Podcast
Questions and Answers
What is the primary function of the periodontal ligament?
What is the primary function of the periodontal ligament?
- To facilitate the eruption of primary teeth
- To provide structural integrity to the tooth enamel
- To produce dental pulp
- To absorb and distribute occlusal forces (correct)
Which statement accurately describes the relationship of the periodontal ligament to the gum tissue?
Which statement accurately describes the relationship of the periodontal ligament to the gum tissue?
- The periodontal ligament acts as a barrier between the tooth and the gum tissue.
- The periodontal ligament originates solely from the gum tissue.
- The periodontal ligament is separated from the gum tissue by the alveolar bone.
- The periodontal ligament is continuous with the connective tissue of the gingiva. (correct)
How does the periodontal ligament communicate with the marrow spaces in the bone?
How does the periodontal ligament communicate with the marrow spaces in the bone?
- Through direct bone contact
- Through vascular channels (correct)
- Through inflammatory mediators
- Through neural connections
Where does the periodontal ligament merge at the root of the tooth?
Where does the periodontal ligament merge at the root of the tooth?
What role do the principal fibres of the periodontal ligament serve?
What role do the principal fibres of the periodontal ligament serve?
What primarily constitutes the fibers of the periodontal ligament?
What primarily constitutes the fibers of the periodontal ligament?
Which of the following statements about the blood supply to the periodontal ligament is correct?
Which of the following statements about the blood supply to the periodontal ligament is correct?
What type of nerves are predominant in the periodontal ligament?
What type of nerves are predominant in the periodontal ligament?
Where in the tooth is the periodontal ligament typically wider?
Where in the tooth is the periodontal ligament typically wider?
What characterizes the principal fibers of the periodontal ligament?
What characterizes the principal fibers of the periodontal ligament?
Which group is NOT one of the principal fiber groups of the periodontal ligament?
Which group is NOT one of the principal fiber groups of the periodontal ligament?
Which component is part of the extracellular matrix found in the periodontal ligament?
Which component is part of the extracellular matrix found in the periodontal ligament?
What role do Sharpey’s fibers play in the periodontal ligament?
What role do Sharpey’s fibers play in the periodontal ligament?
What is the average width of the periodontal ligament (PDL)?
What is the average width of the periodontal ligament (PDL)?
Under heavy loading conditions, what is the width of the PDL near the crest of the alveolus?
Under heavy loading conditions, what is the width of the PDL near the crest of the alveolus?
In which order do the fibers of the PDL develop as the crown erupts?
In which order do the fibers of the PDL develop as the crown erupts?
How does the appearance of the periodontal ligament differ in radiographs for permanent versus deciduous teeth?
How does the appearance of the periodontal ligament differ in radiographs for permanent versus deciduous teeth?
What happens to the organization of PDL fibers as development progresses?
What happens to the organization of PDL fibers as development progresses?
Which of the following describes the position of the first fibers that develop in the PDL?
Which of the following describes the position of the first fibers that develop in the PDL?
What is the relationship between Sharpey’s fibers and cementum during tooth eruption?
What is the relationship between Sharpey’s fibers and cementum during tooth eruption?
Which function is NOT associated with the periodontal ligament?
Which function is NOT associated with the periodontal ligament?
What is the primary function of the interradicular group fibres?
What is the primary function of the interradicular group fibres?
Where are the horizontal group fibres located?
Where are the horizontal group fibres located?
Which group of fibres is primarily responsible for resisting vertical masticatory forces?
Which group of fibres is primarily responsible for resisting vertical masticatory forces?
What occurs at the root tip regarding the apical group fibres?
What occurs at the root tip regarding the apical group fibres?
What do the interdental ligaments primarily connect?
What do the interdental ligaments primarily connect?
What significant change occurs in the periodontal ligament (PDL) with aging?
What significant change occurs in the periodontal ligament (PDL) with aging?
What role does the ground substance of the periodontal ligament play?
What role does the ground substance of the periodontal ligament play?
What is a significant characteristic of the interradicular group fibres?
What is a significant characteristic of the interradicular group fibres?
Which group of fibres primarily becomes significant during the translation of teeth?
Which group of fibres primarily becomes significant during the translation of teeth?
What happens to the fibrous structure of the periodontal ligament with age?
What happens to the fibrous structure of the periodontal ligament with age?
What is the location of the oblique group fibres within the periodontal ligament?
What is the location of the oblique group fibres within the periodontal ligament?
Which type of force do the horizontal group fibres primarily resist?
Which type of force do the horizontal group fibres primarily resist?
Which factor does NOT contribute to periodontal disease?
Which factor does NOT contribute to periodontal disease?
What is one of the significant functions of the alveolar crest group fibres?
What is one of the significant functions of the alveolar crest group fibres?
Flashcards are hidden until you start studying
Study Notes
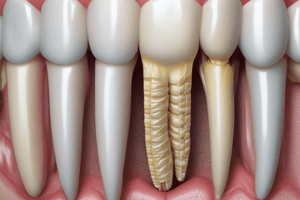
Periodontal Ligament (PDL) Definition and Function
- Connective tissue surrounding tooth roots and connecting them to the alveolar bone.
- Continuous with gingival connective tissue and communicates with bone marrow through vascular channels.
- Merges with dental pulp at the root apex.
PDL Functions
- Sensory: Perceives pressure, pain, and proprioception, crucial for mastication and speech.
- Nutritive: Provides nutrients to the cementum and periodontal tissues.
