Podcast
Questions and Answers
What is the primary factor that determines the induction of anesthesia?
What is the primary factor that determines the induction of anesthesia?
- Depth of CNS depression
- Consciousness and protective reflexes regained
- Rate of anesthetic diffusion from the brain
- Rate of effective concentration of the anesthetic reaching the brain (correct)
What is the main difference between induction and recovery?
What is the main difference between induction and recovery?
- Induction is faster, while recovery is slower
- Induction involves an increase in CNS depression, while recovery involves its decrease (correct)
- Induction is the development of surgical anesthesia, while recovery is the regain of consciousness
- Induction is the administration of anesthesia, while recovery is its discontinuation
What is the primary goal of maintenance of anesthesia?
What is the primary goal of maintenance of anesthesia?
- To induce surgical anesthesia
- To regain consciousness
- To provide pain relief
- To sustain surgical anesthesia (correct)
What is the characteristic of the first stage of anesthesia?
What is the characteristic of the first stage of anesthesia?
What is the last stage of anesthesia?
What is the last stage of anesthesia?
What happens to the CNS during the progression of anesthesia stages?
What happens to the CNS during the progression of anesthesia stages?
What is the term for the degree to which the CNS is depressed?
What is the term for the degree to which the CNS is depressed?
What happens to the patient's consciousness during the first stage of anesthesia?
What happens to the patient's consciousness during the first stage of anesthesia?
What does the Greek word 'anaesthesia' mean?
What does the Greek word 'anaesthesia' mean?
What is the primary characteristic of general anaesthesia?
What is the primary characteristic of general anaesthesia?
What is the term for the agents that produce general anaesthesia?
What is the term for the agents that produce general anaesthesia?
What is the characteristic of regional anaesthesia?
What is the characteristic of regional anaesthesia?
In which stage of general anaesthesia is the patient most responsive?
In which stage of general anaesthesia is the patient most responsive?
What is the primary goal of general anaesthesia?
What is the primary goal of general anaesthesia?
What is the term for the drugs used to produce local anaesthesia?
What is the term for the drugs used to produce local anaesthesia?
What is the state of general anaesthesia characterized by?
What is the state of general anaesthesia characterized by?
What is the primary goal of ideal general anesthesia?
What is the primary goal of ideal general anesthesia?
What is the term used to describe the use of a combination of drugs to produce rapid induction of anesthesia and to ensure rapid recovery from the effects of GA with fewer side effects?
What is the term used to describe the use of a combination of drugs to produce rapid induction of anesthesia and to ensure rapid recovery from the effects of GA with fewer side effects?
Which of the following drugs is NOT an example of a pre-anesthetic agent?
Which of the following drugs is NOT an example of a pre-anesthetic agent?
What is the primary role of neuromuscular relaxants in balanced anesthesia?
What is the primary role of neuromuscular relaxants in balanced anesthesia?
What is the classification of general anesthetics based on?
What is the classification of general anesthetics based on?
What type of anesthetics are used to maintain anesthesia during surgery?
What type of anesthetics are used to maintain anesthesia during surgery?
Which of the following is a non-halogenated inhalation anesthetic?
Which of the following is a non-halogenated inhalation anesthetic?
What is the primary advantage of balanced anesthesia?
What is the primary advantage of balanced anesthesia?
Which intravenous anesthetic is a carboxylated imidazole?
Which intravenous anesthetic is a carboxylated imidazole?
Which of the following is NOT a characteristic of an ideal general anesthetic drug?
Which of the following is NOT a characteristic of an ideal general anesthetic drug?
What is the term used to describe the use of a single drug for induction and maintenance of anesthesia?
What is the term used to describe the use of a single drug for induction and maintenance of anesthesia?
What is the advantage of using thiopental, propofol, and etomidate over inhaled agents?
What is the advantage of using thiopental, propofol, and etomidate over inhaled agents?
Which of the following is a barbiturate intravenous anesthetic?
Which of the following is a barbiturate intravenous anesthetic?
What is the mechanism of action of benzodiazepines as intravenous anesthetics?
What is the mechanism of action of benzodiazepines as intravenous anesthetics?
