Podcast
Questions and Answers
Which of the following is NOT a risk factor for cholecystitis?
Which of the following is NOT a risk factor for cholecystitis?
- Low cholesterol levels (correct)
- Female gender
- Age
- Pregnancy
What is the primary cause of acute cholecystitis?
What is the primary cause of acute cholecystitis?
- Trauma to the gallbladder
- Bacterial infection
- Viral infection
- Obstruction of the cystic duct (correct)
Which of the following terms refers to inflammation of the common bile duct?
Which of the following terms refers to inflammation of the common bile duct?
- Cholangitis (correct)
- Cholecystitis
- Cholelithiasis
- Choledocholithiasis
What is the most common treatment for chronic cholecystitis?
What is the most common treatment for chronic cholecystitis?
Which of these hormones are known to stimulate gallbladder contraction and bile expulsion?
Which of these hormones are known to stimulate gallbladder contraction and bile expulsion?
What is the primary component of gallstones?
What is the primary component of gallstones?
What is the difference between cholelithiasis and cholecystitis?
What is the difference between cholelithiasis and cholecystitis?
Why does the presence of a stone in the cystic duct lead to inflammation?
Why does the presence of a stone in the cystic duct lead to inflammation?
Which of the following is NOT a risk factor for acute pancreatitis?
Which of the following is NOT a risk factor for acute pancreatitis?
What is the primary function of the pancreatic enzyme lipase?
What is the primary function of the pancreatic enzyme lipase?
Which of the following clinical manifestations is NOT typically associated with acute pancreatitis?
Which of the following clinical manifestations is NOT typically associated with acute pancreatitis?
What is the main mechanism by which acute pancreatitis develops?
What is the main mechanism by which acute pancreatitis develops?
Which of the following diagnostic tests is NOT typically used to evaluate acute pancreatitis?
Which of the following diagnostic tests is NOT typically used to evaluate acute pancreatitis?
What is the primary goal of intravenous fluid (IVF) administration in the management of acute pancreatitis?
What is the primary goal of intravenous fluid (IVF) administration in the management of acute pancreatitis?
Which of the following laboratory test results is typically ELEVATED in acute pancreatitis?
Which of the following laboratory test results is typically ELEVATED in acute pancreatitis?
What is the clinical significance of Cullen's sign in a patient with acute pancreatitis?
What is the clinical significance of Cullen's sign in a patient with acute pancreatitis?
What is a potential complication of chronic pancreatitis?
What is a potential complication of chronic pancreatitis?
Which of the following is NOT a typical symptom of chronic pancreatitis?
Which of the following is NOT a typical symptom of chronic pancreatitis?
What medical management strategy aims to reduce the amount of fatty stools in patients with chronic pancreatitis?
What medical management strategy aims to reduce the amount of fatty stools in patients with chronic pancreatitis?
When is surgery usually indicated for patients with chronic pancreatitis?
When is surgery usually indicated for patients with chronic pancreatitis?
What is the primary goal of nutritional therapy in patients with chronic pancreatitis?
What is the primary goal of nutritional therapy in patients with chronic pancreatitis?
What is the main benefit of pancreatic enzyme replacement therapy?
What is the main benefit of pancreatic enzyme replacement therapy?
What is the procedure called that involves placing a stent at the site of a pancreatic duct obstruction?
What is the procedure called that involves placing a stent at the site of a pancreatic duct obstruction?
Which of the following lifestyle modifications is NOT recommended for patients with chronic pancreatitis?
Which of the following lifestyle modifications is NOT recommended for patients with chronic pancreatitis?
Which diagnostic test would be most useful for determining the size of the gallbladder and presence of any masses?
Which diagnostic test would be most useful for determining the size of the gallbladder and presence of any masses?
What is the standard of treatment for cholecystitis?
What is the standard of treatment for cholecystitis?
In managing acute cholecystitis, what dietary restrictions are typically implemented?
In managing acute cholecystitis, what dietary restrictions are typically implemented?
What medication is commonly used to dissolve small gallstones and prevent new stone formation?
What medication is commonly used to dissolve small gallstones and prevent new stone formation?
Which of the following is NOT a potential complication of cholecystectomy?
Which of the following is NOT a potential complication of cholecystectomy?
What nursing intervention is crucial in post-operative cholecystectomy care to alleviate pain and promote comfort?
What nursing intervention is crucial in post-operative cholecystectomy care to alleviate pain and promote comfort?
What is the primary function of the pancreas?
What is the primary function of the pancreas?
Which diagnostic test uses visualization of the biliary tree to detect obstruction?
Which diagnostic test uses visualization of the biliary tree to detect obstruction?
What is the primary reason for avoiding high-fat foods in acute cholecystitis?
What is the primary reason for avoiding high-fat foods in acute cholecystitis?
Which of the following nursing interventions are crucial in post-operative care for a patient who has undergone cholecystectomy? (Select all that apply.)
Which of the following nursing interventions are crucial in post-operative care for a patient who has undergone cholecystectomy? (Select all that apply.)
What is the primary role of the liver in the breakdown and removal of old red blood cells (RBCs)?
What is the primary role of the liver in the breakdown and removal of old red blood cells (RBCs)?
Which of the following is NOT a characteristic of Hepatitis A?
Which of the following is NOT a characteristic of Hepatitis A?
What is the primary route of transmission for Hepatitis B?
What is the primary route of transmission for Hepatitis B?
Which hepatitis type typically causes the most chronic infections, leading to potential long-term liver complications?
Which hepatitis type typically causes the most chronic infections, leading to potential long-term liver complications?
What is the preferred treatment for Hepatitis A?
