Podcast
Questions and Answers
What is the primary nerve supply to the cremaster muscle, crucial for the elevation of the testis?
What is the primary nerve supply to the cremaster muscle, crucial for the elevation of the testis?
- The pudendal nerve, known for its role in perineal sensation and motor function in the pelvic floor.
- The obturator nerve, which primarily serves the adductor muscles of the thigh.
- The ilioinguinal nerve, which also provides sensory innervation to the anterior scrotum.
- The genitofemoral nerve, specifically its genital branch. (correct)
Which of the following best describes the pathway visceral afferent fibers from the ureters take to relay pain sensations?
Which of the following best describes the pathway visceral afferent fibers from the ureters take to relay pain sensations?
- They travel retrogradely along sympathetic fibers to the spinal ganglia and cord segments T11-L5. (correct)
- They are carried by parasympathetic fibers to the sacral spinal cord segments S2-S4.
- They follow the pudendal nerve to the dorsal root ganglia of S2-S4.
- They ascend via the vagus nerve directly to the brainstem, bypassing the spinal cord.
In the context of testicular torsion, what vascular consequence is most likely to precipitate complete gangrene of the testicle?
In the context of testicular torsion, what vascular consequence is most likely to precipitate complete gangrene of the testicle?
- Compression of the spermatic cord leading to reduced venous outflow and subsequent arterial compromise. (correct)
- Increased arterial inflow due to inflammation.
- Thrombosis of the pampiniform plexus leading to acute varicocele formation.
- Primary arterial vasospasm without venous involvement.
What embryological process explains the presence of the tunica vaginalis as a covering of the testis?
What embryological process explains the presence of the tunica vaginalis as a covering of the testis?
Which anatomical structure directly contributes to the formation of the medial umbilical ligament on the posterior aspect of the anterior abdominal wall?
Which anatomical structure directly contributes to the formation of the medial umbilical ligament on the posterior aspect of the anterior abdominal wall?
Visceral afferent fibers from the uterus and superior part of the vagina transmit pain via which pathway?
Visceral afferent fibers from the uterus and superior part of the vagina transmit pain via which pathway?
A patient reports pain radiating from the flank to the groin. Which nerve pathway is most likely conducting this referred pain?
A patient reports pain radiating from the flank to the groin. Which nerve pathway is most likely conducting this referred pain?
What is the most critical structural difference between a direct and an indirect inguinal hernia?
What is the most critical structural difference between a direct and an indirect inguinal hernia?
Which of the following statements best describes the autonomic innervation responsible for male ejaculation?
Which of the following statements best describes the autonomic innervation responsible for male ejaculation?
If the pelvic splanchnic nerves are severed during a surgical procedure, which function would be most affected?
If the pelvic splanchnic nerves are severed during a surgical procedure, which function would be most affected?
During a hysterectomy, the uterine artery must be ligated. What other artery is most at risk of being inadvertently ligated at the same time?
During a hysterectomy, the uterine artery must be ligated. What other artery is most at risk of being inadvertently ligated at the same time?
A patient presents with a rectocele. Which fascial structure is most likely weakened?
A patient presents with a rectocele. Which fascial structure is most likely weakened?
Which anatomical feature predisposes males to a higher incidence of indirect inguinal hernias compared to females?
Which anatomical feature predisposes males to a higher incidence of indirect inguinal hernias compared to females?
What is the most likely consequence of injuring the perineal body during childbirth?
What is the most likely consequence of injuring the perineal body during childbirth?
Which structure in the female pelvis is analogous to the vas deferens in the male pelvis?
Which structure in the female pelvis is analogous to the vas deferens in the male pelvis?
What is the significance of the arcuate line of the pelvis?
What is the significance of the arcuate line of the pelvis?
What is the primary blood supply to the mid-ureter?
What is the primary blood supply to the mid-ureter?
What is the most accurate description of the location of the kidneys in relation to the peritoneum?
What is the most accurate description of the location of the kidneys in relation to the peritoneum?
What is the most likely consequence of complete compression of vasculature of the spermatic cord?
What is the most likely consequence of complete compression of vasculature of the spermatic cord?
Which nerve provides parasympathetic innervation to the bladder, facilitating detrusor muscle contraction for urination?
Which nerve provides parasympathetic innervation to the bladder, facilitating detrusor muscle contraction for urination?
What is the implication of lumbar spinal cord injury above the T12 level on male sexual function?
What is the implication of lumbar spinal cord injury above the T12 level on male sexual function?
What is the anatomical basis for referred pain experienced in testicular torsion?
What is the anatomical basis for referred pain experienced in testicular torsion?
What is the most significant risk associated with an ectopic pregnancy?
What is the most significant risk associated with an ectopic pregnancy?
How would a spinal block administered during childbirth (caudal epidural at S2-S4) impact nerve function?
How would a spinal block administered during childbirth (caudal epidural at S2-S4) impact nerve function?
In a male patient status post prostatectomy, what nerve damage would result in erectile dysfunction?
