Podcast
Questions and Answers
ما الفرق الرئيسي بين مرض كرون والتهاب القولون التقرحي؟
ما الفرق الرئيسي بين مرض كرون والتهاب القولون التقرحي؟
التهاب القولون التقرحي ينتشر بإمكانه أن يشمل القولون بأكمله ويكون شائعا في الجزء الأيسر دون منطقة يمكن تخطيها. من الناحية الأخرى، مرض كرون يشمل منطقة محددة في القولون، عادة في الجهة اليمنى من القولون. ويكون هناك مناطق متخطية في القولون.
قم بمطابقة ما يلي:
قم بمطابقة ما يلي:
التهاب شفاه (شیلیتس) = 1. Chelitis التهاب غشاء الفم (التهاب دماغ الفم) = 2. Stomatitis فشل البلع (صعوبة أو الم), = 3. Dysphagis الكرات اللمفية = 4. Lymphocytes القروح القلاعية = 5. Aphthous ulcers نوع B من التهاب المعدة المزمن = 6. Type B chronic gastritis بروستاغلاندين (PG) = 7. Prostaglandin ( PG) الاستخدام المطول للأسید اللاستروئيدی والأسبرین = 8. Prolong use of NSAIDs and aspirin قناة خلع الفتحة = 9. Type A gastritis الإلتھاب المتزمط الاتجاھي = 10. Glossitis حالة الميزية = 11. Measles كانديدا ألبیكانز = 12. Candida albicans الخلايا النيوتروفيلية = 13. Neutrophils عدم ارتیاح المريء = 14. Achalasia
Qual è la principale differenza tra la malattia di Crohn e la colite ulcerosa?
Qual è la principale differenza tra la malattia di Crohn e la colite ulcerosa?
Crohn's disease è regionale e può colpire specifiche parti del colon, mentre la colite ulcerosa è diffusa e coinvolge l'intero colon. La colite ulcerosa non causa perforazione (nessuna serosite), ma Crohn's disease può causare perforazione (serosite). Crohn's disease aumenta il rischio di cancro, mentre la colite ulcerosa ha infiltrato neutrofilici e secrezione mucopurulenta.
Abbina i seguenti termini alle corrispondenti descrizioni: (Scrivi il numero del termine accanto alla sua descrizione)
Abbina i seguenti termini alle corrispondenti descrizioni: (Scrivi il numero del termine accanto alla sua descrizione)
Fornisci una breve descrizione delle differenze tra la gastrite cronica di tipo A e di tipo B.
Fornisci una breve descrizione delle differenze tra la gastrite cronica di tipo A e di tipo B.
Flashcards are hidden until you start studying
Study Notes
###GIT Physiology
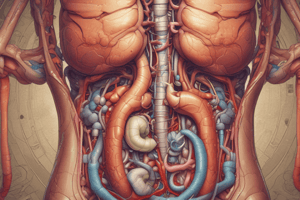
- GIT consists of Mouth, Esophagus, Stomach, Small intestine, and Large intestine (Cecum, Rectum, and Anus)*
###Inflammation of Lips (Chelitis)
- Types of Chelitis:
- Infective: caused by Virus (Herpes simplex), Bacteria (Staph and Syphilis), and Fungus (Candidia or Monilia)
- Non-infective: caused by Dribbling of saliva, Vitamin B and iron deficiency
###Stomatitis
- Definition: Inflammation of the mucous membrane of the mouth
- Types of Stomatitis:
-
- Aphthous ulcers (commonest)
- Self-limiting
- Rounded superficial erosions covered with a gray white exudate having an erythematous rim
- Less than 1 cm on the floor of the mouth and lateral border of the tongue
- Causes: stress, fever, certain foods, malnutrition, pregnancy, and Hormonal Imbalance
-
- Herpetic stomatitis
- Caused by HSV1, person-to-person transmission (kissing)
- Usually asymptomatic, but the virus will persist in ganglia (trigeminal ganglia) in a dormant state
- Reactivated in case of sun exposure, Respiratory tract infection, etc.
