Podcast
Questions and Answers
What is the volume that remains in the lungs after a maximal expiration?
What is the volume that remains in the lungs after a maximal expiration?
- Expiratory reserve volume
- Inspiratory reserve volume
- Tidal volume
- Residual volume (correct)
What is the functional measurement that is defined as the volume of the lungs that does not participate in gas exchange?
What is the functional measurement that is defined as the volume of the lungs that does not participate in gas exchange?
- Expiratory reserve volume
- Physiologic dead space (correct)
- Anatomic dead space
- Inspiratory reserve volume
What is the volume that can be inspired over and above the tidal volume?
What is the volume that can be inspired over and above the tidal volume?
- Expiratory reserve volume
- Inspiratory reserve volume (correct)
- Tidal volume
- Residual volume
What is the volume of the conducting airways?
What is the volume of the conducting airways?
What is the equation used to calculate physiologic dead space?
What is the equation used to calculate physiologic dead space?
What is the normal approximate value of anatomic dead space?
What is the normal approximate value of anatomic dead space?
What is the volume that can be expired after the expiration of a tidal volume?
What is the volume that can be expired after the expiration of a tidal volume?
What is the term for the difference between the volume of air that can be inspired and the tidal volume?
What is the term for the difference between the volume of air that can be inspired and the tidal volume?
What happens to the abdominal contents when the diaphragm contracts?
What happens to the abdominal contents when the diaphragm contracts?
During normal quiet breathing, which muscles are NOT used for inspiration?
During normal quiet breathing, which muscles are NOT used for inspiration?
What is the process of expiration normally?
What is the process of expiration normally?
What is the role of abdominal muscles during forced expiration?
What is the role of abdominal muscles during forced expiration?
What is the equation for compliance of the respiratory system?
What is the equation for compliance of the respiratory system?
What is the relationship between compliance and elastance?
What is the relationship between compliance and elastance?
What is the units of compliance in the respiratory system?
What is the units of compliance in the respiratory system?
What is the slope of the pressure-volume curve?
What is the slope of the pressure-volume curve?
What is the sum of all four lung volumes?
What is the sum of all four lung volumes?
What is the ratio of FEV1 to FVC in normal subjects?
What is the ratio of FEV1 to FVC in normal subjects?
What is the most important muscle for inspiration?
What is the most important muscle for inspiration?
In restrictive lung disease, such as fibrosis, what is the effect on FEV1 and FVC?
In restrictive lung disease, such as fibrosis, what is the effect on FEV1 and FVC?
What is the volume of air that can be forcibly expired after a maximal inspiration?
What is the volume of air that can be forcibly expired after a maximal inspiration?
What is the effect on FEV1/FVC in obstructive lung disease, such as asthma and COPD?
What is the effect on FEV1/FVC in obstructive lung disease, such as asthma and COPD?
What is the unit of measurement for time in the figure illustrates FVC and FEV1?
What is the unit of measurement for time in the figure illustrates FVC and FEV1?
In which type of lung disease is FEV1 reduced more than FVC?
In which type of lung disease is FEV1 reduced more than FVC?
What is the difference in pressure that determines lung volume?
What is the difference in pressure that determines lung volume?
What occurs when the pressure outside of the lungs is negative?
What occurs when the pressure outside of the lungs is negative?
What is the term for the difference between the inflation and deflation curves of the lung?
What is the term for the difference between the inflation and deflation curves of the lung?
At what range of pressures is lung compliance greatest?
At what range of pressures is lung compliance greatest?
What is the result of high expanding pressures on lung compliance?
What is the result of high expanding pressures on lung compliance?
What is the relationship between the compliance of the lungs and chest wall separately and together?
What is the relationship between the compliance of the lungs and chest wall separately and together?
What is the shape of the pressure-volume curve at high expanding pressures?
What is the shape of the pressure-volume curve at high expanding pressures?
Why does the lung follow a different curve during inspiration and expiration?
Why does the lung follow a different curve during inspiration and expiration?
What happens to the intrapleural pressure when air is introduced into the intrapleural space?