In a male patient status post prostatectomy, what nerve damage would result in erectile dysfunction?
What is a key difference between the male and female urethra?
What is a key difference between the male and female urethra?
Flashcards
Bony Pelvis
Bony Pelvis
The bony structure formed by the hip bones, sacrum, and coccyx.
Perineum
Perineum
The region of the body inferior to the pelvic diaphragm.
Scrotum
Scrotum
A cutaneous sac that contains the testes and associated structures.
Ureteropelvic Junction point
Ureteropelvic Junction point
Signup and view all the flashcards
Pelvic Inlet Crossing Point
Pelvic Inlet Crossing Point
Signup and view all the flashcards
Uterovesical Junction point
Uterovesical Junction point
Signup and view all the flashcards
Renal Capsule
Renal Capsule
Signup and view all the flashcards
Perinephric Fat
Perinephric Fat
Signup and view all the flashcards
Renal Fascia
Renal Fascia
Signup and view all the flashcards
Transversalis Fascia
Transversalis Fascia
Signup and view all the flashcards
Arcuate Line
Arcuate Line
Signup and view all the flashcards
Medial Umbilical Fold
Medial Umbilical Fold
Signup and view all the flashcards
Lateral Umbilical Fold
Lateral Umbilical Fold
Signup and view all the flashcards
Indirect Inguinal Hernia
Indirect Inguinal Hernia
Signup and view all the flashcards
Direct Inguinal Hernia
Direct Inguinal Hernia
Signup and view all the flashcards
Gubernaculum
Gubernaculum
Signup and view all the flashcards
Testicular Torsion
Testicular Torsion
Signup and view all the flashcards
Varicocele
Varicocele
Signup and view all the flashcards
Hydrocele
Hydrocele
Signup and view all the flashcards
Rectocele
Rectocele
Signup and view all the flashcards
Cystocele
Cystocele
Signup and view all the flashcards
Uterine Prolapse
Uterine Prolapse
Signup and view all the flashcards
Sacral Plexus
Sacral Plexus
Signup and view all the flashcards
Piriformis location for the Sacral Plexus
Piriformis location for the Sacral Plexus
Signup and view all the flashcards
Male Sympathetic Action
Male Sympathetic Action
Signup and view all the flashcards
Male Parasympathetic Action
Male Parasympathetic Action
Signup and view all the flashcards
Trigone of Bladder
Trigone of Bladder
Signup and view all the flashcards
Ectopic pregnancy
Ectopic pregnancy
Signup and view all the flashcards
Bloody Supply
Bloody Supply
Signup and view all the flashcards
Study Notes
Learning Outcomes
- By the end of this lecture, the anatomy of the bony pelvis, including the contrast between male and female features, should be understood.
- The surface anatomy and innervation of the perineum should be known.
- Understanding of the peritoneal reflections and recesses within the perineum is important.
- An understanding of how inguinal hernias develop, including their anatomy and clinical findings, is important.
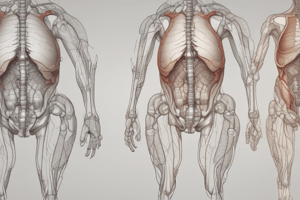
- Should be able to describe the layers of the scrotum, the testis and epididymis, and the effects of torsion.
Ureter
- Constriction areas are located at the junction of the ureters and renal pelves (ureteropelvic junction), where the ureters cross the brim of the pelvic inlet, and during their passage through the wall of the urinary bladder (Uterovesical junction).
- The blood supply to the ureter comes from branches of the renal, gonadal, common iliacs, and internal iliacs arteries, as well as branches from the aorta.
- The nerves to the abdominal part of the ureters derive from renal, abdominal aortic, and superior hypogastric plexuses.
- Visceral afferent fibers convey pain sensations retrograde to spinal ganglia and cord segments T11-L5.
- Referred pain may be felt in the small of the back, lumbar region (flank), and genitals, manifesting as loin to groin pain.
Anterior Abdominal Wall
- The arcuate line is a significant landmark on the posterior surface.
- The median umbilical ligament and medial umbilical ligament are key structures.
- The inferior epigastric artery and deep circumflex artery are important vascular components.
- The medial umbilical fold and lateral umbilical fold are also present on the posterior surface.
Hernias
- Indirect inguinal hernias are more common in men and babies and can be caused by a patent process vaginalis.
- In indirect inguinal hernias, the abdominal content passes through the deep ring, causing the bulge to occur lateral to the epigastric vessels.
- Direct inguinal hernias the abdominal content passes through a weakened posterior wall, causing the bulge to occur medial to the epigastric vessels which forms Hesselbach’s triangle.
- Direct inguinal hernias are more common in mature men and are often acquired through heavy lifting, constipation, or sports.
Descent of Testis
- Gubernaculum guides the testes through the inguinal canal to the scrotum.
- The gonads follow the gubernaculum.
- The spermatic cord also follows, and the gubernaculum degenerates after the descent is complete.
- Processus vaginalis, an evagination of the peritoneum, follows the course of the gubernaculum.