- Appearance of vesicles (5mm diameter) called cold sores or fever blister
-
- Candida albicans (Opportunistic infection)
- Normal flora (30-40%) of the population
- Oral candidiasis (thrush or moniliasis) common in Diabetes mellitus, anemia, antibiotic or cortisone, and immunodeficiency
- Common in children due to immature immunity
-
###Inflammation of Tongue (Glossitis)
- Acute glossitis: characterized by swollen papillae, occurs in eruptions of measles
- Chronic glossitis: the tongue is red without swollen papillae, seen in malnutrition
- Chronic atrophic glossitis: characterized by a smooth tongue
###Disorders of the Esophagus
- Swallowing disorders:
-
- Dysphagia: difficult or painful swallowing, results from narrowing of the esophagus, lack of salivary secretion, and weakness of the muscular structures
-
- Achalasia: failure to relax, the lower esophageal sphincter (LES) does not effectively allow food to pass through, may cause dilation above the LES
-
- Gastro-esophageal reflux (GER): persistent reflux of gastric content into the esophagus, due to incompetent esophageal sphincter, increase in pressure in the stomach, and common in children due to small capacity of the stomach
-
- Symptoms: heartburn, and complications include narrowing of the esophagus, and Barrett esophagus
###Stomach Disorders
-
- Acute gastritis: transient inflammation of the gastric mucosa, severe, nagging pain, and come in short bursts
-
- Chronic gastritis: long duration, and lymphocytes, plasma cells, macrophages
-
- Ulcerative disorders: peptic ulcer disease, and stress ulcers (physiologic stress like in illness)
-
- Cancer of the stomach
###Gastritis Symptoms
- Nausea, vomiting, indigestion, and feeling bloated
- Black stool due to bleeding
###Healthy Gastric Mucosa
- Intact mucosa, mucus production, blood flow to mucosa, and prostaglandin (stimulate secretion of mucous and bicarbonate to protect the stomach from acidic environment)
###Gastritis Pathogenesis
- Increase in acid secretion, decrease in adherent mucous layer, decrease in PGs secretion from the mucosa, and decrease in blood flow
###Causes of Acute Gastritis
- Infective: Salmonellosis, Staphylococcus (food poisoning)
- Non-infective: drugs (NSAIDs, cortisone), decrease in PGs, alcohol, smoking, shock, chemical irritant, and mechanical trauma
###Chronic Gastritis
- Types:
- Type A: Autoimmune gastritis, affect fundus, less than 10% of chronic gastritis
- Type B: Helicobacter pylori gastritis, antral gastritis, 90% of patients due to H. pylori
###Peptic Ulcer Disease (PUD)
- Presence of open sores or perforation in the area of the upper GIT (stomach and duodenum) that are exposed to acid
- Causes: H. pylori, long-term use of NSAIDs or aspirin
###Inflammatory Bowel Disease (IBD)
- Definition: chronic inflammation of the intestine
- Includes two disorders:
- Ulcerative bowel disease:
- Proctitis (rectum only)
- Left-side colitis
- Pancolitis (whole colon)
- Crohn's disease:
- Regional, takes certain region in the intestine
- Deep penetrating (serositis), and skip lesions
- Ulcerative bowel disease:
###Ulcerative Colitis (UC)
- Definition: chronic non-specific inflammation of the large intestine
- Causes: no specific cause, genetic predisposition, viral, and autoimmune
- Pathology: mucosa appears deeply congested associated with mucopurulent discharge and superficial irregular ulcers
- Symptoms: diarrhea, abdominal bleeding, and rectal bleeding
###Crohn's Disease
- Definition: regional enteritis, non-caseating granuloma of the alimentary tract
- Causes: no specific cause, genetic predisposition, virus or bacteria, and autoimmune
- Site: terminal ileum, right colon, but any part can be affected
- Have skip lesions, linear deep penetrating ulcers, and cobblestone appearance
###GIT Physiology
- GIT consists of Mouth, Esophagus, Stomach, Small intestine, and Large intestine (Cecum, Rectum, and Anus)*
###Inflammation of Lips (Chelitis)
- Types of Chelitis:
- Infective: caused by Virus (Herpes simplex), Bacteria (Staph and Syphilis), and Fungus (Candidia or Monilia)
- Non-infective: caused by Dribbling of saliva, Vitamin B and iron deficiency
###Stomatitis
- Definition: Inflammation of the mucous membrane of the mouth
- Types of Stomatitis:
-
- Aphthous ulcers (commonest)
- Self-limiting
- Rounded superficial erosions covered with a gray white exudate having an erythematous rim
- Less than 1 cm on the floor of the mouth and lateral border of the tongue
- Causes: stress, fever, certain foods, malnutrition, pregnancy, and Hormonal Imbalance
-
- Herpetic stomatitis
- Caused by HSV1, person-to-person transmission (kissing)
- Usually asymptomatic, but the virus will persist in ganglia (trigeminal ganglia) in a dormant state
- Reactivated in case of sun exposure, Respiratory tract infection, etc.
