Podcast
Questions and Answers
Which of the following best describes anechoic echo patterns in ultrasound terminology?
Which of the following best describes anechoic echo patterns in ultrasound terminology?
- No internal echoes. (correct)
- Equal to surroundings.
- Less bright than surroundings.
- Bright echoes.
What is the patient preparation required for a transabdominal pelvic ultrasound?
What is the patient preparation required for a transabdominal pelvic ultrasound?
A full bladder, typically achieved by drinking 32 ounces of water.
What patient preparation is required for transvaginal ultrasound?
What patient preparation is required for transvaginal ultrasound?
An empty bladder.
What does T2P2A1L4 mean in TPAL format for reproductive history?
What does T2P2A1L4 mean in TPAL format for reproductive history?
The common iliac bifurcation occurs at the level of the...
The common iliac bifurcation occurs at the level of the...
Ureters are normally visible on ultrasound, even when not obstructed.
Ureters are normally visible on ultrasound, even when not obstructed.
What is the location of the bladder in the pelvis?
What is the location of the bladder in the pelvis?
The ______ is anterior to the internal iliac artery and posterior to the ovary.
The ______ is anterior to the internal iliac artery and posterior to the ovary.
Which one of these is a common reason for a pelvic ultrasound?
Which one of these is a common reason for a pelvic ultrasound?
What are the four layers of the bladder wall, from inner to outer?
What are the four layers of the bladder wall, from inner to outer?
What is the most common position of the uterus?
What is the most common position of the uterus?
What is the primary function of the zona functionalis?
What is the primary function of the zona functionalis?
During which phase of the menstrual cycle does the endometrium exhibit a trilaminar appearance?
During which phase of the menstrual cycle does the endometrium exhibit a trilaminar appearance?
What is the normal range for endometrial thickness in a postmenopausal woman?
What is the normal range for endometrial thickness in a postmenopausal woman?
What is the formula for volume calculation of the ovary?
What is the formula for volume calculation of the ovary?
Which one of these is the most helpful for imaging uterine malformations?
Which one of these is the most helpful for imaging uterine malformations?
The endometrium is atrophic after menopause
The endometrium is atrophic after menopause
What is another name for the uterine tubes?
What is another name for the uterine tubes?
List the structural layers of the fallopian tube, from outside to inside.
List the structural layers of the fallopian tube, from outside to inside.
What is the longest and most tortuous segment of the fallopian tube?
What is the longest and most tortuous segment of the fallopian tube?
What triggers ovulation?
What triggers ovulation?
During which endometrial phase is the functional layer shed?
During which endometrial phase is the functional layer shed?
Which of the following is a sonographic appearance of the proliferative phase?
Which of the following is a sonographic appearance of the proliferative phase?
Which structure produces progesterone after ovulation?
Which structure produces progesterone after ovulation?
The "three line sign" is associated with which endometrial phase?
The "three line sign" is associated with which endometrial phase?
In early pregnancy, hCG is produced by the:
In early pregnancy, hCG is produced by the:
What is the first evidence of an intrauterine pregnancy (IUP) on ultrasound?
What is the first evidence of an intrauterine pregnancy (IUP) on ultrasound?
The yolk sac is typically no longer visible by:
The yolk sac is typically no longer visible by:
At approximately what gestational age do the amnion and chorion normally fuse?
At approximately what gestational age do the amnion and chorion normally fuse?
The blastocyst typically implants at:
The blastocyst typically implants at:
When should the yolk sac be visible with transvaginal ultrasound?
When should the yolk sac be visible with transvaginal ultrasound?
What does an MSD greater than 7mm suggest?
What does an MSD greater than 7mm suggest?
What thermal index is most important for obstetric scanning?
What thermal index is most important for obstetric scanning?
During what weeks of gestation is the double decidual sac sign present?
During what weeks of gestation is the double decidual sac sign present?
What is the first structure inside the gestational sac?
What is the first structure inside the gestational sac?
The caudal end of the neural tube develops into what?
The caudal end of the neural tube develops into what?
When performing transabdominal pelvic scans, the patient should drink how much water?
When performing transabdominal pelvic scans, the patient should drink how much water?
What does T2P1A3L2 indicate?
What does T2P1A3L2 indicate?
When should the entry point of the transvaginal probe be oriented?
When should the entry point of the transvaginal probe be oriented?
In what phase is a homogenous endometrium typically seen?
In what phase is a homogenous endometrium typically seen?
The most common site of ectopic pregnancy is the...
The most common site of ectopic pregnancy is the...
The amniotic cavity should be visible on ultrasound when the MSD (Mean Sac Diameter) measures what?
The amniotic cavity should be visible on ultrasound when the MSD (Mean Sac Diameter) measures what?
