Podcast
Questions and Answers
What is the functional significance of the oblique slit-like openings of the ureters into the bladder?
What is the functional significance of the oblique slit-like openings of the ureters into the bladder?
- They allow for independent control of urine flow from each kidney.
- They prevent reflux of urine back into the ureters during bladder contraction. (correct)
- They enhance the storage capacity of the bladder by allowing it to expand more easily.
- They facilitate the flow of urine into the bladder during periods of high intra-abdominal pressure.
Which statement accurately describes the position of the bladder in relation to other structures?
Which statement accurately describes the position of the bladder in relation to other structures?
- The urinary bladder is anterior to the uterovesical pouch and the anterior vaginal wall. (correct)
- The urinary bladder is posterior to the rectovesical pouch and seminal vesicles.
- The urinary bladder holds about 1500-2000 ml of urine
- When full, the urinary bladder is located in the pelvis.
A patient undergoing suprapubic catheterization experiences injury to the peritoneum. Which statement explains why this is most concerning?
A patient undergoing suprapubic catheterization experiences injury to the peritoneum. Which statement explains why this is most concerning?
- The peritoneum's role in supporting the bladder's superior surface is compromised.
- Peritoneal damage complicates subsequent imaging assessment of the urinary tract.
- Injury increases the risk of peritonitis due to the bladder's direct contact with the peritoneal cavity. (correct)
- The peritoneum restricts access to the bladder.
A surgeon is performing a procedure that requires access to the posterior surface of the anterior abdominal wall. Which ligament should they be aware of?
A surgeon is performing a procedure that requires access to the posterior surface of the anterior abdominal wall. Which ligament should they be aware of?
Surgical removal of the bladder neck poses a risk to the internal urethral sphincter in males. How would compromising the sympathetic innervation impact urinary function?
Surgical removal of the bladder neck poses a risk to the internal urethral sphincter in males. How would compromising the sympathetic innervation impact urinary function?
If the superior vesical artery is blocked due to atherosclerosis, which arteries could potentially provide collateral circulation to the anterosuperior part of the bladder?
If the superior vesical artery is blocked due to atherosclerosis, which arteries could potentially provide collateral circulation to the anterosuperior part of the bladder?
In bladder cancer staging, where would the lymphatics from the neck of the bladder primarily drain?
In bladder cancer staging, where would the lymphatics from the neck of the bladder primarily drain?
How do the structural differences in the male and female urethra affect susceptibility to urinary tract infections (UTIs)?
How do the structural differences in the male and female urethra affect susceptibility to urinary tract infections (UTIs)?
During a male bladder catheterization, resistance is met at a point along the urethra. What anatomical consideration explains the need to align the penis?
During a male bladder catheterization, resistance is met at a point along the urethra. What anatomical consideration explains the need to align the penis?
Considering the developmental origin of the testes, where would one expect the testicular artery to arise from?
Considering the developmental origin of the testes, where would one expect the testicular artery to arise from?
During a vasectomy a segment of the vas deferens is removed and the cut ends are ligated. What is being prevented by this procedure?
During a vasectomy a segment of the vas deferens is removed and the cut ends are ligated. What is being prevented by this procedure?
After a prostatectomy, a patient reports retrograde ejaculation. Which anatomical relationship explains this complication?
After a prostatectomy, a patient reports retrograde ejaculation. Which anatomical relationship explains this complication?
A patient is diagnosed with benign prostatic hypertrophy (BPH). What impact does the enlargement of the median lobe have on urinary function?
A patient is diagnosed with benign prostatic hypertrophy (BPH). What impact does the enlargement of the median lobe have on urinary function?
A patient is diagnosed with prostate cancer in the peripheral zone. Considering the anatomical arrangement, what is a likely outcome?
A patient is diagnosed with prostate cancer in the peripheral zone. Considering the anatomical arrangement, what is a likely outcome?
During an anatomical study, it is noted that a particular vein connects the pelvic venous plexus with the vertebral venous plexus. What is the significance of this venous pathway?