- It is anterior to both the gubernaculum and testes and usually obliterates, but a small part may persist as the tunica vaginalis.
Testicular Torsion
- Torsion, or twisting of the spermatic cord, results in compression of the vasculature.
- The most common predisposing factor is excessive mobility of the testis due to developmental anomalies.
- Torsion of the tiny vestigial appendix testis may cause acute pain in the scrotum, simulating acute epididymitis or mimicking acute appendicitis that manifests as referred pain.
Weakness in Pelvic Support
- Rectocele: Weakening of the tissue between the vagina and rectum (rectovaginal fascia) allows the rectum to protrude into the lower posterior vaginal wall.
- Cystocele: Descent in the anterior compartment causes the bladder to prolapse into the vagina.
- Uterine prolapse: Weakening of the uterus support (ligaments, perineal body, levator ani) causes the uterus to drop into the vagina.
Injury to Pelvic Floor
- The pelvic floor supports the fetal head during childbirth.
- The perineum, levator ani, and pelvic fascia may be injured during childbirth.
- These injuries may alter the position of the neck of the bladder and urethra and cause urinary stress incontinence.
Spermatic Cord
- Consists of three layers: internal spermatic fascia, cremasteric layer, and external spermatic fascia.
- It contains three arteries: testicular, cremasteric, and artery of vas.
- It consists of three nerves: nerve to cremaster, sympathetic, and ilioinguinal.
- Contains the vas deferens and pampiniform plexus of veins, with lymphatics to para-aortic nodes at L2.
Sacral Plexus
- Formed by the anterior rami of S1-4 and the lumbosacral trunk.
- Located anterior to the piriformis muscle.
- Consists of several main branches which include: sciatic nerve (L4-S3).
- Other nerves include: Pudendal nerve (S2-4)
- Superior (L4-S1) and inferior (L5-S2) gluteal nerves, posterior cutaneous nerve of the thigh (S1-S3), and pelvic splanchnic nerves (S2-4), including preganglionic parasympathetic and visceral afferents.
Autonomics of Pelvis
- The autonomic nerves enter the pelvic by four main routes.
- Sacral sympathetic trunks mainly supply the lower limb and postsynaptic fibers.
- Peri-arterial plexuses supply the superior rectal, ovaries, and internal iliac arteries.
- Pelvic splanchnic nerves provide parasympathetic innervation to the pelvic and hindgut.
- The hypogastric plexuses are the most important sympathetic route.
Hypogastric Plexus
- The inferior hypogastric plexus contains sympathetic, parasympathetic, and visceral afferent fibers.
- Arises from the rectal, uterovaginal, prostatic, and vesical plexuses.
Female Reproductive Organs
- The ovaries and uterine tube receive innervation.
- Nerves descend via the ovarian plexus on top of arteries.
- Visceral afferents carry pain via sympathetic fibers to T11-L1 and reflexes via parasympathetics to S2-S4.
- The uterus and superior part of the vagina.
- Nerves from the uterovaginal nerve plexus carry sympathetic (T12-L2), parasympathetics (S2-4), and visceral afferents.
- Visceral afferents carrying pain from intraperitoneal structures go back with sympathetic fibers.
- The inferior quarter of the vagina is innervated by somatic-pudendal nerves.
Regional Blocks
- Pudendal block anesthetizes the S2-4 region and is somatic.
- A caudal block anesthetizes S2-4 and is both somatic and parasympathetic.
- Spinal block anesthetizes the somatic, parasympathetic, and sympathetic areas
Male Internal Genital Organs
- The nerves from the inferior hypogastric plexus carry sympathetic (T12-L2), parasympathetic (S2-4), and visceral afferent fibers.
- Sympathetic innervation (T12-L2) causes contraction of the internal urethral sphincter, stimulates rapid peristalsis of the ductus deferens, and contributes to contraction and secretion of the prostate and seminal vesicles, resulting in ejaculation.
- Parasympathetic innervation (S2-3) supplies the erectile tissue.
- Causes the prostatic plexuses to form cavernous nerves which innervate the erectile tissue of the penis and are responsible for erection.
Male and Female Urethra
- Males urethra is both long and bends twice.
- The male urethra has four regions: pre-prostatic, prostatic, membranous, and spongy.
- The membranous portion contains the external urethral sphincter.
- The spongy portion contains the corpus spongiosum and bulbourethral glands, with two parts: bulbar and penile.
- The female urethra is short and goes through the pelvic floor and perineum to open into the vestibule, and has para-urethral mucous glands.
Male Urethra
- The prostatic urethra contains the prostatic urethra, seminal colliculus. Has multiple openings
- The bulbourethral glands are also present.
Female Reproductive Organs
- Ectopic pregnancy happens when a blastocyst implants in the uterine tube which causes tubal rupture and severe hemorrhage that can be life-threatening.
- The ovarian artery supplies the ovary and uterine tubes, while the uterine artery anastomoses with branches from the ovarian and vaginal arteries.
- The vagina is supplied by the vaginal artery and internal pudendal artery.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.