Podcast
Questions and Answers
A client with acute pancreatitis has a nasogastric tube to low intermittent suction, is NPO, and requires frequent oral care. What is the primary rationale for this nursing intervention?
A client with acute pancreatitis has a nasogastric tube to low intermittent suction, is NPO, and requires frequent oral care. What is the primary rationale for this nursing intervention?
- To stimulate saliva production and aid in digestion.
- To prevent aspiration pneumonia from excessive salivation.
- To minimize dryness and mucosal breakdown due to decreased oral intake. (correct)
- To provide comfort and prevent the transmission of oral bacteria to the GI tract.
The nurse is caring for a client with cholecystitis receiving conservative management. Which combination of interventions would best address the client's gallbladder inflammation and associated pain?
The nurse is caring for a client with cholecystitis receiving conservative management. Which combination of interventions would best address the client's gallbladder inflammation and associated pain?
- IV fluid administration, NPO status, analgesics for pain, a low-fat diet, and antibiotics if infection is suspected. (correct)
- Limiting fluid intake, administering NSAIDs, and providing a bland diet.
- Monitoring liver enzymes, providing a regular diet, and administering antipyretics.
- Encouraging a high-fat diet, administering antibiotics, and ambulating frequently.
A client with suspected common bile duct stones is undergoing intraoperative cholangiography. Which set of nursing actions is most important to ensure client safety and accurate results during and after the procedure?
A client with suspected common bile duct stones is undergoing intraoperative cholangiography. Which set of nursing actions is most important to ensure client safety and accurate results during and after the procedure?
- Obtaining baseline liver function tests, administering a cleansing enema, and monitoring for signs of infection post-procedure.
- Ensuring informed consent, monitoring for allergies to contrast dye, and documenting/labeling any removed stones. (correct)
- Preparing the surgical site, assessing for bleeding disorders, and encouraging deep breathing exercises post-procedure.
- Administering a pre-operative sedative, monitoring vital signs every 15 minutes, and restricting fluids post-procedure.
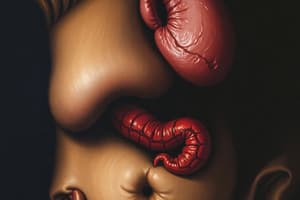
During assessment of a client experiencing an acute pancreatitis attack, the nurse observes a bluish discoloration around the umbilicus. How should the nurse document this finding?
During assessment of a client experiencing an acute pancreatitis attack, the nurse observes a bluish discoloration around the umbilicus. How should the nurse document this finding?
A 45-year-old patient with Type 2 Diabetes Mellitus is being educated on long-term complications. Which complications should the nurse prioritize in the teaching session?
A 45-year-old patient with Type 2 Diabetes Mellitus is being educated on long-term complications. Which complications should the nurse prioritize in the teaching session?
A patient with Type 1 Diabetes Mellitus presents with nausea, vomiting, abdominal pain, Kussmaul respirations, and a fruity odor on their breath. Which intervention is the nurse's priority?
A patient with Type 1 Diabetes Mellitus presents with nausea, vomiting, abdominal pain, Kussmaul respirations, and a fruity odor on their breath. Which intervention is the nurse's priority?
A 65-year-old patient with Type 2 Diabetes Mellitus is being treated for diabetic foot ulcers. Which statement by the patient indicates a need for further teaching regarding foot care?
A 65-year-old patient with Type 2 Diabetes Mellitus is being treated for diabetic foot ulcers. Which statement by the patient indicates a need for further teaching regarding foot care?
A patient with Type 1 Diabetes Mellitus is confused, diaphoretic, and has a blood glucose of 42 mg/dL. Which nursing action takes priority?
A patient with Type 1 Diabetes Mellitus is confused, diaphoretic, and has a blood glucose of 42 mg/dL. Which nursing action takes priority?
A newly diagnosed patient with Type 2 Diabetes Mellitus is asking the nurse about risk factors. Which factor is non-modifiable?
A newly diagnosed patient with Type 2 Diabetes Mellitus is asking the nurse about risk factors. Which factor is non-modifiable?
A patient with Type 2 Diabetes Mellitus is prescribed Metformin. Which teaching points are essential for the nurse to include?
A patient with Type 2 Diabetes Mellitus is prescribed Metformin. Which teaching points are essential for the nurse to include?
Flashcards
Why is oral care critical for a patient with acute pancreatitis?
Why is oral care critical for a patient with acute pancreatitis?
To reduce dryness and breakdown of the oral mucosa due to NPO status and the nasogastric tube.
What is Cullen's sign?
What is Cullen's sign?
A bluish discoloration around the umbilical area, indicating retroperitoneal bleeding.
What is Retinopathy?
What is Retinopathy?