During an anatomical study, it is noted that a particular vein connects the pelvic venous plexus with the vertebral venous plexus. What is the significance of this venous pathway?
Which scenario exemplifies the autonomic control over the urinary bladder?
Which scenario exemplifies the autonomic control over the urinary bladder?
Why might a clinician intentionally avoid the use of 'all of the above' in multiple choice questions?
Why might a clinician intentionally avoid the use of 'all of the above' in multiple choice questions?
Why should options within a multiple-choice question be approximately similar in length?
Why should options within a multiple-choice question be approximately similar in length?
When constructing distractors for a multiple-choice question, why should you avoid directly using phrases from the reading material?
When constructing distractors for a multiple-choice question, why should you avoid directly using phrases from the reading material?
Why is including an 'info' section that references the content of a multiple-choice question considered poor practice?
Why is including an 'info' section that references the content of a multiple-choice question considered poor practice?
A subject is scheduled to undergo a TRUS biopsy. They ask what can be assessed by this method. What is the most accurate answer?
A subject is scheduled to undergo a TRUS biopsy. They ask what can be assessed by this method. What is the most accurate answer?
Following a bicycle accident involving trauma to the pelvic region, a male patient exhibits urinary incontinence, and further tests reveal damage to the levator ani muscles. What role do the levator ani muscles play in bladder support?
Following a bicycle accident involving trauma to the pelvic region, a male patient exhibits urinary incontinence, and further tests reveal damage to the levator ani muscles. What role do the levator ani muscles play in bladder support?
A patient with bladder cancer is being evaluated for potential metastasis through lymphatic drainage pathways. If cancer cells were found in the external iliac lymph nodes, what region of the bladder is most likely the primary site of the tumor?
A patient with bladder cancer is being evaluated for potential metastasis through lymphatic drainage pathways. If cancer cells were found in the external iliac lymph nodes, what region of the bladder is most likely the primary site of the tumor?
What is the expected outcome of bilateral damage to the hypogastric nerves following a surgical procedure in the pelvis?
What is the expected outcome of bilateral damage to the hypogastric nerves following a surgical procedure in the pelvis?
During a digital rectal examination, an enlarged posterior lobe is palpated. How does cancer in this location typically manifest?
During a digital rectal examination, an enlarged posterior lobe is palpated. How does cancer in this location typically manifest?
Which feature distinguishes transitional cell carcinoma (TCC) from other epithelial cancers in the urinary tract, particularly in terms of disease presentation?
Which feature distinguishes transitional cell carcinoma (TCC) from other epithelial cancers in the urinary tract, particularly in terms of disease presentation?
What is an important consideration regarding suprapubic catheterization?
What is an important consideration regarding suprapubic catheterization?
Concerning the male urethra, what accurately describes a segment of this tract?
Concerning the male urethra, what accurately describes a segment of this tract?
In the event of a traumatic injury that severs the inferior vesical artery in a male patient, what is the most likely outcome?
In the event of a traumatic injury that severs the inferior vesical artery in a male patient, what is the most likely outcome?
The detrusor muscle contracts when stimulated by the parasympathetic nervous system. Which scenario reflects the relationship between parasympathetic activation and urinary bladder function?
The detrusor muscle contracts when stimulated by the parasympathetic nervous system. Which scenario reflects the relationship between parasympathetic activation and urinary bladder function?
A patient is diagnosed with a tumor in the transitional epithelium of the bladder. What outcome is most likely?
A patient is diagnosed with a tumor in the transitional epithelium of the bladder. What outcome is most likely?
A male has developed vas deferens complications. What function is most likely to be compromised?
A male has developed vas deferens complications. What function is most likely to be compromised?
A urologist is planning a challenging catheterization. What aspect is known to make catheterization difficult?
A urologist is planning a challenging catheterization. What aspect is known to make catheterization difficult?
In what zone do prostatic tumors most commonly occur?
In what zone do prostatic tumors most commonly occur?