What are the three vessels of the umbilical cord?
What are the three vessels of the umbilical cord?
What is oligohydramnios?
What is oligohydramnios?
Flashcards
Anechoic
Anechoic
No internal echoes; appears black.
Hyperechoic
Hyperechoic
Bright echoes.
Hypoechoic
Hypoechoic
Less bright than surrounding tissues.
Homogeneous
Homogeneous
Signup and view all the flashcards
Heterogeneous
Heterogeneous
Signup and view all the flashcards
Transabdominal Ultrasound Prep
Transabdominal Ultrasound Prep
Signup and view all the flashcards
Transvaginal Ultrasound Prep
Transvaginal Ultrasound Prep
Signup and view all the flashcards
TPAL
TPAL
Signup and view all the flashcards
Uterine Arteries
Uterine Arteries
Signup and view all the flashcards
Urinary Bladder Location
Urinary Bladder Location
Signup and view all the flashcards
Anterior Cul-de-sac
Anterior Cul-de-sac
Signup and view all the flashcards
Posterior Cul-de-sac
Posterior Cul-de-sac
Signup and view all the flashcards
Zona Functionalis
Zona Functionalis
Signup and view all the flashcards
Uterine Version
Uterine Version
Signup and view all the flashcards
Uterine Flexion
Uterine Flexion
Signup and view all the flashcards
Uterine Length Measurement
Uterine Length Measurement
Signup and view all the flashcards
Ovarian Blood Supply
Ovarian Blood Supply
Signup and view all the flashcards
Left Ovarian Vein
Left Ovarian Vein
Signup and view all the flashcards
Müllerian Duct
Müllerian Duct
Signup and view all the flashcards
Oviducts and Salpinges
Oviducts and Salpinges
Signup and view all the flashcards
Ampulla
Ampulla
Signup and view all the flashcards
Salpingitis
Salpingitis
Signup and view all the flashcards
Hydrosalpinx
Hydrosalpinx
Signup and view all the flashcards
GnRH
GnRH
Signup and view all the flashcards
Ampulla of Fallopian Tube
Ampulla of Fallopian Tube
Signup and view all the flashcards
Trophoblast
Trophoblast
Signup and view all the flashcards
Inner Cell Mass
Inner Cell Mass
Signup and view all the flashcards
Double Decidual Sac Sign
Double Decidual Sac Sign
Signup and view all the flashcards
Yolk Sac
Yolk Sac
Signup and view all the flashcards
Gestational Age
Gestational Age
Signup and view all the flashcards
Study Notes
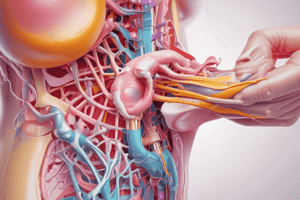
Pelvic Ultrasound: Basic Concepts and Anatomy
Basic Ultrasound Terminology
- Anechoic: Without internal echoes, appears black (e g., fluid, cysts, vessels, bladder)
- Hyperechoic: Displays bright echoes (e.g., bone, fat, air, ligaments, diaphragm)
- Hypoechoic: Less bright than surrounding tissues
- Isoechoic: Equal brightness to surrounding tissues
- Homogeneous: Refers to uniform texture
- Heterogeneous: Non-uniform texture
Scanning Fundamentals
- Sagittal Plane:
- Entry: Anterior or posterior.
- Visuals: Anterior, posterior, superior, and inferior aspects
- Transverse Plane:
- Entry: Multiple points.
- Visuals: Anterior, posterior, right lateral, and left lateral aspects
- Coronal Plane:
- Entry: Lateral.