What happens to the intrapleural pressure when air is introduced into the intrapleural space?
What is the result of increased lung compliance in a patient with emphysema?
What is the result of increased lung compliance in a patient with emphysema?
What is the tendency of the lungs in a patient with fibrosis?
What is the tendency of the lungs in a patient with fibrosis?
What is the relationship between the collapsing force on the lungs and the expanding force on the chest wall at FRC?
What is the relationship between the collapsing force on the lungs and the expanding force on the chest wall at FRC?
What is the effect of decreased lung compliance in a patient with fibrosis?
What is the effect of decreased lung compliance in a patient with fibrosis?
What happens to the chest wall in a patient with emphysema?
What happens to the chest wall in a patient with emphysema?
What is the result of the opposing forces at FRC?
What is the result of the opposing forces at FRC?
What is the relationship between elastic recoil and lung compliance?
What is the relationship between elastic recoil and lung compliance?
What is the relationship between surface tension and collapsing pressure in an alveolus?
What is the relationship between surface tension and collapsing pressure in an alveolus?
What is the effect of surfactant on the collapsing pressure of small alveoli?
What is the effect of surfactant on the collapsing pressure of small alveoli?
What is the difference in collapsing pressure between large and small alveoli?
What is the difference in collapsing pressure between large and small alveoli?
What is the role of surfactant in preventing alveolar collapse?
What is the role of surfactant in preventing alveolar collapse?
What is the equation that relates collapsing pressure, surface tension, and alveolar radius?
What is the equation that relates collapsing pressure, surface tension, and alveolar radius?
Why do small alveoli have a tendency to collapse?
Why do small alveoli have a tendency to collapse?
What is the effect of surfactant on alveolar compliance?
What is the effect of surfactant on alveolar compliance?
What is the relationship between alveolar radius and collapsing pressure?
What is the relationship between alveolar radius and collapsing pressure?
What is the relationship between the radius of the airway and the resistance to airflow?
What is the relationship between the radius of the airway and the resistance to airflow?
What is the primary site of airway resistance in the respiratory system?
What is the primary site of airway resistance in the respiratory system?
What is the effect of parasympathetic stimulation on airway resistance?
What is the effect of parasympathetic stimulation on airway resistance?
What is the effect of high lung volumes on airway resistance?
What is the effect of high lung volumes on airway resistance?
What is the effect of sympathetic stimulation on airway resistance?
What is the effect of sympathetic stimulation on airway resistance?
What is the relationship between airway radius and airflow?
What is the relationship between airway radius and airflow?
What is the effect of a 4-fold decrease in airway radius on resistance?
What is the effect of a 4-fold decrease in airway radius on resistance?
What is the mechanism by which lung volume affects airway resistance?
What is the mechanism by which lung volume affects airway resistance?
What is the reason why patients with COPD learn to expire slowly with 'pursed lips'?
What is the reason why patients with COPD learn to expire slowly with 'pursed lips'?
What is the characteristic of lung disease in patients with 'pink puffers'?
What is the characteristic of lung disease in patients with 'pink puffers'?
What is the effect of increased lung compliance in a patient with COPD?
What is the effect of increased lung compliance in a patient with COPD?
What is the characteristic of lung disease in patients with fibrosis?
What is the characteristic of lung disease in patients with fibrosis?
What is the effect of air trapping in patients with COPD?
What is the effect of air trapping in patients with COPD?
What is the characteristic of patients with 'blue bloaters'?
What is the characteristic of patients with 'blue bloaters'?
What is the effect of COPD on FEV1, FVC, and FEV1/FVC?
What is the effect of COPD on FEV1, FVC, and FEV1/FVC?
What is the shape of the chest in a patient with COPD?
What is the shape of the chest in a patient with COPD?
What is the main reason for the increase in FEV1/FVC in restrictive lung disease?
What is the main reason for the increase in FEV1/FVC in restrictive lung disease?
What is the partial pressure of oxygen in humidified tracheal air at 37°C?
What is the partial pressure of oxygen in humidified tracheal air at 37°C?