Anatomists classify the prostate into which sections?
Anatomists classify the prostate into which sections?
Which of the following best describes the position of the urinary bladder relative to other pelvic structures?
Which of the following best describes the position of the urinary bladder relative to other pelvic structures?
What is the typical range of urine volume that a healthy urinary bladder can hold?
What is the typical range of urine volume that a healthy urinary bladder can hold?
During suprapubic catheterization, it is important to consider the distension of the bladder. Why is this clinically relevant?
During suprapubic catheterization, it is important to consider the distension of the bladder. Why is this clinically relevant?
Which statement accurately describes the location of the apex of the urinary bladder?
Which statement accurately describes the location of the apex of the urinary bladder?
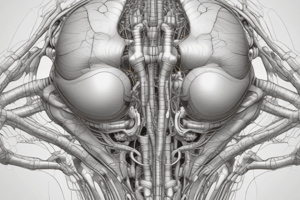
The base of the urinary bladder is characterized by which of the following?
The base of the urinary bladder is characterized by which of the following?
How does the arrangement of the ureters entering the bladder contribute to urinary function?
How does the arrangement of the ureters entering the bladder contribute to urinary function?
The inferolateral surfaces of the bladder are supported primarily by which structure?
The inferolateral surfaces of the bladder are supported primarily by which structure?
What is the clinical significance of the median umbilical ligament in relation to the urinary bladder?
What is the clinical significance of the median umbilical ligament in relation to the urinary bladder?
Which artery primarily supplies the anterosuperior portion of the bladder?
Which artery primarily supplies the anterosuperior portion of the bladder?
What is the primary blood supply to the base and neck of the bladder in males?
What is the primary blood supply to the base and neck of the bladder in males?
In females, which arteries replace the inferior vesical arteries in supplying the base and neck of the bladder?
In females, which arteries replace the inferior vesical arteries in supplying the base and neck of the bladder?
To which group of lymph nodes does the superior surface of the bladder primarily drain?
To which group of lymph nodes does the superior surface of the bladder primarily drain?
Where do the lymphatics from the inferior half of the bladder primarily drain?
Where do the lymphatics from the inferior half of the bladder primarily drain?
Which statement accurately describes the characteristics of the male urethra?
Which statement accurately describes the characteristics of the male urethra?
Why are ascending infections of the urinary bladder (cystitis) more common in women than in men?
Why are ascending infections of the urinary bladder (cystitis) more common in women than in men?
What anatomical adaptation is necessary when placing a bladder catheter in men that isn't as crucial in females, and why?
What anatomical adaptation is necessary when placing a bladder catheter in men that isn't as crucial in females, and why?
What is the primary function of the proteolytic enzymes secreted by the prostate gland?
What is the primary function of the proteolytic enzymes secreted by the prostate gland?
Which anatomical structure does the prostate gland directly surround?
Which anatomical structure does the prostate gland directly surround?
Considering its relationship to surrounding structures, which surface of the prostate is in direct contact with the levator ani muscles?
Considering its relationship to surrounding structures, which surface of the prostate is in direct contact with the levator ani muscles?
What is the anatomical location of the base of the prostate in relation to the urinary bladder?
What is the anatomical location of the base of the prostate in relation to the urinary bladder?
Where is the apex of the prostate located?
Where is the apex of the prostate located?
What structures converge at the seminal colliculus within the prostatic urethra?
What structures converge at the seminal colliculus within the prostatic urethra?
Which anatomical structure is located within the prostate gland and is a common site for benign prostatic hypertrophy (BPH)?
Which anatomical structure is located within the prostate gland and is a common site for benign prostatic hypertrophy (BPH)?
Which zone of the prostate is most commonly affected by prostatic tumors?
Which zone of the prostate is most commonly affected by prostatic tumors?
Which of the following is true regarding the function of the Batson venous plexus in the context of the prostate?
Which of the following is true regarding the function of the Batson venous plexus in the context of the prostate?
