Podcast
Questions and Answers
Which receptor subtype, when activated, stimulates a G protein that inhibits adenylyl cyclase and increases K+ conduction, leading to decreased heart rate and contraction force?
Which receptor subtype, when activated, stimulates a G protein that inhibits adenylyl cyclase and increases K+ conduction, leading to decreased heart rate and contraction force?
- M1
- M3
- Nicotinic receptors
- M2 (correct)
Which of the following receptors is found on parietal cells of the stomach?
Which of the following receptors is found on parietal cells of the stomach?
- M1 (correct)
- M3
- M2
- Nicotinic receptors
What is the primary effect of activating M1 or M3 receptors?
What is the primary effect of activating M1 or M3 receptors?
- Increase in intracellular Ca++ (correct)
- Inhibition of adenylyl cyclase
- Inhibition of Ca++ channels
- Stimulation of phospholipase A2
Which of the following drugs selectively inhibits M1 receptors in the gastric mucosa and is useful in the treatment of gastric and duodenal ulcers?
Which of the following drugs selectively inhibits M1 receptors in the gastric mucosa and is useful in the treatment of gastric and duodenal ulcers?
Which of the following receptors are found in the central nervous system (CNS), adrenal medulla, autonomic ganglia, and the neuromuscular junction?
Which of the following receptors are found in the central nervous system (CNS), adrenal medulla, autonomic ganglia, and the neuromuscular junction?
What is the primary effect of activating the M2 subtype on cardiac muscle?
What is the primary effect of activating the M2 subtype on cardiac muscle?
Which of the following is a direct-acting cholinergic agonist that mimics the effects of acetylcholine by binding directly to cholinoceptors?
Which of the following is a direct-acting cholinergic agonist that mimics the effects of acetylcholine by binding directly to cholinoceptors?
Which of the following receptors show only a weak affinity for muscarine?
Which of the following receptors show only a weak affinity for muscarine?
What is the primary use of pilocarpine in the context provided?
What is the primary use of pilocarpine in the context provided?
What is the mechanism of action of acetylcholinesterase inhibitors in the treatment of Alzheimer's disease?
What is the mechanism of action of acetylcholinesterase inhibitors in the treatment of Alzheimer's disease?
What is the primary use of physostigmine in the context provided?
What is the primary use of physostigmine in the context provided?
What is the mechanism of action of physostigmine as an acetylcholinesterase inhibitor?
What is the mechanism of action of physostigmine as an acetylcholinesterase inhibitor?
What is the effect of placing physostigmine topically in the eye?
What is the effect of placing physostigmine topically in the eye?
What is the duration of action of physostigmine?
What is the duration of action of physostigmine?
What is the primary side effect of pilocarpine mentioned in the text?
What is the primary side effect of pilocarpine mentioned in the text?
What is the primary mechanism of action of acetylcholinesterase inhibitors?
What is the primary mechanism of action of acetylcholinesterase inhibitors?
What is the primary mechanism of action of epinephrine in relieving bronchospasm?
What is the primary mechanism of action of epinephrine in relieving bronchospasm?
Which of the following is NOT a mechanism by which epinephrine can increase blood glucose levels?
Which of the following is NOT a mechanism by which epinephrine can increase blood glucose levels?
Which of the following is NOT a potential adverse effect of epinephrine?
Which of the following is NOT a potential adverse effect of epinephrine?
In which of the following conditions should the dose of epinephrine be reduced?
In which of the following conditions should the dose of epinephrine be reduced?
Which enzyme is primarily responsible for the metabolism of epinephrine?
Which enzyme is primarily responsible for the metabolism of epinephrine?
In which of the following scenarios would the use of epinephrine be contraindicated?
In which of the following scenarios would the use of epinephrine be contraindicated?
Which of the following drug interactions is most significant when using epinephrine?
Which of the following drug interactions is most significant when using epinephrine?
Which route of administration of epinephrine is most appropriate in an emergency situation like anaphylactic shock?
Which route of administration of epinephrine is most appropriate in an emergency situation like anaphylactic shock?
Which statement about atropine is correct?
Which statement about atropine is correct?
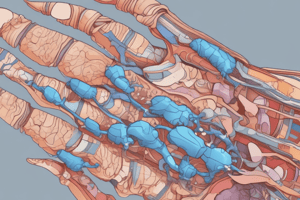
What is recommended as part of the nonpharmacologic therapy for acute gouty arthritis?
What is recommended as part of the nonpharmacologic therapy for acute gouty arthritis?
Which adverse effect is specifically associated with oral colchicine during an acute gout attack?