What is the effect of physiologic shunt on the Po2 of arterial blood?
What is the effect of physiologic shunt on the Po2 of arterial blood?
What is the relationship between the amount of gas dissolved in a solution and its partial pressure?
What is the relationship between the amount of gas dissolved in a solution and its partial pressure?
What is the characteristic of FEV1/FVC in obstructive lung disease, such as asthma and COPD?
What is the characteristic of FEV1/FVC in obstructive lung disease, such as asthma and COPD?
What is the correction factor for calculating the partial pressure of oxygen in humidified tracheal air?
What is the correction factor for calculating the partial pressure of oxygen in humidified tracheal air?
What is the effect of restrictive lung disease, such as fibrosis, on FEV1 and FVC?
What is the effect of restrictive lung disease, such as fibrosis, on FEV1 and FVC?
What is the equation for calculating the partial pressure of a gas?
What is the equation for calculating the partial pressure of a gas?
What is the concentration of dissolved oxygen in blood when the partial pressure of oxygen is 100 mmHg?
What is the concentration of dissolved oxygen in blood when the partial pressure of oxygen is 100 mmHg?
What is the partial pressure of oxygen in humidified tracheal air?
What is the partial pressure of oxygen in humidified tracheal air?
What is the partial pressure of carbon dioxide in alveolar air after equilibration with pulmonary capillary blood?
What is the partial pressure of carbon dioxide in alveolar air after equilibration with pulmonary capillary blood?
What is the effect of oxygen diffusion from alveolar air into pulmonary capillary blood on the partial pressure of oxygen?
What is the effect of oxygen diffusion from alveolar air into pulmonary capillary blood on the partial pressure of oxygen?
What is the reason for the difference in partial pressure of oxygen between arterial and mixed venous blood?
What is the reason for the difference in partial pressure of oxygen between arterial and mixed venous blood?
What is the effect of the addition of water to inspired air on the partial pressure of oxygen?
What is the effect of the addition of water to inspired air on the partial pressure of oxygen?
What is the primary factor that determines the diffusion rate of oxygen and carbon dioxide across the alveolar-pulmonary capillary membrane?
What is the primary factor that determines the diffusion rate of oxygen and carbon dioxide across the alveolar-pulmonary capillary membrane?
What is the equation that describes the diffusion of gases across the alveolar-pulmonary capillary membrane?
What is the equation that describes the diffusion of gases across the alveolar-pulmonary capillary membrane?
What happens to the lung diffusing capacity (DL) during exercise?
What happens to the lung diffusing capacity (DL) during exercise?
What type of gas exchange is illustrated by N2O and by O2 under normal conditions?
What type of gas exchange is illustrated by N2O and by O2 under normal conditions?
What is the effect of emphysema on the lung diffusing capacity (DL)?
What is the effect of emphysema on the lung diffusing capacity (DL)?
What is the effect of fibrosis on the lung diffusing capacity (DL)?
What is the effect of fibrosis on the lung diffusing capacity (DL)?
What is the relationship between the lung diffusing capacity (DL) and the diffusion coefficient of the gas?
What is the relationship between the lung diffusing capacity (DL) and the diffusion coefficient of the gas?
What is the equivalent of permeability of the alveolar-pulmonary capillary barrier?
What is the equivalent of permeability of the alveolar-pulmonary capillary barrier?
What is the primary limiting factor in perfusion-limited gas exchange?
What is the primary limiting factor in perfusion-limited gas exchange?
In which type of gas exchange does the partial pressure difference between alveolar air and pulmonary capillary blood remain throughout the length of the capillary?
In which type of gas exchange does the partial pressure difference between alveolar air and pulmonary capillary blood remain throughout the length of the capillary?
What is the effect of thickening of the alveolar membrane on oxygen diffusion?
What is the effect of thickening of the alveolar membrane on oxygen diffusion?
Which of the following is an example of a diffusion-limited gas?
Which of the following is an example of a diffusion-limited gas?
What is the primary function of hemoglobin in oxygen transport?