Damage to the retina of the eyes, potentially leading to blindness.
What is Nephropathy?
What is Nephropathy?
Signup and view all the flashcards
What is Peripheral Neuropathy?
What is Peripheral Neuropathy?
Signup and view all the flashcards
What to do for low blood sugar?
What to do for low blood sugar?
Signup and view all the flashcards
Why prescribe ACE inhibitors for diabetes?
Why prescribe ACE inhibitors for diabetes?
Signup and view all the flashcards
Diabetes sick day rule?
Diabetes sick day rule?
Signup and view all the flashcards
Why annual dilated eye exams?
Why annual dilated eye exams?
Signup and view all the flashcards
Why rotate insulin injection sites?
Why rotate insulin injection sites?
Signup and view all the flashcards
Study Notes
- Oral care is critical for clients with acute pancreatitis, NPO status, and nasogastric tubes to low intermittent suction because it minimizes dryness and mucosal breakdown.
- Interventions for cholecystitis that can relieve gallbladder inflammation or pain include:
- IV fluid administration and bowel rest (NPO status)
- Administration of prescribed analgesics for pain control
- Encouraging a diet low in fat and avoiding spicy foods
- Use of antibiotics if infection is suspected
- Nursing responsibilities for intraoperative cholangiography include:
- Ensuring signed informed consent specifically for cholangiography
- Monitoring for allergic reaction to contrast dye
- Documenting and labeling any removed stones for pathology
- Cullen's sign during an acute pancreatitis attack presents as a bluish discoloration around the umbilical area.
- Long-term complications of diabetes to include in patient education are:
- Retinopathy
- Nephropathy
- Peripheral neuropathy
- Coronary artery disease
- Priority nursing intervention for a Type 1 diabetic patient with nausea, vomiting, abdominal pain, Kussmaul respirations, and fruity breath odor is to initiate IV fluids with normal saline.
- "I will soak my feet in warm water every night" suggests the need for further teaching for a Type 2 diabetic patient being treated for diabetic foot ulcers.
- The most appropriate nursing action for a confused, diaphoretic patient with Type 1 diabetes and a blood glucose of 42 mg/dL is to give 15g of fast-acting carbohydrates.
- Family history is not a modifiable risk factor for Type 2 Diabetes
- Teaching points for a Type 2 diabetic prescribed Metformin (Glucophage)
- "Take this medication with meals."
- "This medication may cause mild diarrhea at first."
- "Stop taking this medication if your blood sugar is above 200 mg/dL."
- Teaching points for a Type 1 diabetic learning about insulin therapy
- Rotate insulin injection sites to prevent lipodystrophy.
- Administer rapid-acting insulin 15 minutes before meals.
- Long-acting insulin should not be mixed with other insulins.
- Intervention during abdominal pain, vomiting, and deep rapid respirations associated with Type 1 DM
- Initiate IV normal saline infusion
- The immediate intervention for a Type 2 diabetic experiencing severe hypoglycemia (BG: 42 mg/dL) and unresponsiveness is to administer IM glucagon.
- A serum creatinine of 3.0 mg/dL requires immediate intervention for a Type 2 diabetic with CKD prescribed Metformin.
- Teach daily foot care and inspection for a Type 1 diabetic reporting numbness and tingling in both feet. Notes indicate: "I'm walking on pins and needles", loss of vibratory sensation, and diminished monofilament test results.
- During Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHS) with blood glucose of 750 mg/dL, serum osmolality of 340 mOsm/kg, negative ketones, and pH of 7.38, prioritize administering IV fluids rapidly.
- ACE inhibitors (Lisinopril) are prescribed to prevent diabetic nephropathy.
- Improve glycemic control in patients with diabetes experiencing delayed wound healing, elevated Hemoglobin A1c (10.2%), elevated white blood cell count (13,000/mm³), and blood glucose of 245 mg/dL.
- "I will continue taking my insulin even if I am not eating" is a correct statement for Type 1 diabetics learning about sick day management.
- The most important intervention for a diabetic at risk for retinopathy is annual dilated eye exams.
- Clarification is required if a newly diagnosed Type 1 diabetic is holding rapid-acting insulin for blood sugar < 100 mg/dL.
- For a Type 2 diabetic with Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHS), prioritize IV fluids.
- “If I'm vomiting, I will stop taking my insulin" indicates the need for further teaching for a Type 1 diabetic preparing for discharge after hospitalization for DKA.
- Administer IM glucagon for a Type 2 diabetic experiencing severe hypoglycemia (BG: 42 mg/dL) and unresponsiveness.
- Anticipate the administration of sodium bicarbonate for pH < 7.1 to a Type 1 diabetic with Kussmaul respirations, ketonuria, and altered mental status.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.