Podcast
Questions and Answers
The term ______ refers to an inflammation of the pancreas.
The term ______ refers to an inflammation of the pancreas.
Pancreatitis
What is the most common cause of pancreatitis?
What is the most common cause of pancreatitis?
- Gallstones
- Alcohol abuse (correct)
- Viral infections
- Autoimmune disorders
Acute pancreatitis resolves quickly, and the inflammation usually disappears after a short period of time.
Acute pancreatitis resolves quickly, and the inflammation usually disappears after a short period of time.
True (A)
Which of the following is NOT a symptom of chronic pancreatitis?
Which of the following is NOT a symptom of chronic pancreatitis?
What is the primary function of the endocrine pancreas?
What is the primary function of the endocrine pancreas?
Which of the following is NOT a role of the liver?
Which of the following is NOT a role of the liver?
Hepatitis is a viral infection that causes inflammation of the liver.
Hepatitis is a viral infection that causes inflammation of the liver.
Which type of hepatitis is most commonly spread through fecal-oral route?
Which type of hepatitis is most commonly spread through fecal-oral route?
What is the most common complication of liver cirrhosis?
What is the most common complication of liver cirrhosis?
Match the following types of bowel elimination with their primary location.
Match the following types of bowel elimination with their primary location.
The intestinal flora (microorganisms) play a significant role in the rate of bowel motility.
The intestinal flora (microorganisms) play a significant role in the rate of bowel motility.
What is the primary function of the kidneys?
What is the primary function of the kidneys?
The glomerular filtration rate (GFR) measures how quickly blood is filtered through the glomeruli in the kidneys.
The glomerular filtration rate (GFR) measures how quickly blood is filtered through the glomeruli in the kidneys.
The renin-angiotensin-aldosterone system (RAAS) is triggered by which of the following?
The renin-angiotensin-aldosterone system (RAAS) is triggered by which of the following?
The functional units of the kidneys are called ______.
The functional units of the kidneys are called ______.
Hydronephrosis is a condition where the bladder swells due to a buildup of urine.
Hydronephrosis is a condition where the bladder swells due to a buildup of urine.
Which of the following is NOT a symptom of kidney failure?
Which of the following is NOT a symptom of kidney failure?
What is the most common cause of urinary tract infections (UTIs)?
What is the most common cause of urinary tract infections (UTIs)?
Which of the following is NOT a factor that can increase the risk of UTIs?
Which of the following is NOT a factor that can increase the risk of UTIs?
Acute pyelonephritis is a sudden and severe infection of the kidneys.
Acute pyelonephritis is a sudden and severe infection of the kidneys.
What is the hallmark symptom of chronic renal failure?
What is the hallmark symptom of chronic renal failure?
What is the definition of a hormone?
What is the definition of a hormone?
Positive feedback amplifies a response, while negative feedback reduces or stabilizes it.
Positive feedback amplifies a response, while negative feedback reduces or stabilizes it.
Which of the following is considered a primary endocrine disorder?
Which of the following is considered a primary endocrine disorder?
What are the two most common causes of hyperfunction in endocrine disorders?
What are the two most common causes of hyperfunction in endocrine disorders?
Match the following hormones with their primary functions.
Match the following hormones with their primary functions.
The active form of thyroid hormone is T3.
The active form of thyroid hormone is T3.
Which of the following is NOT a symptom of hypothyroidism?
Which of the following is NOT a symptom of hypothyroidism?
What is the most common cause of primary hypothyroidism?
What is the most common cause of primary hypothyroidism?
Congenital hypothyroidism (cretinism) is a condition that is present at birth.
Congenital hypothyroidism (cretinism) is a condition that is present at birth.
Which of the following is a potential cause of hyperthyroidism?
Which of the following is a potential cause of hyperthyroidism?
Graves' disease is characterized by an underactive thyroid gland.
Graves' disease is characterized by an underactive thyroid gland.
What are the two main types of mineralocorticoids produced by the adrenal cortex?
What are the two main types of mineralocorticoids produced by the adrenal cortex?
Which of the following is NOT a symptom of Addison's disease (hypocortisolism)?
Which of the following is NOT a symptom of Addison's disease (hypocortisolism)?
Cushing's syndrome (hypercortisolism) is a condition caused by an overactive adrenal gland.
Cushing's syndrome (hypercortisolism) is a condition caused by an overactive adrenal gland.