What is the primary function of hemoglobin in oxygen transport?
What is the result of decreased surface area for gas exchange in emphysema?
What is the result of decreased surface area for gas exchange in emphysema?
In diffusion-limited exchange, what happens to the partial pressure of the gas as blood flows through the pulmonary capillary?
In diffusion-limited exchange, what happens to the partial pressure of the gas as blood flows through the pulmonary capillary?
What is the primary mechanism of oxygen transport in the blood?
What is the primary mechanism of oxygen transport in the blood?
Which of the following is an example of a perfusion-limited gas?
Which of the following is an example of a perfusion-limited gas?
What is the primary cause of a high A-a gradient in a patient with fibrosis?
What is the primary cause of a high A-a gradient in a patient with fibrosis?
What is the value of the respiratory exchange ratio (R) used in the alveolar gas equation?
What is the value of the respiratory exchange ratio (R) used in the alveolar gas equation?
What is the normal range of the A-a gradient?
What is the normal range of the A-a gradient?
What is the equation used to calculate the A-a gradient?
What is the equation used to calculate the A-a gradient?
What is the primary factor that determines the A-a gradient?
What is the primary factor that determines the A-a gradient?
What is the effect of a right-to-left shunt on the A-a gradient?
What is the effect of a right-to-left shunt on the A-a gradient?
What is the primary cause of increased A-a gradient?
What is the primary cause of increased A-a gradient?
What is the effect of decreased hemoglobin concentration on oxygen delivery?
What is the effect of decreased hemoglobin concentration on oxygen delivery?
What is the mechanism by which hypoxia-inducible factor 1a is produced in response to hypoxia?
What is the mechanism by which hypoxia-inducible factor 1a is produced in response to hypoxia?
What is the effect of cyanide poisoning on oxygen delivery?
What is the effect of cyanide poisoning on oxygen delivery?
What is the role of erythropoietin in response to hypoxia?
What is the role of erythropoietin in response to hypoxia?
What is the equation that describes oxygen delivery?
What is the equation that describes oxygen delivery?
What is the enzyme that facilitates the reaction between CO2 and H2O to form H2CO3 in the red blood cells?
What is the enzyme that facilitates the reaction between CO2 and H2O to form H2CO3 in the red blood cells?
What is the major form in which CO2 is transported to the lungs?
What is the major form in which CO2 is transported to the lungs?
What is the purpose of the chloride shift in red blood cells?
What is the purpose of the chloride shift in red blood cells?
Why is deoxyhemoglobin a better buffer for H+ ions than oxyhemoglobin?
Why is deoxyhemoglobin a better buffer for H+ ions than oxyhemoglobin?
What is the significance of the deoxygenation of hemoglobin by the time blood reaches the venous end of the capillaries?
What is the significance of the deoxygenation of hemoglobin by the time blood reaches the venous end of the capillaries?
What is the purpose of the hydration reaction of CO2 in the red blood cells?
What is the purpose of the hydration reaction of CO2 in the red blood cells?
What is the percentage of cardiac output that bypasses the lungs in right-to-left shunts under normal conditions?
What is the percentage of cardiac output that bypasses the lungs in right-to-left shunts under normal conditions?
What happens to the arterial P~ when a right-to-left shunt occurs?
What happens to the arterial P~ when a right-to-left shunt occurs?
What is the direction of blood flow in a left-to-right shunt?
What is the direction of blood flow in a left-to-right shunt?
What is the approximate V/Q ratio in a normal individual?
What is the approximate V/Q ratio in a normal individual?
What is the effect of a left-to-right shunt on arterial P~?
What is the effect of a left-to-right shunt on arterial P~?
What is the purpose of having the patient breathe 100% O2 to estimate the magnitude of a right-to-left shunt?
What is the purpose of having the patient breathe 100% O2 to estimate the magnitude of a right-to-left shunt?
What is the effect of gravitational forces on arterial pressure in the upright lung?
What is the effect of gravitational forces on arterial pressure in the upright lung?
Which of the following statements is true about the V/Q ratio in the lung?