- Formative & Resorptive: Plays a critical role in tooth movement and remodelling, allowing adaptation to forces and orthodontic treatment.
- Physical: Supports the tooth in the alveolus, providing resistance to forces during chewing, speaking, and other functions.
PDL Width and Loading Conditions
- Average width: 0.2mm (range: 0.15mm to 0.38mm).
- Width varies based on loading conditions:
- Heavy Loaded: Around 0.35mm near the crest of the alveolus, 0.28mm in the middle, and 0.30mm near the fundus.
- Normally Loaded: Around 0.14mm near the crest, 0.10mm in the middle, and 0.12mm near the fundus.
- Functionless: Around 0.10mm near the crest, 0.06mm in the middle, and 0.06mm near the fundus.
PDL Radiograph Appearance
- Appears as a radiolucent area on radiographs, known as the periodontal space.
- Located between the radiopaque cementum and the lamina dura of the alveolar bone.
- Permanent teeth exhibit a narrower periodontal space compared to deciduous teeth.
PDL Development
- PDL originates from the dental follicle shortly after root development begins.
- Early fibers lack organization but develop an oblique orientation to the tooth.
- First fibers appear apical to the cemento-enamel junction (CEJ), giving rise to gingivodental fibers.
- As eruption progresses, more fibers develop and attach to new cementum and bone.
PDL Components
-
Cells:
- Synthetic: Fibroblasts (major component), cementoblasts, and osteoblasts.
- Resorptive: Osteoclasts and cementoclasts.
- Progenitor: Undifferentiated cells capable of differentiating into either synthetic or resorptive cells.
- Defence: Macrophages and lymphocytes.
- Epithelial Rests of Malassez: Remnants of the epithelial root sheath.
-
Extracellular Substance:
- Fibers: Collagen fibers constitute the primary component of the PDL and contribute to its strength and resilience.
- Ground Substance: Provides a medium for the diffusion of nutrients and waste, and aids in maintaining PDL structure.
Blood Supply to PDL
- Primarily supplied by the superior and inferior alveolar arteries.
- Blood vessels enter from various sources:
- Apical Vessels: Enter the PDL through the root apex.
- Penetrating Vessels: Originate from the alveolar bone and enter the PDL.
- Anastomosing Vessels: Connect with vessels from the gingiva.
- Blood vessels form extensive networks within the interstitial spaces.
Nerve Supply to PDL
- Two types of nerves:
- Sensory: Provide innervation for pain, pressure, and proprioception.
- Autonomic: Regulate blood flow and glandular secretions.
- Nerves originate from branches of the second and third divisions of the fifth cranial nerve (trigeminal nerve).
Principal PDL Fibers
- Made of collagen and organized into groups based on orientation and function.
- Purpose: Distribute masticatory and speech forces, providing support and stability to the tooth.
- Sharpey's Fibers: Embedded within the cementum and bone, anchoring the PDL fibers.
Principal PDL Fiber Groups
-
Alveolar Crest Group: Just beneath the junctional epithelium.
- Origin: Cementum below the CEJ.
- Insertion: Alveolar crest, running downwards and outwards.
- Significance: Prevents tooth extrusion and resists lateral, tilting, and intrusive forces.
-
Horizontal Group: Limited to the coronal fourth of the periodontal ligament.
- Origin: Cementum, apical to the alveolar crest group.
- Insertion: Alveolar bone apical to the alveolar crest, running perpendicular to the long axis.
- Significance: Resists horizontal and tipping forces.
-
Oblique Group: Occupies two-thirds of the length of the ligament.
- Origin: Cementum.
- Insertion: Alveolar bone, running obliquely in a coronal direction.
- Significance: Largest group, resistant to vertical masticatory forces, preventing tooth intrusion.
-
Apical Group: Located at the root tip.
- Origin: Cementum around the apex of the tooth.
- Insertion: Apex of the socket, fanning out irregularly.
- Significance: Not present in incompletely formed roots, resists vertical, luxative, and twisting forces, protects delicate nerves and vessels at the apex.
-
Interradicular Group: Found in multi-rooted teeth.
- Origin: Cementum.
- Insertion: Interradicular septum.
- Significance: Resists vertical and lateral movement, tipping, torquing, and luxation.
Interdental Ligament or Transseptal Fibers
- Span between neighboring teeth, extending through the gingival mucosa.
- Insert into cervical cementum of adjacent teeth over the alveolar crest.
- Cementum-to-cementum attachment, no bony involvement.
- Resist rotational forces and maintain tooth alignment.
Gingival Fiber Group
- Separate but adjacent fiber groups within the lamina propria of the marginal gingiva.
- Key component of gingival histology.
Ground Substance Composition and Functions
- Content:
- Collagen fibers.
- Water (approximately 70%).
- Tissue fluid pressure (slightly higher than atmospheric pressure).
- Functions:
- Facilitates the exchange of metabolites.
- Binds ions and water.
- Influences fiber orientation.
- Contributes to tooth support and binding mechanisms.
Age-Related Changes in PDL
- Decrease in cellularity, increase in fibrous tissue.
- Decline in vascularity and mitotic activity.
- Narrowing of the PDL width.
- Scalloping pattern observed on the calcified tissues (bone and cementum), with the PDL attached to the peaks of these scallops.
PDL Clinical Considerations
- Understanding PDL anatomy is crucial for:
- Diagnosis and treatment of periodontal diseases.
- Planning and executing orthodontic procedures.
- Implant placement and maintenance.
- Assessing tooth stability and predicting treatment outcomes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.