Which adverse effect is specifically associated with oral colchicine during an acute gout attack?
Which of the following is NOT a use of atropine?
Which of the following is NOT a use of atropine?
Which receptor type does atropine primarily target?
Which receptor type does atropine primarily target?
When is colchicine most effective in relieving acute gout attacks?
When is colchicine most effective in relieving acute gout attacks?
Which statement about the duration of action of atropine is correct?
Which statement about the duration of action of atropine is correct?
What can worsen the neutropenia and axonal neuromyopathy associated with colchicine use?
What can worsen the neutropenia and axonal neuromyopathy associated with colchicine use?
Which of the following is NOT a common non-GI adverse effect of colchicine?
Which of the following is NOT a common non-GI adverse effect of colchicine?
Which statement about the effects of atropine on the eye is correct?
Which statement about the effects of atropine on the eye is correct?
Which statement about the effects of atropine on secretions is correct?
Which statement about the effects of atropine on secretions is correct?
What effect does joint rest for 1 to 2 days have on acute gouty arthritis?
What effect does joint rest for 1 to 2 days have on acute gouty arthritis?
Why may patients be advised to reduce intake of foods high in purines?
Why may patients be advised to reduce intake of foods high in purines?
What impact does losing weight have on the treatment of acute gouty arthritis?
What impact does losing weight have on the treatment of acute gouty arthritis?
Which statement about the use of atropine in the respiratory system is correct?
Which statement about the use of atropine in the respiratory system is correct?
Which statement about the use of atropine in the gastrointestinal tract is correct?
Which statement about the use of atropine in the gastrointestinal tract is correct?
Which of the following is the most important factor in determining if prophylactic treatment for gout should be instituted immediately after resolution of an acute attack?
Which of the following is the most important factor in determining if prophylactic treatment for gout should be instituted immediately after resolution of an acute attack?
What is the recommended oral dose of colchicine for prophylactic treatment of gout in patients with no evidence of visible tophi and a normal or slightly elevated serum urate concentration?
What is the recommended oral dose of colchicine for prophylactic treatment of gout in patients with no evidence of visible tophi and a normal or slightly elevated serum urate concentration?
When should patients on prophylactic colchicine treatment increase the dose during an acute gout attack?
When should patients on prophylactic colchicine treatment increase the dose during an acute gout attack?
When can discontinuation of prophylactic gout treatment be attempted?
When can discontinuation of prophylactic gout treatment be attempted?
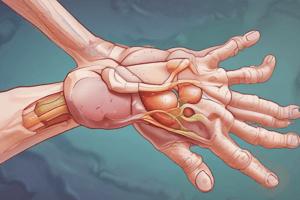
What is the primary criterion for using uricosuric drugs like probenecid and sulfinpyrazone for gout prophylaxis?
What is the primary criterion for using uricosuric drugs like probenecid and sulfinpyrazone for gout prophylaxis?
What is the recommended approach when starting treatment with uricosuric drugs for gout prophylaxis?
What is the recommended approach when starting treatment with uricosuric drugs for gout prophylaxis?
What is the primary reason patients with gout are advised to reduce intake of foods high in purines?
What is the primary reason patients with gout are advised to reduce intake of foods high in purines?
What is the recommended duration of joint rest for acute gouty arthritis?
What is the recommended duration of joint rest for acute gouty arthritis?
Which phase is associated with the initial depolarization of the receptor and transient muscle fasciculation caused by depolarizing neuromuscular blockers?
Which phase is associated with the initial depolarization of the receptor and transient muscle fasciculation caused by depolarizing neuromuscular blockers?
What is the primary mode of action of non-depolarizing (competitive) neuromuscular blockers at low doses?
What is the primary mode of action of non-depolarizing (competitive) neuromuscular blockers at low doses?
Which of the following agents can be used to reverse the effects of non-depolarizing neuromuscular blockers?
Which of the following agents can be used to reverse the effects of non-depolarizing neuromuscular blockers?
Which of the following statements is true regarding the use of depolarizing neuromuscular blockers for endotracheal intubation?
Which of the following statements is true regarding the use of depolarizing neuromuscular blockers for endotracheal intubation?
What is the primary reason for the development of newer non-depolarizing neuromuscular blockers over older agents like tubocurarine?
What is the primary reason for the development of newer non-depolarizing neuromuscular blockers over older agents like tubocurarine?
Which phase is characterized by the gradual repolarization of the receptor and flaccid paralysis caused by depolarizing neuromuscular blockers?
Which phase is characterized by the gradual repolarization of the receptor and flaccid paralysis caused by depolarizing neuromuscular blockers?
