small intestine
- Enhances Ca2+ reabsorption and inhibits Pi reabsorption from renal, causing increased urine Pi excretion
- Results in increased ECF calcium and decreased ECF phosphate
Secondary Hyperparathyroidism
- Caused by chronic renal failure and malabsorption
- Elevated PTH levels
- Long-term activation causes hyperplasia of glands, loss of sensitivity to circulating calcium
- Autonomous secretion of PTH even with normal calcium levels
Complications of Hyperparathyroidism
- Death due to cardiac and neurological dysfunctions
- Hypercalcemia, hypercalciuria, and osteoporosis
Treatment of Hyperparathyroidism
- Medical emergency for severe hypercalcemia
- Use diuretics to increase calcium excretion
- Use drugs to inhibit bone resorption
- Surgical removal of tumor or ectopic secretion due to tumor
Hypoparathyroidism
- Abnormal or low PTH levels
- Etiology: thyroid surgery, autoimmunity, genetic mechanism, and Di George syndrome
- Clinical findings: depressed calcium, increased phosphate, decreased bone resorption, and hypocalciuria
- Treatment: calcium and vitamin D replacement therapy, risk of kidney stones
Complications of Hypoparathyroidism
- Paresthesia, muscle cramps, and spasms (tetany)
- Fatigue, headaches, bone pain, and insomnia
- Severe irregularities in normal heart beat
- Spasm of airways causing respiratory failure
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the functions of parathyroid glands, calcium metabolism, and calcium's role in the nervous system and muscle contractions.