Podcast
Questions and Answers
What is the nature of Ischmere Disease?
What is the nature of Ischmere Disease?
- Chronic condition with gradual onset
- Fast onset with a potential for early ventricular arrhythmia (correct)
- Is a non-cardiac related issue
- Consistent classification within the Vaughn-Williams system
Which option describes a key feature of accessory pathways?
Which option describes a key feature of accessory pathways?
- They are primarily responsible for systemic blood flow.
- They have no impact on heart rhythm.
- They contribute to abnormal impulse formation. (correct)
- They exclusively facilitate cellular metabolism.
Which of the following antiarrhythmic agents is mentioned as a common treatment?
Which of the following antiarrhythmic agents is mentioned as a common treatment?
- Dofetilide
- Flecanide propafenone (correct)
- Quinidine
- Atenolol
What is NOT a feature of ventricular arrhythmias associated with Ischmere Disease?
What is NOT a feature of ventricular arrhythmias associated with Ischmere Disease?
What does the Vaughn-Williams classification primarily address?
What does the Vaughn-Williams classification primarily address?
Which treatment option is typically NOT recommended for arrhythmias?
Which treatment option is typically NOT recommended for arrhythmias?
What is the role of epinephrine in cardiac arrest situations?
What is the role of epinephrine in cardiac arrest situations?
What is a potential risk associated with rapid ventricular depolarization?
What is a potential risk associated with rapid ventricular depolarization?
Which statement accurately reflects the prognosis of untreated arrhythmias?
Which statement accurately reflects the prognosis of untreated arrhythmias?
Which drug is classified as a Class I antiarrhythmic agent?
Which drug is classified as a Class I antiarrhythmic agent?
Flashcards
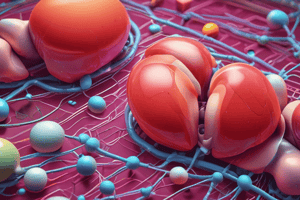
Ischemic Heart Disease (IHD)
Ischemic Heart Disease (IHD)
A condition caused by reduced blood flow to the heart muscle.
Ventricular Tachycardia
Ventricular Tachycardia
A rapid heartbeat originating in the lower chambers of the heart.
Accessory Pathways
Accessory Pathways
Abnormal electrical pathways in the heart that allow impulse transmission outside the normal conduction system.
Antiarrhythmic Agents
Antiarrhythmic Agents
Signup and view all the flashcards
Vaughn-Williams Classification
Vaughn-Williams Classification
Signup and view all the flashcards
Shockable Rhythms
Shockable Rhythms
Signup and view all the flashcards
Unshockable Rhythms
Unshockable Rhythms
Signup and view all the flashcards
CPR
CPR
Signup and view all the flashcards
Epi/Epinephrine
Epi/Epinephrine
Signup and view all the flashcards
Impulse Formation
Impulse Formation
Signup and view all the flashcards
Study Notes
Pathophysiology of Arrhythmias
- Abnormal Impulse Formation: Triggered activity or abnormal automaticity originating from the SA node or other sites.
- Abnormal Impulse Conduction:
- Re-entry (most common): Impulse travels backward through the conducting pathway.
- Block: Conducting pathway is blocked, preventing impulse transmission.
Classification of Arrhythmias
- Supraventricular Arrhythmias (Atrial Arrhythmias): Arrhythmias originating above the bundle of His.
- Sinus bradycardia
- Sinus tachycardia
- Atrial flutter
- Atrial fibrillation (AF)
- Paroxysmal supraventricular tachycardia
- Wolff-Parkinson-White (WPW) syndrome
- Premature atrial contractions (PACS)
- Ventricular Arrhythmias: Arrhythmias originating below the bundle of His.
- Premature ventricular contractions (PVCs)
- Ventricular tachycardia (VT)
- Ventricular fibrillation (VF)
Anti-Arrhythmic Agents
- Adenosine: Rapidly blocks the AV node, used for acute treatment of PSVT (pre-excitation supraventricular tachycardia) causing short-term chest heaviness or flushing.
- CCB (Calcium Channel Blockers): Alternative to adenosine if it's ineffective, administered as an IV bolus or infusion.
- Long-term management: Oral CCBs, beta-blockers, or digoxin may be used as alternatives. Radiofrequency catheter ablation could be used if pharmacological treatment proves insufficient.
Paroxysmal Supraventricular Tachycardia (PSVT)
- Definition: Sudden onset and termination of tachycardia (180-200 beats/min).
- Source: AV nodal re-entry.
- ECG Characteristics: Normal ECG with heart rate of 180-200 bpm.
- Causes: Electrolyte abnormalities, ischemic heart disease (IHD), cardiac surgery, thyrotoxicosis.
- Clinical Presentation: Palpitations, dizziness, presyncope (near-fainting).
- Complications: May degenerate to other serious arrhythmias. PSVT may not increase risk of stroke.