Which of the following is a potential side effect associated with the use of depolarizing neuromuscular blockers?
Which of the following is a potential side effect associated with the use of depolarizing neuromuscular blockers?
What is the primary advantage of using non-depolarizing neuromuscular blockers over depolarizing agents during general anesthesia?
What is the primary advantage of using non-depolarizing neuromuscular blockers over depolarizing agents during general anesthesia?
What is the primary mechanism of action of carbachol (carbamylcholine) in the context provided?
What is the primary mechanism of action of carbachol (carbamylcholine) in the context provided?
What is the primary use of pilocarpine mentioned in the text?
What is the primary use of pilocarpine mentioned in the text?
What is the primary side effect of pilocarpine mentioned in the text?
What is the primary side effect of pilocarpine mentioned in the text?
What is the primary effect of activating M2 receptors on cardiac muscle?
What is the primary effect of activating M2 receptors on cardiac muscle?
Which of the following is a direct-acting cholinergic agonist that mimics the effects of acetylcholine by binding directly to cholinoceptors?
Which of the following is a direct-acting cholinergic agonist that mimics the effects of acetylcholine by binding directly to cholinoceptors?
What is the primary mechanism of action of acetylcholinesterase inhibitors, such as physostigmine, in the context provided?
What is the primary mechanism of action of acetylcholinesterase inhibitors, such as physostigmine, in the context provided?
What is the duration of action of carbachol (carbamylcholine) compared to acetylcholine?
What is the duration of action of carbachol (carbamylcholine) compared to acetylcholine?
What is the primary mechanism by which ephedrine causes bronchodilation?
What is the primary mechanism by which ephedrine causes bronchodilation?
Which of the following is the LEAST potent among the bronchodilators mentioned in the text?
Which of the following is the LEAST potent among the bronchodilators mentioned in the text?
Which of the following is the primary reason why ephedrine is better suited for prophylactic use in asthma than for acute attacks?
Which of the following is the primary reason why ephedrine is better suited for prophylactic use in asthma than for acute attacks?
How does phenoxybenzamine primarily differ from other alpha-adrenergic antagonists in its mechanism of action?
How does phenoxybenzamine primarily differ from other alpha-adrenergic antagonists in its mechanism of action?
What is the primary effect of phenoxybenzamine on the cardiovascular system?
What is the primary effect of phenoxybenzamine on the cardiovascular system?
How does phenoxybenzamine's effect on alpha-2 receptors contribute to its overall cardiovascular effects?
How does phenoxybenzamine's effect on alpha-2 receptors contribute to its overall cardiovascular effects?
What is the primary mechanism by which phenoxybenzamine reverses the actions of epinephrine?
What is the primary mechanism by which phenoxybenzamine reverses the actions of epinephrine?
What is the primary therapeutic use of ephedrine mentioned in the text?
What is the primary therapeutic use of ephedrine mentioned in the text?
Which muscle group is typically paralyzed first when using non-depolarizing muscle relaxants?
Which muscle group is typically paralyzed first when using non-depolarizing muscle relaxants?
Which of the following is NOT a reason why non-depolarizing muscle relaxants are not administered orally?
Which of the following is NOT a reason why non-depolarizing muscle relaxants are not administered orally?
Which of the following non-depolarizing muscle relaxants undergoes spontaneous degradation in plasma, followed by ester hydrolysis?
Which of the following non-depolarizing muscle relaxants undergoes spontaneous degradation in plasma, followed by ester hydrolysis?
Which of the following is a potential adverse effect associated with the metabolite laudanosine, produced during the metabolism of atracurium?
Which of the following is a potential adverse effect associated with the metabolite laudanosine, produced during the metabolism of atracurium?
Which class of antibiotics can potentiate the neuromuscular blockade caused by non-depolarizing muscle relaxants?
Which class of antibiotics can potentiate the neuromuscular blockade caused by non-depolarizing muscle relaxants?
Which of the following non-depolarizing muscle relaxants is an aminosteroid drug that undergoes deacetylation in the liver?
Which of the following non-depolarizing muscle relaxants is an aminosteroid drug that undergoes deacetylation in the liver?
Which of the following statements regarding the interaction between halogenated hydrocarbon anesthetics and non-depolarizing muscle relaxants is correct?
Which of the following statements regarding the interaction between halogenated hydrocarbon anesthetics and non-depolarizing muscle relaxants is correct?
Which of the following drugs can overcome the neuromuscular blockade caused by non-depolarizing muscle relaxants?
Which of the following drugs can overcome the neuromuscular blockade caused by non-depolarizing muscle relaxants?
Flashcards are hidden until you start studying