- Appearance of vesicles (5mm diameter) called cold sores or fever blister
-
- Candida albicans (Opportunistic infection)
- Normal flora (30-40%) of the population
- Oral candidiasis (thrush or moniliasis) common in Diabetes mellitus, anemia, antibiotic or cortisone, and immunodeficiency
- Common in children due to immature immunity
-
###Inflammation of Tongue (Glossitis)
- Acute glossitis: characterized by swollen papillae, occurs in eruptions of measles
- Chronic glossitis: the tongue is red without swollen papillae, seen in malnutrition
- Chronic atrophic glossitis: characterized by a smooth tongue
###Disorders of the Esophagus
- Swallowing disorders:
-
- Dysphagia: difficult or painful swallowing, results from narrowing of the esophagus, lack of salivary secretion, and weakness of the muscular structures
-
- Achalasia: failure to relax, the lower esophageal sphincter (LES) does not effectively allow food to pass through, may cause dilation above the LES
-
- Gastro-esophageal reflux (GER): persistent reflux of gastric content into the esophagus, due to incompetent esophageal sphincter, increase in pressure in the stomach, and common in children due to small capacity of the stomach
-
- Symptoms: heartburn, and complications include narrowing of the esophagus, and Barrett esophagus
###Stomach Disorders
-
- Acute gastritis: transient inflammation of the gastric mucosa, severe, nagging pain, and come in short bursts
-
- Chronic gastritis: long duration, and lymphocytes, plasma cells, macrophages
-
- Ulcerative disorders: peptic ulcer disease, and stress ulcers (physiologic stress like in illness)
-
- Cancer of the stomach
###Gastritis Symptoms
- Nausea, vomiting, indigestion, and feeling bloated
- Black stool due to bleeding
###Healthy Gastric Mucosa
- Intact mucosa, mucus production, blood flow to mucosa, and prostaglandin (stimulate secretion of mucous and bicarbonate to protect the stomach from acidic environment)
###Gastritis Pathogenesis
- Increase in acid secretion, decrease in adherent mucous layer, decrease in PGs secretion from the mucosa, and decrease in blood flow
###Causes of Acute Gastritis
- Infective: Salmonellosis, Staphylococcus (food poisoning)
- Non-infective: drugs (NSAIDs, cortisone), decrease in PGs, alcohol, smoking, shock, chemical irritant, and mechanical trauma
###Chronic Gastritis
- Types:
- Type A: Autoimmune gastritis, affect fundus, less than 10% of chronic gastritis
- Type B: Helicobacter pylori gastritis, antral gastritis, 90% of patients due to H. pylori
###Peptic Ulcer Disease (PUD)
- Presence of open sores or perforation in the area of the upper GIT (stomach and duodenum) that are exposed to acid
- Causes: H. pylori, long-term use of NSAIDs or aspirin
###Inflammatory Bowel Disease (IBD)
- Definition: chronic inflammation of the intestine
- Includes two disorders:
- Ulcerative bowel disease:
- Proctitis (rectum only)
- Left-side colitis
- Pancolitis (whole colon)
- Crohn's disease:
- Regional, takes certain region in the intestine
- Deep penetrating (serositis), and skip lesions
- Ulcerative bowel disease:
###Ulcerative Colitis (UC)
- Definition: chronic non-specific inflammation of the large intestine
- Causes: no specific cause, genetic predisposition, viral, and autoimmune
- Pathology: mucosa appears deeply congested associated with mucopurulent discharge and superficial irregular ulcers
- Symptoms: diarrhea, abdominal bleeding, and rectal bleeding
###Crohn's Disease
- Definition: regional enteritis, non-caseating granuloma of the alimentary tract
- Causes: no specific cause, genetic predisposition, virus or bacteria, and autoimmune
- Site: terminal ileum, right colon, but any part can be affected
- Have skip lesions, linear deep penetrating ulcers, and cobblestone appearance
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.