Which of the following statements is true about the V/Q ratio in the lung?
What is the effect of a complete airway blockage on the V/Q ratio?
What is the effect of a complete airway blockage on the V/Q ratio?
What is the relationship between Po2 and Pco2 at the apex and base of the lung?
What is the relationship between Po2 and Pco2 at the apex and base of the lung?
What is the primary reason for the regional differences in ventilation in the upright lung?
What is the primary reason for the regional differences in ventilation in the upright lung?
What is the effect of the regional differences in V/Q ratio on gas exchange?
What is the effect of the regional differences in V/Q ratio on gas exchange?
Which nerve relays information from peripheral chemoreceptors and mechanoreceptors in the lung?
Which nerve relays information from peripheral chemoreceptors and mechanoreceptors in the lung?
What is the effect of airway obstruction on the composition of systemic arterial blood?
What is the effect of airway obstruction on the composition of systemic arterial blood?
What is the primary function of the dorsal respiratory group?
What is the primary function of the dorsal respiratory group?
Where is the pneumotaxic center located?
Where is the pneumotaxic center located?
What is the condition where blood flow to a lung is completely blocked, leading to zero blood flow, but ventilation is normal?
What is the condition where blood flow to a lung is completely blocked, leading to zero blood flow, but ventilation is normal?
What is the location of the medullary respiratory center?
What is the location of the medullary respiratory center?
What is the role of central chemoreceptors in the medulla?
What is the role of central chemoreceptors in the medulla?
What is the primary function of the apneustic center?
What is the primary function of the apneustic center?
What is the effect of a pulmonary embolus on the composition of alveolar gas?
What is the effect of a pulmonary embolus on the composition of alveolar gas?
What is the term for the situation where ventilation is normal, but blood flow is zero?
What is the term for the situation where ventilation is normal, but blood flow is zero?
What is the role of the ventral respiratory group?
What is the role of the ventral respiratory group?
What is the effect of a ventilation-perfusion defect on gas exchange?
What is the effect of a ventilation-perfusion defect on gas exchange?
What is the effect of hyperventilation on breath-holding?
What is the effect of hyperventilation on breath-holding?
What is the coordinating center for sensory information in the brain?
What is the coordinating center for sensory information in the brain?
What is the effect of a decrease in pH of the cerebrospinal fluid (CSF) on breathing rate?
What is the effect of a decrease in pH of the cerebrospinal fluid (CSF) on breathing rate?
Why does CO2 diffuse from arterial blood into the CSF?
Why does CO2 diffuse from arterial blood into the CSF?
What happens when CO2 combines with H2O in the CSF?
What happens when CO2 combines with H2O in the CSF?
What is the effect of an increase in Pco2 and [H+] on breathing rate?
What is the effect of an increase in Pco2 and [H+] on breathing rate?
What is the response of peripheral chemoreceptors to a decrease in arterial Pco2?
What is the response of peripheral chemoreceptors to a decrease in arterial Pco2?
Where are the carotid bodies located?
Where are the carotid bodies located?
What is the effect of hyperventilation or hypoventilation on arterial Pco2?
What is the effect of hyperventilation or hypoventilation on arterial Pco2?
Why do decreases in pH of the CSF produce increases in breathing rate?
Why do decreases in pH of the CSF produce increases in breathing rate?
What is the role of the central chemoreceptors in regulating breathing?
What is the role of the central chemoreceptors in regulating breathing?
Flashcards
Tidal Volume (VT)
Tidal Volume (VT)
Volume inspired or expired with each normal breath.
Inspiratory Reserve Volume (IRV)
Inspiratory Reserve Volume (IRV)
Volume that can be inspired over and above the tidal volume; used during exercise.
Expiratory Reserve Volume (ERV)
Expiratory Reserve Volume (ERV)
Volume that can be expired after the expiration of a tidal volume.
