Podcast
Questions and Answers
In the context of acid-base balance, what is the primary role of a buffer system?
In the context of acid-base balance, what is the primary role of a buffer system?
- To completely neutralize strong acids and bases in a solution.
- To maintain pH stability by resisting changes in hydrogen ion concentration. (correct)
- To exponentially amplify changes in pH to signal metabolic shifts.
- To selectively remove only strong acids from biological systems.
What does the Henderson-Hasselbalch equation allow one to determine?
What does the Henderson-Hasselbalch equation allow one to determine?
- The precise color change of an indicator at different pH levels.
- The exact speed of an acid-base reaction in any solution.
- The concentration of strong acids needed to neutralize a strong base.
- The ionisation state of weak acids and bases at a given pH. (correct)
Which factor most significantly affects the buffering capacity of a buffer system?
Which factor most significantly affects the buffering capacity of a buffer system?
- The concentration of the buffer components. (correct)
- The presence of strong oxidizing agents.
- The temperature of the solution.
- The atmospheric pressure applied to the solution.
What is a crucial function of the bicarbonate buffer system in the human body?
What is a crucial function of the bicarbonate buffer system in the human body?
Why is maintaining blood pH within a narrow range crucial for human health?
Why is maintaining blood pH within a narrow range crucial for human health?
What is the effect of changes in intracellular fluid pH on extracellular pH?
What is the effect of changes in intracellular fluid pH on extracellular pH?
Under what condition might acidosis or alkalosis become life-threatening?
Under what condition might acidosis or alkalosis become life-threatening?
According to Le Chatelier's principle, how does a buffer system counteract changes in pH?
According to Le Chatelier's principle, how does a buffer system counteract changes in pH?
What does the effectiveness of a buffer system depend on, according to the provided materials?
What does the effectiveness of a buffer system depend on, according to the provided materials?
What roles do the kidneys play in maintaining buffer capacity within the body?
What roles do the kidneys play in maintaining buffer capacity within the body?
What is the significance of the Bohr effect in the context of blood buffering?
What is the significance of the Bohr effect in the context of blood buffering?
In the context of acid-base balance, what is the primary role of the lungs?
In the context of acid-base balance, what is the primary role of the lungs?
Which of the following is an example of a biologically important buffer system?
Which of the following is an example of a biologically important buffer system?
Why is the bicarbonate buffer system considered an 'open' system?
Why is the bicarbonate buffer system considered an 'open' system?
What is the primary mechanism by which the lungs influence the bicarbonate buffer system?
What is the primary mechanism by which the lungs influence the bicarbonate buffer system?
During metabolic acidosis, what compensatory mechanism does the body typically employ?
During metabolic acidosis, what compensatory mechanism does the body typically employ?
How does hyperventilation affect the pH of the blood?
How does hyperventilation affect the pH of the blood?
During hypoxia, what adaptation occurs at the level of cytochrome oxidase (Complex 4 of ETC)?
During hypoxia, what adaptation occurs at the level of cytochrome oxidase (Complex 4 of ETC)?
What is the role of carbonic anhydrase in the bicarbonate buffer system?
What is the role of carbonic anhydrase in the bicarbonate buffer system?
How do changes in the rate of breathing affect the concentration of carbon dioxide in the blood?
How do changes in the rate of breathing affect the concentration of carbon dioxide in the blood?
How do the kidneys compensate for respiratory acidosis?
How do the kidneys compensate for respiratory acidosis?
What acid-base imbalance is likely to result from impaired kidney function?
What acid-base imbalance is likely to result from impaired kidney function?
What role does the excretion of ammonium (NH4+) play in acid-base balance?
What role does the excretion of ammonium (NH4+) play in acid-base balance?
If the ratio of [A-]/[HA] is equal to 1 in a buffer solution, how does the pH relate to the pKa of the weak acid?
If the ratio of [A-]/[HA] is equal to 1 in a buffer solution, how does the pH relate to the pKa of the weak acid?
Why can't we directly measure [H2CO3] and, instead, express it in terms of pCO2?
Why can't we directly measure [H2CO3] and, instead, express it in terms of pCO2?
Flashcards
What is pH?
What is pH?
The negative log of hydrogen ion concentration; indicates acidity or alkalinity of a solution.