- Visuals: Lateral, medial, superior, and inferior views
Patient Preparation and History
- Transabdominal Ultrasound: Requires a full bladder achieved with 32 ounces of water
- Transvaginal Ultrasound: Needs an empty bladder, verbal consent, and a chaperone if the examiner is male
- History: Review prior records (imaging reports, lab results, biopsies) and reproductive history using TPAL format (Term, Preterm, Abortion, Living children)
Pelvic Vascular Anatomy
Arterial Supply: - Major vessels: Begins with common iliac bifurcation at the superior margin of the sacrum, leading to external and internal iliac arteries - Uterine Blood Supply: Paired uterine arteries with a branching pattern including uterine (serosal), arcuate (myometrial), and radial (deep myometrial) arteries - Straight/basal arteries supply basal endometrial layer, and spiral arteries supply functional endometrial layer
- Venous Drainage: Mirrors arterial supply, drains to internal iliac veins, then IVC, except the left ovarian vein drains to the left renal vein
Pelvic Organs
Urinary System: - Bladder's location is in the anterior pelvis. Shape is pyramid when empty, dome when full. Wall layers are mucosa, submucosa, muscular, serosa. - Ureters route from kidney to bladder, anterior to internal iliac artery and posterior to ovary; not normally visible unless obstructed - Urethra: Muscular tube, bladder to genitals, for expelling urine
Clinical Considerations for Pelvic Ultrasound
- Common indications are pelvic pain and menstrual irregularities like dysmenorrhea, amenorrhea, menorrhagia, metrorrhagia; also infertility and postmenopausal bleeding
- Contraindications involve certain limitations
Technical Aspects
Infection Control: Transvaginal probe requires a sterile cover and proper disinfection with glutaraldehyde (20 min) or Trophon machine (7 min); never autoclave Documentation: Must include patient position, scanning approach, organ measurements, vascular assessment, and any pathological findings
Gynecologic Anatomy and Sonography
Pelvic Anatomy Overview
Anatomical Spaces: - Anterior cul-de-sac (uterovesical pouch): Between bladder and uterus - Posterior cul-de-sac (pouch of Douglas): Between rectum and uterus - Space of Retzius: Anterior to bladder and posterior to symphysis pubis Uterine Location: Posterior/inferior to the bladder and anterior to the rectum
Uterine Anatomy
Basic Structure: - Major Parts: Fundus (dome), body (corpus), isthmus, and cervix - Wall Layers: Endometrium (innermost), myometrium (middle), and perimetrium (outermost) Endometrial Characteristics: - Layers: Functional zone (sheds during menstruation) and basal zone (deep basal layer) - Sonographic Appearances: Vary with menstrual phase (thin, linear, echogenic, under 4 mm), periovulatory (trilaminar, 10-16 mm), and secretory (homogeneous, 16-18 mm) Uterine Positions: Version is cervix orientation to vagina, flexion is body orientation to cervix
Normal Measurements
Uterine Dimensions: - Adult Measurements: Length (6-9 cm), AP (2.5-3.5 cm), width (3-4 cm) - Changes in uterus size with respect to prepubertal or postmenopausal phase
Ovarian Anatomy
Basic Structure: - Dimensions: Maximum normal size is 3x2x2 cm; volume is calculated as L×W×H/2; reproductive age max is 6 cc - Anatomical Parts: Including germinal epithelium, tunica albuginea, cortex, medulla, follicles, and corpus luteum/albicans Blood Supply: Arterial (direct from aorta, ovarian branches of uterine arteries) and venous (right to IVC, left to left renal vein)
Sonographic Evaluation
Uterine Scanning - key views necessary Congenital Anomalies - mullerian duct development Clinical Applications: - Normal Variants: Postmenopausal changes include atrophic endometrium, tubular uterus, and equal cervix/body ratio
Gynecologic Anatomy and Physiology
Fallopian Tube Anatomy
- Alternative Names: Oviducts, salpinges (singular: salpinx), uterine tubes
- Dimensions: 7-14 cm Length, 1 - 4 mm Diameter
- Bilateral extension from cornua
Anatomical sections:
- Interstitial (Intramural): Located within uterine horn, the proximal portion.
- Isthmus: Located in the narrow portion, between the interstitial and ampulla.
- Longest/most tortuous segment : Ampulla, which is common site for fertilization and ectopic pregnancy.
- Infundibulum: Most distal section with funnel-shaped opening, connects to fimbriae.
- Fimbriae: Finger-like projections, helps to guide oocyte into the tube.
- Structural Layers (Outside to Inside): Serosal, muscularis, mucosal
Fallopian Tube Pathology
-
Condidtions: Salpingitis, Bacterial inflammation (STDs), causes infertility, symptoms range from none to pelvic pain. Fluid Collections:
-
Hydrosalpinx: Appears anechoic and tubular, comprised of Clear fluid .
-
Pyosalpinx: Shows internal echoes, comprised of Pus.
-
Hematosalpinx: Shows low-level echoes, comprised of Blood.
The Menstrual Cycle:
-
Cycles Involved: Ovarian cycle, uterine (endometrial) cycle, hormonal cycle.
-
Timing: 28 days - average duration , menses is 1-5 days, and day 14 for ovulation.
-
Hormonal Control:
- GnRH from Hypothalamus controls anterior pituitary
- FSH leads to Follicle development
- LH triggers ovulation
- Estrogen is driven by theca/granulosa cells, used in the first half of cycle, promotes endometrial thickening.
- Progesteroneis used the by corpus luteum, in the second half of cycle, maintains endometrial thickness.