What is the term for a specific type of fat deposition seen in Cushing's syndrome, often described as a 'buffalo hump'?
What is the term for a specific type of fat deposition seen in Cushing's syndrome, often described as a 'buffalo hump'?
Match the following pancreatic cell types with their primary hormone secretions.
Match the following pancreatic cell types with their primary hormone secretions.
The primary function of insulin is to ______ blood glucose levels.
The primary function of insulin is to ______ blood glucose levels.
Type 1 diabetes is primarily caused by a deficiency in insulin production.
Type 1 diabetes is primarily caused by a deficiency in insulin production.
Which of the following is MOST COMMON in type 2 diabetes?
Which of the following is MOST COMMON in type 2 diabetes?
What are the three main symptoms of diabetes?
What are the three main symptoms of diabetes?
Which diagnostic test is used to measure the average blood glucose levels over the past 2-3 months?
Which diagnostic test is used to measure the average blood glucose levels over the past 2-3 months?
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that can be life-threatening.
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that can be life-threatening.
Flashcards
Acute Gastritis
Acute Gastritis
Short-term stomach inflammation that resolves when the cause is removed.
Chronic Gastritis
Chronic Gastritis
Long-term stomach inflammation, can lead to ulcers and gastric cancer due to unrelenting injury or chronic infection, and autoimmunity.
Acute Pancreatitis
Acute Pancreatitis
Acute inflammation of the pancreas, leading to organ dysfunction and potential systemic failure.
Chronic Pancreatitis
Chronic Pancreatitis
Signup and view all the flashcards
Crohn's Disease
Crohn's Disease
Signup and view all the flashcards
Ulcerative Colitis
Ulcerative Colitis
Signup and view all the flashcards
Hepatitis
Hepatitis
Signup and view all the flashcards
Hepatitis A
Hepatitis A
Signup and view all the flashcards
Hepatitis B
Hepatitis B
Signup and view all the flashcards
Hepatitis C
Hepatitis C
Signup and view all the flashcards
Ascites
Ascites
Signup and view all the flashcards
Glomerular Filtration Rate (GFR)
Glomerular Filtration Rate (GFR)
Signup and view all the flashcards
Renin-Angiotensin-Aldosterone System (RAAS)
Renin-Angiotensin-Aldosterone System (RAAS)
Signup and view all the flashcards
Urolithiasis
Urolithiasis
Signup and view all the flashcards
Urinary Tract Infection (UTI)
Urinary Tract Infection (UTI)
Signup and view all the flashcards
Acute Pyelonephritis
Acute Pyelonephritis
Signup and view all the flashcards
Renal Failure
Renal Failure
Signup and view all the flashcards
Diabetes Mellitus Type 1
Diabetes Mellitus Type 1
Signup and view all the flashcards
Diabetes Mellitus Type 2
Diabetes Mellitus Type 2
Signup and view all the flashcards
Diabetic Ketoacidosis (DKA)
Diabetic Ketoacidosis (DKA)
Signup and view all the flashcards
Hypothyroidism
Hypothyroidism
Signup and view all the flashcards
Hyperthyroidism
Hyperthyroidism
Signup and view all the flashcards
Addison's Disease
Addison's Disease
Signup and view all the flashcards
Cushing's Disease
Cushing's Disease
Signup and view all the flashcards
Study Notes
Pathophysiology Exam #5 Master Document
- This document covers everything needed for the 5th Pathophysiology Exam.
- Content may be subject to change based on the released exam blueprint.
- The document's key is used to differentiate different levels of importance for the exam.
- Green: Big topic (similar to orange if a subtopic).
- Blue: Subtopic.
- Yellow: Vocabulary and important concepts within subtopics; helps separate ideas. Subtopics under yellow are now bigger than blue, but smaller than green.
- Orange: Same as yellow, but with more detailed content.
- Red: Specific examples; likely not all that important.
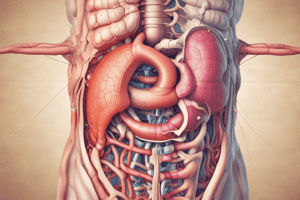
GI Disorders
- Inflammation:
- Gastritis: Stomach inflammation.
- Pancreatitis: Pancreas inflammation.
- Inflammatory Bowel Disease (Crohn's and Ulcerative Colitis): Chronic inflammation increases cancer risk. Tissue changes also increase cancer risk.