Residual Volume (RV)
Residual Volume (RV)
Signup and view all the flashcards
Dead Space
Dead Space
Signup and view all the flashcards
Anatomic Dead Space
Anatomic Dead Space
Signup and view all the flashcards
Physiologic Dead Space
Physiologic Dead Space
Signup and view all the flashcards
Compliance
Compliance
Signup and view all the flashcards
Diaphragm
Diaphragm
Signup and view all the flashcards
Abdominal Muscles (Expiration)
Abdominal Muscles (Expiration)
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD)
Signup and view all the flashcards
Emphysema
Emphysema
Signup and view all the flashcards
Chronic Bronchitis
Chronic Bronchitis
Signup and view all the flashcards
Fibrosis
Fibrosis
Signup and view all the flashcards
Dalton's Law of Partial Pressures
Dalton's Law of Partial Pressures
Signup and view all the flashcards
Dissolved Gases
Dissolved Gases
Signup and view all the flashcards
Lung Diffusing Capacity (DL)
Lung Diffusing Capacity (DL)
Signup and view all the flashcards
A-a Gradient
A-a Gradient
Signup and view all the flashcards
Causes of Hypoxemia
Causes of Hypoxemia
Signup and view all the flashcards
Erythropoietin (EPO)
Erythropoietin (EPO)
Signup and view all the flashcards
Hypoxia-Inducible Factor 1α
Hypoxia-Inducible Factor 1α
Signup and view all the flashcards
CO2 Transport Forms
CO2 Transport Forms
Signup and view all the flashcards
CO2 in RBCs
CO2 in RBCs
Signup and view all the flashcards
Chloride Shift
Chloride Shift
Signup and view all the flashcards
H+ Buffering in RBCs
H+ Buffering in RBCs
Signup and view all the flashcards
Right-to-Left Shunts
Right-to-Left Shunts
Signup and view all the flashcards
V/Q Ratio
V/Q Ratio
Signup and view all the flashcards
V/Q in Airway Obstruction
V/Q in Airway Obstruction
Signup and view all the flashcards
V/Q in Pulmonary Embolism
V/Q in Pulmonary Embolism
Signup and view all the flashcards
Study Notes
Here are the study notes:
- Respiratory Physiology*
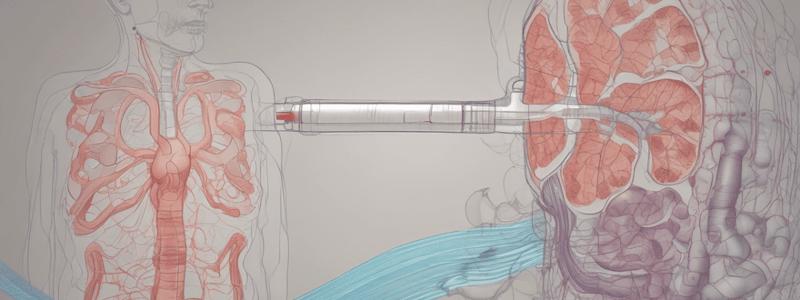
Lung Volumes and Capacities
- Tidal volume (VT): volume inspired or expired with each normal breath
- Inspiratory reserve volume (IRV): volume that can be inspired over and above the tidal volume, used during exercise
- Expiratory reserve volume (ERV): volume that can be expired after the expiration of a tidal volume
- Residual volume (RV): volume that remains in the lungs after a maximal expiration, cannot be measured by spirometry
- Dead space: volume of the lungs that does not participate in gas exchange
- Anatomic dead space: volume of the conducting airways (approximately 150 mL)
- Physiologic dead space: functional measurement of the volume of the lungs that does not participate in gas exchange (approximately equal to anatomic dead space in normal lungs, but may be greater in lung diseases with ventilation/perfusion defects)
Compliance of the Respiratory System
- Compliance: describes the distensibility of the lungs and chest wall
- Equation: C = ΔV / ΔP
- Describes the change in volume for a given change in pressure
- Inversely related to elastance and stiffness
Muscles of Inspiration and Expiration
- Muscles of inspiration:
- Diaphragm: most important muscle for inspiration
- External intercostal muscles: not used for inspiration during normal quiet breathing, but used during exercise and in respiratory distress
- Muscles of expiration:
- Abdominal muscles: compress the abdominal cavity, push the diaphragm up, and push air out of the lungs
- Internal intercostal muscles: pull the ribs downward and inward
Lung Disease
- Asthma: obstructive disease, expiration is impaired, characterized by decreased FVC, FEV1, and FEV1/FVC