- Treatment: Vagal maneuvers (carotid massage, Valsalva maneuver), followed by drug therapy if those methods fail. Pharmacological treatment for acute episodes.
Wolff-Parkinson-White (WPW) Syndrome
- Definition: Pre-excitation syndrome where an impulse excites the ventricle before the expected regular impulse.
- Source: Accessory bypass tract connecting atria to ventricles.
- ECG Characteristics: Short PR interval, delta wave (fused complex) seen from pre-excitation
- Clinical Presentation: Atrial fibrillation, tachycardia, palpitations, lightheadedness, and fatigue.
- Treatment: Procainamide (FDA-approved for WPW) may be preferable to other anti-arrhythmic drugs; radiofrequency ablation is effective in the long term.
Drugs to Avoid in WPW
- Adenosine
- Beta-blockers
- Diltiazem
- Verapamil
- Digoxin
- Amiodarone
Ventricular Arrhythmias
- Definition: Arrhythmias originating below the bundle of His.
- Source: Irritable ectopic foci within the ventricular myocardium.
- ECG Characteristics: Wide, bizarre-looking QRS complexes.
- Clinical Forms:
- Premature ventricular contractions (PVCs)
- Ventricular tachycardia (VT)
- Ventricular flutter
- Ventricular fibrillation (VF)
- Torsades de Pointes (TdP)
Premature Ventricular Contraction (PVC)
- Definition: Extra heart beat arising from irritable ectopic foci of the ventricular myocardium.
- ECG characteristics: Wide and bizarre QRS complex.
- Clinical Presentation: Occasional/asymptomatic, symptomatic as PVCs in high frequency.
- Complication: High risk when it's frequent or in combination with structural heart disease (frequent PVCs, especially with reduced ejection fraction in patients to increase risk of sudden cardiac death).
- Treatment: If frequent, IV beta-blockers or CCBs may be used. Oral beta blockers or amiodarone are considered to prevent recurrence.
Nonsustained Ventricular Tachycardia (NSVT)
- Definition: Three or more consecutive PVCs lasting less than 30 seconds, self-terminating.
- ECG Characteristics: Three or more consecutive premature ventricular complexes(PVCs) lasting < 30 seconds, with or without symptoms.
- Clinical Presentation: Palpitations, lightheadedness.
- Complication: Risk of sudden cardiac death (SCD)
- Treatment: Varies based on the patient's ejection fraction and symptoms, usually no treatment needed if EF >40%
- IV beta blockers may be considered, if EF <40%.
Sustained Ventricular Tachycardia (SuVT)
- Definition: Three or more consecutive PVCs lasting more than 30 seconds.
- Source: Irritable ectopic foci that cause a sustained cardiac rhythm.
- ECG Characteristics: Three or more consecutive PVCs lasting >30 seconds, P-waves are lost in the QRS complex.
- Clinical Presentation: Pale, diaphoretic, lightheadedness, and may not respond to commands.
- Complication: Ventricular fibrillation, sudden cardiac death (SCD).
- Treatment: Hemodynamically stable patients may receive intravenous lidocaine/procainimide infusions; if these fail, other medications such as sotalol, and amiodarone may be used for long-term treatment.
Torsades de Pointes (TdP)
- Definition: Rapid polymorphic ventricular tachycardia that occurs at abnormal intervals with QT interval prolongation.
- ECG characteristics: Rapid, irregular QRS complexes and is identified in the presence of prolonged QT interval
- Clinical Presentation: Dizziness, consciousness if unstable
- Causes & Risk: Proarrhythmic drugs (class IA drugs except amiodarone and ibutilide), macrolide antibiotics.
- Complication: Ventricular fibrillation, sudden cardiac death (SCD)
- Treatment: Treatment if hemodynamically unstable includes electrical cardioversion and if hemodynamically stable magnesium as first-line measure and class IB antiarrhythmic agents as second-line measure.
Cardiac Conduction Blocks
- Supraventricular Blocks:
- First-degree AV block
- Second-degree AV block
- Third-degree AV block
- Ventricular Blocks:
- Right bundle branch block (RBBB)
- Left bundle branch block (LBBB)
Bradyarrhythmias
- Treatment (Symptomatic):
- Atropine injection (0.5-3 mg IV)
- Alternative treatments if unresponsive to atropine include transcutaneous pacing, dopamine infusion, epinephrine infusion, isoproterenol, transvenous pacing, and implantable pacemaker for refractory cases.
Implantable Cardioverter-Defibrillator (ICD)
- Overview: Implanted device under the skin with wires that detects and treats dangerous arrhythmias.
- Capabilities: Sensing, pacing, and defibrillation.
Cardiopulmonary Arrest
- Causes: Ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), pulseless electrical activity (PEA), asystole.
- Treatment: Cardiopulmonary resuscitation (CPR), drug therapy (epinephrine, amiodarone), defibrillation.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.