Which nerve fibers stimulate the detrusor muscle to contract, facilitating bladder emptying?
Which nerve fibers stimulate the detrusor muscle to contract, facilitating bladder emptying?
The sympathetic nervous system influences the function of the urinary bladder in which way?
The sympathetic nervous system influences the function of the urinary bladder in which way?
Compared to those in the male, what structural differences exist in the female urethra?
Compared to those in the male, what structural differences exist in the female urethra?
What is the action of the sympathetic nervous system on the internal urethral sphincter?
What is the action of the sympathetic nervous system on the internal urethral sphincter?
Contraction of the detrusor muscle is directly stimulated by which division of the autonomic nervous system?
Contraction of the detrusor muscle is directly stimulated by which division of the autonomic nervous system?
The testis originally develops in which location?
The testis originally develops in which location?
What is the function of the vas deferens?
What is the function of the vas deferens?
Which statement accurately describes the seminal vesicles?
Which statement accurately describes the seminal vesicles?
Which of the following accurately describes the duct of the seminal vesicle?
Which of the following accurately describes the duct of the seminal vesicle?
What is the purpose of a vasectomy?
What is the purpose of a vasectomy?
To which of the following arteries is the prostatic artery directly a branch?
To which of the following arteries is the prostatic artery directly a branch?
What is the significance of the rectovesical pouch regarding pelvic anatomy?
What is the significance of the rectovesical pouch regarding pelvic anatomy?
Flashcards
The bladder
The bladder
Most anterior element of the pelvic viscera.
Urinary bladder capacity
Urinary bladder capacity
Holds 150-600 ml of urine, pelvic when empty, abdominal when distended.
Apex of bladder
Apex of bladder
Directed towards the pubic symphysis.
Inferolateral bladder surface
Inferolateral bladder surface
Signup and view all the flashcards
Bladder's Mucosal lining
Bladder's Mucosal lining
Signup and view all the flashcards
Male bladder neck muscles
Male bladder neck muscles
Signup and view all the flashcards
Bladder cancer
Bladder cancer
Signup and view all the flashcards
Male Urethra
Male Urethra
Signup and view all the flashcards
Ejaculatory duct
Ejaculatory duct
Signup and view all the flashcards
Male bladder catheter
Male bladder catheter
Signup and view all the flashcards
The male reproductive system
The male reproductive system
Signup and view all the flashcards
Seminal vesicles function
Seminal vesicles function
Signup and view all the flashcards
Vas Deference
Vas Deference
Signup and view all the flashcards
Prostate Function
Prostate Function
Signup and view all the flashcards
Prostate Position
Prostate Position
Signup and view all the flashcards
Bulbourethral glands
Bulbourethral glands
Signup and view all the flashcards
Prostatic Anatomy
Prostatic Anatomy
Signup and view all the flashcards
Anterior lobe position
Anterior lobe position
Signup and view all the flashcards
Prostate lobes
Prostate lobes
Signup and view all the flashcards
Prostate Transitional Zone
Prostate Transitional Zone
Signup and view all the flashcards
Prostate cancer incidence
Prostate cancer incidence
Signup and view all the flashcards
Prostatic arteries blood supply
Prostatic arteries blood supply
Signup and view all the flashcards
Prostatic venous plexus
Prostatic venous plexus
Signup and view all the flashcards
Sympathetic role: bladder
Sympathetic role: bladder
Signup and view all the flashcards
Parasympathetic role: bladder
Parasympathetic role: bladder
Signup and view all the flashcards
Posterior division (Internal iliac)
Posterior division (Internal iliac)
Signup and view all the flashcards
Suprapubic Catheterization
Suprapubic Catheterization
Signup and view all the flashcards
Base of bladder
Base of bladder
Signup and view all the flashcards
Vasectomy
Vasectomy
Signup and view all the flashcards
Median Lobe position
Median Lobe position
Signup and view all the flashcards
Lateral prostate lobes
Lateral prostate lobes
Signup and view all the flashcards
Prostate Central Zone
Prostate Central Zone
Signup and view all the flashcards
Batson venous plexus
Batson venous plexus
Signup and view all the flashcards
Study Notes
Pelvic Content
- Pelvic viscera include parts of the gastrointestinal, urinary, and reproductive systems.