Ovarian Cycle Phases:
- Characteristics of Follicular Phase (Days 1-14): Follicle development, estrogen production, ends with ovulation
- Follicle's Components: -Fluid-filled center, theca cells, oocyte, granulosa cells (sonographic marker)
- Phases of Ovulation:
- Triggered by LH surge, Graafian follicle rupture,release oocyte, possible mittelschmerz pain
Luteal Phase (Days 15-28)
development, corpus luteum formation, progesterone production, maintains endometrium. Outcomes
restart if no pregnancy: Corpus albicans,Progesterone decline cycle
The Endometrial Cycle
Three Phases:
- The functional layer is shed in the menstrual Phase.
- Sonographic Appearances driven During The proliferative Phase:
- Early : Thin, enchogenic
- Late: 3 line sign.
- Post ovulatory and Progesterone maintained during the secretory phase:
- Thick and uniformly echogenic.
Sonographic Considerations
- usually not visible and may see proximal segments on TV- Normal findings of fallopian tubes .
-
cysts > 3 cm, , Follicles < 3 cm-,Corpus luteum development-Ovarian Structures - Changes Throughout Cycle
- Early proliferative : Thin, echogenic -Endometrial Appearance: late proliferative is three-line sign , secretory is echogenicity with uniform thickness.
Clinical Applications
Important follicle sizing measurements :
-
Tube small < cm , Follicle sizes and cyst measurements> 3
-
enlarded -Tube pathology enlarged Abnormal Signs
-
cycle irregular and sign Abnormal fluid collections
-
abnormal endometrial Anovulation signs
Fetal Embryologic Development
Basic Cell Development and Reproduction
- Types of Cells
- Gametes (Haploid cells - 23 chromosomes)
- Female: Ova/oocytes
- Male: Spermatozoa (viable up to 72 hours)
- Human cells (Diploid - 46 chromosomes)
-23 from mother (22 + X)
-23 from father (22 + X or Y)
- Cell Division Processes:
- Meiosis: Creates gametes (23 chromosomes)
- Mitosis: Creates diploid cells (46 chromosomes)
Early Pregnancy Development
-
Timeline.
- Fertilization timeline of after 24-26 hours of post-ovulation. Implants - Location: Ampulla of fallopian tube at day 7,
- Early Developmental Stages :Single-cell starts from fertilized ovum zygote. Blastomere. 2-4 cell stages stages Morula mass of dividing cells. Blastocyst. Organised cell collection.
-
Pregnancy Dating
- Age Calculations: Conceptual Age that starts from conception. Gestational dating from LMP adds up to 2 weeks of developmental periods. Embryo and uterus Zygote. Conception till to implantation implantation(12 days.Embiryo till week 10.After week 10 into fetus
-
Trimester Division: - (1st trimester) 1-12 weeks, (2nd trimester) 13-26 weeks, (3rd trimester) 27-42 weeks.
Structures Of Early Pregnancy.
Blastocyst Components- Components:
Trophoblast - Key Structures: produces Hcg .Lining(outer layer of the Yolk sac . Becomes the inner mass(embryonic sack , Amnion.
- Decidual Development - develops within one week :Basalis implantation site, and then Capsularis surrounding the blastocyst which transforms into Verae uninvolved tissue.
- Pregnancy significance sonographically -Decidual formation, not so specific must check correlation between and age :Checkup must occur with HCG
Features Of Pregnancy
Production to assess early functions from placenta Detectable at day 23 of maintained detectable by day 23(menstrual age), maintains corpus, levels of around Normal 48 levels,peaks at 10, to 20 mmil
- Sonographic Correlation
Discriminatory (transvaginal and trans abdominal) :Transvaginal levels that measures between 12/18mm : Transabdominal : Possible detection with between 500mil Sonographic Finds During Early Pregnancy :First indication is gestational. :Forms in either mid shape in the uterus ,the growth rate :1mm by day Gestational Sac - Characteristics: Double Decidual sign that includes requires the yolk sac, required 8mm MSD
Extraembryonic Membranes Components
Amnion: Fluid-filled Protective sac . Yolk sac: Provides blood cell formation. Allantois Provides umbilical vessels through development
Specifics Of Yolk Sac
Detaches at around 8 weeks Becomes unviable :Disappears by 12 weeks-normal
- Normal size < 6mm Indicates - viability (90% accuracy)-.
- Note most indications
Placental Development
-
Formation Of Structure : -Components involved with basal maternal, and frondosum fetal structure -Provides energy -Functionalities :Oxygen transfer, nutrient ,waste Hormone- HCG
-
Includes
The spiral, endometrial veins, formation components of circulation (maternal).
-
Fevessels, developed Development vessels within the circulation
-
development Formation Layer:
- Endolining -Three Germs Digestive/ respiratory
- Mesoderm: muscles and bone
-
Ectoderm and neurological system Key formation from fetal of shape 10 weeks-Organ rudiments
Warnings For consideration
pregnancy of size from sac Gestational Characteristics
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.