- Inflammation/Infection:
- Hepatitis: Viral liver inflammation.
- Stomach:
- Functions:
- Protection: Stomach acids destroy harmful substances. Prostaglandins protect the gastric mucosa. Gastric mucosa is highly vascular, dependent on blood flow for function. Alteration of blood flow causes gastritis.
- Digestion: Food and liquids mix with gastric secretions (mucus, acid, enzymes, hormones, intrinsic factor) in the stomach lining. Absorption mostly involves water and alcohol.
- Functions:
- Acute Gastritis: Inflammation of the stomach lining (gastric mucosa) that resolves when the cause is removed.
- Causes: Aspirin, alcohol, certain microorganisms.
Acute Pancreatitis
- Causes:
- Duct blockage by gallstones.
- Excessive alcohol use.
- Symptoms:
- Sudden upper abdominal pain, radiating to the back.
- Nausea, vomiting, anorexia, diarrhea.
- Patho:
- Injury triggers blockage of enzymatic pathways.
- Spills secretory enzymes → Inflammation .
- Response leads to increased vascular permeability, edema, hemorrhage, necrosis, granuloma formation, and abscess formation.
- Chronic Pancreatitis:
- Characterized by irreversible damage and tissue changes.
- Causes: Chronic alcohol use (most common), autoimmune disease, cystic fibrosis, and unknown causes.
Inflammatory Bowel Disease
- Chronic Inflammatory Processes:
- Can Occur Anywhere Along The GI Tract
- Most Commonly Of Small And Large Intestine
- MORE COMMON IN DEVELOPING COUNTRIES
- INCREASED RISK FOR PEOPLE IN COLDER CLIMATES AND URBAN AREAS.
- Small Intestine
- Digestion and Absorption:
- Primary Roles: Digestion and absorption through villi. Absorption happens in the intestinal mucosa. Processes include vitamin absorption, mineral absorption, fat absorption, carbohydrate absorption, protein absorption, water absorption, and electrolyte absorption (Na+ and K+).
- Large Intestine:
- Absorbs water and electrolytes (No villi).
Crohn's Disease
- Patchy Inflammation: Inflammation skips segments.
- Chronic Inflammation: Occurs in patchy segments (skip lesions).
- Increased Permeability: Inflammation begins in the mucosa and submucosa; increases permeability and vascularity leading to edema and fibrosis.
- Patho:
- Macrophages, plasma cells, and lymphocytes are released.
- Inflammation leads to granuloma formation.
- Location: Submucosal layers of the small intestine and ascending colon are the most common locations.
Ulcerative Colitis
- Non-Patchy Inflammation: Doesn't skip segments.
- Begins in the Rectum: Extends up the descending colon.
- Invades the Superficial Mucosa: Causes friability and causes bleeding.
Liver Disorders
- Liver Roles:
- Bile secretion involved in fat emulsification and absorption.
- Detoxification (removes toxins from the body).
- Bilirubin metabolism (breaks down red blood cells into heme and globin). Heme is then broken down into amino acids.
- Blood storage.
- Clotting factor synthesis.
- Nutrient metabolism
- Mineral and vitamin storage.
- LIVER IS ENCAPSULATED BY THE GLISSON CAPSULE.
Hepatitis (Viral)
- Transmission varies by type (fecal-oral or infected blood/body fluids).
- Incubation period and carrier states vary per type.
- Hepatitis A: Fecal-oral transmission, 1-2 months incubation period, no carrier state, and vaccine available.
- Hepatitis B: Contacted with infected blood , 2-3 months incubation period, carrier state possible, vaccine available.
- Hepatitis C: Contacted with infected blood, 2-3 months incubation period, carrier state possible, no vaccine.
- Hepatitis D: Contacted with infected blood, 2-3 months incubation period, carrier state possible, no vaccine.
- Hepatitis E: Fecal-oral transmission, 1-2 months incubation period, no carrier state, no vaccine.
Chronic Renal Failure
- Patho:
- Sodium and water balance is affected.
- Potassium balance is affected.
- There is an elimination of nitrogenous wastes.
- Erythropoietin production is affected.
- Acid-base balance issues occur.
- Activation and elimination of Vitamin D is affected.
- Phosphate elimination and hypocalcemia are potential complications.
- Possible complications result in skeletal issues, gastrointestinal disorders, neurologic issues, and sexual dysfunction.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.