Which of the following is a non-barbiturate intravenous anesthetic?
Which of the following is a non-barbiturate intravenous anesthetic?
What is the brand name of the opioid fentanyl?
What is the brand name of the opioid fentanyl?
Which of the following inhalation anesthetics is a non-flammable halogenated hydrocarbon?
Which of the following inhalation anesthetics is a non-flammable halogenated hydrocarbon?
What is the primary function of inhalation anesthesia?
What is the primary function of inhalation anesthesia?
Which of the following factors affects the transfer of general anesthetic from the lung to the blood and then to the brain?
Which of the following factors affects the transfer of general anesthetic from the lung to the blood and then to the brain?
What is the MAC of nitrous oxide (N2O)?
What is the MAC of nitrous oxide (N2O)?
What is the effect of increasing the anesthetic concentration in the inspired air?
What is the effect of increasing the anesthetic concentration in the inspired air?
Which of the following inhalation anesthetics is an inorganic agent?
Which of the following inhalation anesthetics is an inorganic agent?
How does the potency of halothane compare to enflurane?
How does the potency of halothane compare to enflurane?
What is the effect of increased pulmonary ventilation on the rate of induction?
What is the effect of increased pulmonary ventilation on the rate of induction?
Flashcards are hidden until you start studying
Study Notes
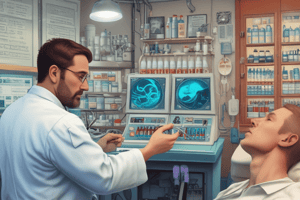
Anesthesia
- Anesthesia is a Greek word that means "loss of sensation".
- There are three types of anesthesia: General Anaesthesia, Regional Anaesthesia, and Local Anaesthesia.
General Anaesthesia
- General Anaesthesia is a state of reversible CNS inhibition characterized by loss of consciousness, sensation, and motor activity.
- It can be divided into three stages: Induction, Maintenance, and Recovery.
- Induction is the period of time from the onset of administration of the potent anesthetic to the development of effective surgical anesthesia in the patient.
- Maintenance provides a sustained surgical anesthesia.
- Recovery is the time from discontinuation of administration of anesthesia until consciousness and protective physiologic reflexes are regained.
Stages of Anesthesia (Depth)
- Anesthesia can be divided into a series of four stages, each characterized by an increase in CNS depression caused by the accumulation of the anesthetic drug in the brain.
- The four stages are: Analgesia, Excitement, Surgical Anesthesia, and Medullary Paralysis.
- Stage I (stage of analgesia) is characterized by reduced sensation of pain, with the patient remaining conscious and conversational.
Ideal General Anesthesia
- Ideal general anesthesia should rapidly and smoothly induce anesthesia, permit rapid recovery, and have a wide margin of safety with no adverse effects.
Balanced Anesthesia
- Balanced anesthesia is a protocol that uses a combination of different drugs to produce rapid induction of anesthesia and ensure rapid recovery from the effects of GA with fewer side effects.
- The drugs used in balanced anesthesia include pre-anesthetic agents, induction agents, maintenance agents, and neuromuscular relaxants.
Classification of General Anesthetics
- General anesthetics can be classified into two categories based on the route of administration: Inhalation Anesthetics and Intravenous Anesthetics.
- Inhalation anesthetics include halogenated hydrocarbons (e.g., halothane, enflurane, isoflurane, sevoflurane) and non-halogenated gases (e.g., nitrous oxide, diethylether).
- Intravenous anesthetics include barbiturates (e.g., sodium thiopentone, methohexitone), non-barbiturates (e.g., propofol, opioids, benzodiazepines, etomidate, ketamine).
Minimum Alveolar Concentration (MAC)
- MAC is the minimum alveolar concentration of an anesthetic agent required to eliminate movement among 50% of patients when exposed to skin incision.
- MAC varies among different anesthetic agents, with higher MAC indicating lower potency (e.g., MAC of N2O = 100, MAC of halothane = 0.75).
Factors Affecting Transfer of GA
- The transfer of general anesthesia from lung to blood to brain is affected by several factors, including solubility in blood, anesthetic concentration in the inspired air, pulmonary ventilation, and cardiac output.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.