What is a buffer?
What is a buffer?
A solution that resists changes in pH by neutralizing small amounts of added acid or base.
How do buffers work?
How do buffers work?
Weak acids and bases resist pH changes by neutralizing added acids or bases in a solution.
What is buffer capacity?
What is buffer capacity?
Signup and view all the flashcards
Optimal buffering range
Optimal buffering range
Signup and view all the flashcards
Why maintain blood pH?
Why maintain blood pH?
Signup and view all the flashcards
Bicarbonate buffer system
Bicarbonate buffer system
Signup and view all the flashcards
Components of bicarbonate buffer system
Components of bicarbonate buffer system
Signup and view all the flashcards
Respiratory control of pH
Respiratory control of pH
Signup and view all the flashcards
Kidney's role in pH
Kidney's role in pH
Signup and view all the flashcards
What is acidosis?
What is acidosis?
Signup and view all the flashcards
What is alkalosis?
What is alkalosis?
Signup and view all the flashcards
Alkaline reserve
Alkaline reserve
Signup and view all the flashcards
Key blood buffer
Key blood buffer
Signup and view all the flashcards
Compensatory mechanisms
Compensatory mechanisms
Signup and view all the flashcards
Mechanism of Buffers
Mechanism of Buffers
Signup and view all the flashcards
Henderson-Hasselbalch Equation
Henderson-Hasselbalch Equation
Signup and view all the flashcards
Buffer Capacity
Buffer Capacity
Signup and view all the flashcards
CO2 + H2O
CO2 + H2O
Signup and view all the flashcards
Bicarbonate transport
Bicarbonate transport
Signup and view all the flashcards
Buffering capacity
Buffering capacity
Signup and view all the flashcards
What do the kidneys replenish?
What do the kidneys replenish?
Signup and view all the flashcards
Study Notes
Lecture Learning Outcomes
- Buffer systems maintain pH stability in biological and chemical systems
- The Henderson-Hasselbalch equation interprets acid/base equilibria
- The Henderson-Hasselbalch equation determines the ionisation state of weak acids and bases given the pKa and pH
- Buffer capacity is influenced by factors particularly in biological systems
- The bicarbonate buffer system maintains physiological pH balance.
- Acidosis and alkalosis intricacies beyond the scope of the session
Maintaining pH
- pH measures hydrogen ion concentration (pH = -log[H+]) on a log scale
- Neutral pH (pH=7) equates to 10-7 M of H+
- Small pH changes represent large [H+] changes due to the log scale
- Body compartments maintain 'normal' pH within tight limits
- 'Normal' pH varies across body compartments like arterial blood (7.41), venous blood (7.36), intracellular fluid (7.35), and urine (~6-8)
- Changes in intracellular fluid pH affect extracellular pH and vice versa
- Problems occur rapidly when pH moves outside the normal range
- Proteins and enzymes denature, which leads to metabolism malfunction
- Acidosis or alkalosis are life-threatening if untreated with a blood pH below 7.35
- The CNS malfunctions and coma may result in blood pH falling below 7.35
Buffers Explained
- A buffer is a mix of weak acid/base and its conjugate form
- Weak acid buffers are aqueous solutions of a weak acid (HA, e.g., acetic acid) and its conjugate base salt (e.g., NaA, sodium acetate)
- Equilibria have certain concentrations of HA and A-
- Changes in pH drive the system to counteract the change based on Le Chatelier's principle
- The Henderson-Hasselbalch equation restates the acid dissociation constant, Ka, in terms of pH
Buffer Action
- Weak acids in the body are generally organic, such as carboxylic acids or inorganic, such as phosphoric acid
- Buffers resist pH changes upon addition of H+ or OH-
- When pH equals pKa, [HA] equals [A-]
- Buffers function best within +/-1 pH unit from the pKa, with about 10-90% dissociation
Buffer Capacity
- Buffering ability relies on concentration
- When the weak acid (HA) and conjugate base (A-) are used up the ability to resist pH change exhausts
- Greater availability of A- and HA molecules reduces the impact of strong acid (H+) or strong base (OH-) addition on pH
- Body buffers determine ability to cope with acidity changes
- Kidneys supply bicarbonate (HCO3-) to the blood
- Bicarbonate mops up H+
- Metabolic acidosis can result from improperly functioning kidneys.