- The gastrointestinal system includes the rectum and anal canal.
- The urinary system includes terminal parts of the ureters, the bladder, and the proximal part of the urethra.
- Female reproductive systems include the uterus, uterine tubes, ovaries, and proximal vagina.
- Male reproductive systems include the vas deferens, seminal vesicles, prostate, and bulbourethral glands.
The Bladder
- Anterior to the rectovesical pouch and seminal vesicles in males.
- Anterior to the uterovesical pouch and the anterior vaginal wall in females.
- It is located in the pelvis when empty and can extend into the abdomen when full.
- It is the most anterior element of the pelvic viscera.
- The terminal parts of the ureters, the bladder itself, and the proximal part of the urethra are the pelvic parts of the urinary system
- The bladder holds about 150-600 ml of urine
- The apex is directed towards the pubic symphysis, with the median umbilical ligament continuing from the tip to the umbilicus.
- The base faces posterior-inferiorly.
- Two ureters enter at the top with oblique slit-like openings to prevent reflux, found at the lateral margins of the inter-ureteric crest.
- Contraction of the detrusor muscle creates a sphincteric effect.
- The urethra drains inferiorly.
- The mucosal lining is smooth and firmly attached to the underlying smooth muscle coat.
- Inferolateral surfaces are supported by the levator ani muscles.
- The superior surface is domed and covered with peritoneum.
Suprapubic Catheterization
- A small catheter is passed in the midline approximately 2 cm above the pubic symphysis to facilitate drainage.
Neck of the Bladder
- The most inferior part of the bladder is fixed.
- In males, detrusor muscles form the involuntary internal urethral sphincter.
- Sympathetic innervation constricts the internal urethral sphincter.
- The bladder supported by the perineal membrane, associated muscles, pubic bones, and tough ligaments.
- Females have pubovesical ligaments, and laxity can contribute to stress incontinence.
- Males have puboprostatic ligaments.
Vessels
- Anterosuperior parts are supplied by the superior vesical arteries.
- The base and neck are supplied by the inferior vesical arteries in males, replaced by the vaginal arteries in females.
- The obturator and inferior gluteal arteries also supply small branches to the bladder.
Lymphatics
- Lymphatics from the superior surface drain to the external iliac lymph nodes.
- Lymphatics from the inferior half drain to the internal iliac lymph nodes.
- Some lymphatics from the neck drain into the sacral (which drains then to internal iliac) or common iliac lymph nodes.
Bladder Cancer
- The most common tumor of the urinary tract.
- 1/3 are multifocal, and 2/3 are superficial and amenable to local treatment.
- Tumors can spread through the bladder wall and invade local structures and lymph nodes.
- Treatment depends on the severity: local resection, chemotherapy, or radical surgical removal of the bladder and prostate in men.
Urethra
- Male urethra is longer and bends twice.
- Pre-prostatic, internal urethral sphincter
- Prostatic, prostatic sinus, seminal colliculus
- Membranous, external urethral sphincter
- Spongy, corpus spongiosum, openings of the bulbourethral glands, bulbar and penile parts
Bladder Catheter
- Placement is easier in females.
- Ascending infections of the urinary bladder i.e cystitis more common in women than men because of shorter length of the female urethra
- Placement is more difficult in men because the urethra is longer and has angles that require a penis to be aligned.
- These angles must be compensated for by aligning the penis to prevent perforations.
- Prostatic tissue damage can cause pain and bleeding.
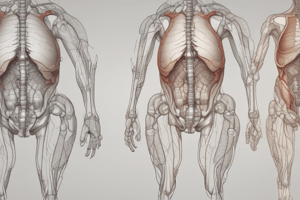
Male Reproductive System
- Major components include the testis, epididymis, ductus deferens, ejaculatory ducts, urethra, and penis.