- Chronic Obstructive Pulmonary Disease (COPD): obstructive disease with increased lung compliance, expiration is impaired, characterized by decreased FVC, FEV1, and FEV1/FVC
- Emphysema: "pink puffers" (mild hypoxemia, normal PCO2)
- Chronic bronchitis: "blue bloaters" (severe hypoxemia with cyanosis, hypercapnia, and right ventricular failure)
- Fibrosis: restrictive disease, inspiration is impaired, characterized by a decrease in all lung volumes
Gas Exchange
- Dalton's law of partial pressures: P = PT x F
- Partial pressure of O2 and CO2 in inspired air, alveolar air, and blood
- Dissolved gases: amount of gas dissolved in a solution is proportional to its partial pressure
- Diffusion of gases: rates depend on partial pressure differences across the membrane and the area available for diffusion
- Lung diffusing capacity (DL): equivalent to permeability of the alveolar-pulmonary capillary barrier
Oxygen Transport
-
Oxygen is carried in blood in two forms: dissolved or bound to hemoglobin
-
Hemoglobin increases the O2-carrying capacity of blood 70-fold
-
A-a gradient: difference in PO2 between alveolar gas and arterial blood
-
Causes of hypoxemia:
- High altitude
- Hypoventilation
- Diffusion defect
- V/Q defect
- Right-to-left shunt
-
Erythropoietin (EPO): a growth factor that is synthesized in the kidneys in response to hypoxia### Hypoxia-Inducible Factor and EPO
-
Hypoxia-inducible factor 1α directs the synthesis of mRNA for EPO, which promotes the development of mature red blood cells.
CO2 Transport
- CO2 is transported in three forms: dissolved CO2, carbaminohemoglobin, and HCO3- (the major form, accounting for 90%)
- In the RBCs, CO2 combines with H2O to form H2CO3, which dissociates into H+ and HCO3-
- HCO3- leaves the RBCs in exchange for Cl- (chloride shift) and is transported to the lungs in the plasma
- H+ is buffered inside the RBCs by deoxyhemoglobin, which is a better buffer for H+ than oxyhemoglobin
Shunts
- Right-to-left shunts occur when 2% of the cardiac output bypasses the lungs, resulting in a decrease in arterial P02
- May be as great as 50% of cardiac output in certain congenital abnormalities, such as tetralogy of Fallot
- Left-to-right shunts are more common, caused by congenital abnormalities or traumatic injury, and do not result in a decrease in arterial P02
V/Q Defects
- V/Q ratio is the ratio of alveolar ventilation (V) to pulmonary blood flow (Q)
- Ventilation and perfusion (blood flow) matching is important for achieving the ideal exchange of O2 and CO2
- Normal V/Q ratio is approximately 0.8, resulting in an arterial P02 of 100 mm Hg and an arterial Pco2 of 40 mm Hg
- Regional variations in the lung of perfusion, ventilation, V/Q, P02, and Pco2 occur due to gravitational effects
- V/Q ratio is higher at the apex and lower at the base of the lung
- As a result, gas exchange is more efficient at the apex and less efficient at the base
Changes in V/Q Ratio
- V/Q ratio in airway obstruction: If airways are completely blocked, then ventilation is zero, resulting in a V/Q ratio of 0
- V/Q ratio in pulmonary embolism: If blood flow to a lung is completely blocked, then blood flow to that lung is zero, resulting in a V/Q ratio of infinity (dead space)
Control of Breathing
- Central control of breathing involves the brainstem and cerebral cortex
- Medullary respiratory center is located in the reticular formation and responds to changes in pH of the CSF
- Peripheral chemoreceptors in the carotid and aortic bodies respond to changes in arterial P02
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.