Need for Buffers
- Most biological processes are pH-dependent, with enzymes functioning in a narrow pH range
- Small pH changes drastically affect reaction rates and system integrity
- Normal metabolism constantly generates CO2 and H+, disturbing pH
- Buffers maintain a suitable physiological pH
Body Buffers
- Phosphate buffer is intracellular with H2PO4- ↔ HPO4- + H+, pKa = 6.86
- Bicarbonate buffer system is in extracellular fluid (ECF), red blood cells (RBC), and blood; it has reversible equilibria including dissolved CO2
- Proteins are found throughout the body, such as albumin in blood and haemoglobin
Body buffering
- The body uses chemical buffering to minimize changes in [H+], but it does not remove it
- Body buffering involves food intake, digestion, and absorption with normal net acid input of ~1mM/Kg body weight/day
- The body employs cell metabolism, respiratory response, and renal response with chemical buffering of sulphate and phosphate
- Chemical buffering contains Chloride while binding to bases and excreting urine.
Phosphate Buffer System
- The main intracellular buffer alongside proteins with about 6X higher concentrations in ICF compared to ECF
- At physiological pH, the dissociation of the 2nd H+ is relevant at a pKa of H2PO4- of 6.86
- Buffers work best between +/- 1 from the pKa and act as effective buffers at a pH ~ 7.4
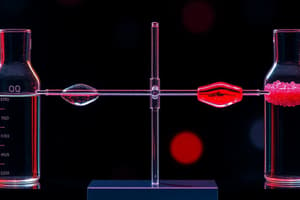
Bicarbonate System
- Key blood buffer is maintained at nearly constant pH (~pH 7.4; venous ~7.36)
- Also a key intracellular buffer in RBCs.
- Aids cell volume and fluid secretion maintainence and eliminates CO2 (major waste product).
- Consists of kidneys which excrete or retain H+ in the form of ammonia (NH4+) and lungs which exhale/inhale volatile acid (CO2)
- [CO2] can be rapidly adjusted by changes in rate of breathing with a large reservoir of CO2
- Bicarbonate (HCO3-) transport proteins provide pH inside and outside of RBCs
- Diseases like cystic fibrosis and heart disease may result due to disruption of this transport system
Bicarbonate Equilibria
- A drop in blood pH results in lactic acid production or exogenous salicylates
- Equilibria shifts towards production of CO2(g) increasing its exhalation
- Elevated NH3 levels cause reduction in cellular H+ resulting in blood pH rising
- Causes plasma [H+] to decrease,
- H2CO3 dissociates causing more CO2(g) in lungs to dissolve.
H-H Bicarbonate Equation
- Normal levels of bicarb [HCO3-] are ~24mM with a carbonic acid [H2CO3] of ~1.2mM
- [H2CO3] is expressed as pCO2 with dCO2 = 0.03 x pCO2
Respiratory vs. Metabolic Control
-
[H2CO3] is normally ~1mEq/L
-
CO2 released during respiration limits supply of H2CO3 with volatile acid (CO2) exhaled from lungs
-
[H2CO3] is under respiratory control
-
Respiratory function impairments cause acid/base imbalance
-
[HCO3-] is normally ~25mEq/L and closely regulated by kidneys
-
Kidneys are ultimate acid/base regulators and are acting slowly to compensate for disturbances arising from diet, metabolic, or disease
-
Body buffers temporarily tie up acids while the kidneys permanently excrete them
-
Metabolic (fixed) acids arise from incomplete metabolism (lactate, ketones) and proteins (sulfate)
Acid/Base Balance
- Concentration of buffering species determines the body’s buffering capacity
- Rate of acid/base production exceeding buffering species’ ability overwhelms the system
- In the bicarbonate buffer system, this is called the alkaline reserve (available HCO3-)
Acid Excretion
- Excess acid is transferred to NH3 (a weak base) in the kidney's proximal convoluted tubule (PCT) forming ammonium, NH4+
- Ammonium is very weak acid which stays protonated and is excreted in urine
- Simultaneously HCO3- is produced in the kidneys and transferred into the blood
- Kidneys replenish the HCO3- buffering capacity
- Respiratory/metabolic acid/base imbalances result from kidney or lung malfunction
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.