- Accessory glands include a single prostate, a pair of seminal vesicles, and a pair of bulbourethral glands.
Testes
- The testes develop high on the posterior abdominal wall and then descend.
- Sperm made in the seminiferous tubules.
- They produce sperm and testosterone.
- Epididymis: stores newly formed sperms.
- The epididymis is located on the posterolateral sides of the testis.
Vas Deference and Seminal Vesicles
- Muscular duct which transports spermatozoa from the tail of the epididymis to the ejaculatory duct
- Accessory gland of the male reproductive system
- Part of the spermatic cord
- The secretions increase the volume of semen
- Blind-ended tubular outgrowth from vas deferens
- The duct joins vas deferens joining to form ejaculatory duct in the prostate gland.
Vasectomy
- A method of birth control that can be performed under local anaesthesia is a vasectomy.
- It involves removing a section of the vas (ductus) deferens.
- It involves ligating and/or cauterising the cut ends.
Prostate
- It secretes proteolytic enzymes into the semen for breaking down clotting factors in the ejaculate.
- It surrounds the urethra in the pelvic cavity
- Relationships: posterior to the pubic symphysis, anterior to the rectum, inferior to the urinary bladder.
- The apex of the prostate: along the superior fascia of the deep perineal pouch.
- The inferolateral surfaces: levator ani.
Prostate Anatomy
- Capsule
- Prostatic urethra
- Seminal colliculus
- Bulbourethral glands
Lobes of the Prostate:
- Anterior lobe is anterior to the urethra.
- Median lobe is posterior to the urethra, bounded inferiorly by the ejaculatory ducts, and enlarges into the base of the bladder in benign prostatic hypertrophy.
- Posterior lobe: posterior to the urethra, bounded superiorly by the ejaculatory ducts, can be felt in a digital rectal examination.
- Lateral lobes: right & left
Zones of the Prostate:
- Transitional zone surrounds the proximal and middle urethra.
- Benign prostatic hypertrophy occurs in the transition zone.
- The central zone is posterior to the prostatic urethra and forms the base of the prostate, containing the ejaculatory ducts.
- The peripheral zone surrounds the distal prostatic urethra at the apex and extends posterolaterally to the base, deficient anteriorly.
- About 70% of prostatic tumours occur in the peripheral zone.
Rectal Examination
- Prostate examined with digital rectal examination
- External anal sphincter
- Irregular/hard prostate means malignant
- Males: seminal vesicle, recto-vesical pouch
- Females: posterior wall of the vagina, cervix, rectouterine pouch
Benign Prostatic Hypertrophy (BPH)
- BPH is common in males.
- Clinical features result because they have been compressing prostatic part of the urethra resulting in obstructing urine overflow
- Muscular hypertrophy happens because there is high muscular pressure needed to push the fluids away out of the bladder
- Higher pressure lead to kidneys and ureters dilating which is hydronephrosis
Prostatic Cancer
- Common after the age of 65.
- People with early-stage are ASYMPTOMATIC
- Can happen in peripheral regions of prostate
- Feel prostate with digital exam
- If have ultrasound assess transrectal ultrasonography
Male Pelvic Fascia
-
Prostatic fascia dense fascia around the lateral of anterior regions and prostate
- Contains venous plexus
-
Rectovescial septum to separates surface of the bladder for of the rectum
-
Peritoneum surface continuous w pelvic inlet of the peritoneum
Blood Vessels-Prostate
- Artery: Prostatic arteries from inferior artery < internal iliac artery
Venous
- drainage drains prostate
- Batson veinsvalveless parallel that connect to deep pelvis
Autonomics to the Urinary Bladder
- Parasympathetic (pelvic splanchnic- S2-4):
- Pelvic splanchnic
- Motor bladder contracting
- Inhibitory to sphincter
- T12-L2 Sympathetic
- Contract sphincter
- innervate vessels
- Pain
- afferents follow sympathetics
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.