What is the preferred treatment for Hepatitis A?
Which of the following laboratory tests is NOT typically used for the diagnosis of Hepatitis?
Which of the following laboratory tests is NOT typically used for the diagnosis of Hepatitis?
Which of these is a potential complication of Hepatitis B or C?
Which of these is a potential complication of Hepatitis B or C?
Which of the following is NOT a sign or symptom of Hepatitis?
Which of the following is NOT a sign or symptom of Hepatitis?
What is the most effective way to prevent Hepatitis A?
What is the most effective way to prevent Hepatitis A?
Which of the following imaging tests is used for the diagnosis of Hepatitis?
Which of the following imaging tests is used for the diagnosis of Hepatitis?
What is a common symptom, that is associated with an increase in portal venous pressure?
What is a common symptom, that is associated with an increase in portal venous pressure?
Which of the following laboratory tests is NOT typically elevated in a patient with cirrhosis?
Which of the following laboratory tests is NOT typically elevated in a patient with cirrhosis?
Which of the following is a medical management intervention commonly used for ascites?
Which of the following is a medical management intervention commonly used for ascites?
Which of these is NOT a contributing factor to the development of Cirrhosis?
Which of these is NOT a contributing factor to the development of Cirrhosis?
What is the primary goal of the Transjugular Intrahepatic Portosystemic Shunt (TIPS) procedure?
What is the primary goal of the Transjugular Intrahepatic Portosystemic Shunt (TIPS) procedure?
What is the mechanism of action of Lactulose in the treatment of hepatic encephalopathy?
What is the mechanism of action of Lactulose in the treatment of hepatic encephalopathy?
Which of the following is a distinguishing characteristic of hepatic encephalopathy?
Which of the following is a distinguishing characteristic of hepatic encephalopathy?
Why are patients with cirrhosis advised to limit their intake of dietary protein?
Why are patients with cirrhosis advised to limit their intake of dietary protein?
What is the underlying reason for the development of splenomegaly in patients with cirrhosis?
What is the underlying reason for the development of splenomegaly in patients with cirrhosis?
What is the most likely explanation for the development of esophageal varices in a patient with cirrhosis?
What is the most likely explanation for the development of esophageal varices in a patient with cirrhosis?
Flashcards
Cholecystitis
Cholecystitis
Inflammation of the gallbladder often due to gallstones.
Cholelithiasis
Cholelithiasis
Presence of gallstones in the gallbladder.
Choledocholithiasis
Choledocholithiasis
Gallstones located in the common bile duct.
Cholangitis
Cholangitis
Signup and view all the flashcards
Acute Cholecystitis Pathophysiology
Acute Cholecystitis Pathophysiology
Signup and view all the flashcards
Chronic Cholecystitis Pathophysiology
Chronic Cholecystitis Pathophysiology
Signup and view all the flashcards
Risk Factors for Cholecystitis
Risk Factors for Cholecystitis
Signup and view all the flashcards
Gallbladder Function
Gallbladder Function
Signup and view all the flashcards
Ultrasonography
Ultrasonography
Signup and view all the flashcards
Magnetic resonance cholangiopancreatography (MRCP)
Magnetic resonance cholangiopancreatography (MRCP)
Signup and view all the flashcards
Endoscopic retrograde cholangiopancreatography (ERCP)
Endoscopic retrograde cholangiopancreatography (ERCP)
Signup and view all the flashcards
Cholecystectomy
Cholecystectomy
Signup and view all the flashcards
Intravenous fluids (IVF)
Intravenous fluids (IVF)
Signup and view all the flashcards
Analgesia
Analgesia
Signup and view all the flashcards
Post-Operative Care
Post-Operative Care
Signup and view all the flashcards
Nutritional Assessment
Nutritional Assessment
Signup and view all the flashcards
Potential Complications
Potential Complications
Signup and view all the flashcards
Exocrine Functions of Pancreas
Exocrine Functions of Pancreas
Signup and view all the flashcards
Endocrine Functions of Pancreas
Endocrine Functions of Pancreas
Signup and view all the flashcards
Trypsin
Trypsin
Signup and view all the flashcards
Amylase
Amylase
Signup and view all the flashcards
Lipase
Lipase
Signup and view all the flashcards
Acute Pancreatitis Symptoms
Acute Pancreatitis Symptoms
Signup and view all the flashcards
Cullen's Sign
Cullen's Sign
Signup and view all the flashcards
Diagnostics for Acute Pancreatitis
Diagnostics for Acute Pancreatitis
Signup and view all the flashcards
Parenteral Nutrition
Parenteral Nutrition
Signup and view all the flashcards
Chronic Pancreatitis
Chronic Pancreatitis
Signup and view all the flashcards
Digestive Problems in Chronic Pancreatitis
Digestive Problems in Chronic Pancreatitis
Signup and view all the flashcards
Glucose Control Issues
Glucose Control Issues
Signup and view all the flashcards
Signs of Biliary Obstruction
Signs of Biliary Obstruction
Signup and view all the flashcards
Pancreatic Enzyme Replacement
Pancreatic Enzyme Replacement
Signup and view all the flashcards
Nutritional Therapy for Pancreatitis
Nutritional Therapy for Pancreatitis
Signup and view all the flashcards
Surgical Options for Pancreatic Obstruction
Surgical Options for Pancreatic Obstruction
Signup and view all the flashcards
Cirrhosis
Cirrhosis
Signup and view all the flashcards
Portal Hypertension
Portal Hypertension
Signup and view all the flashcards
Ascites
Ascites
Signup and view all the flashcards
Esophageal Varices
Esophageal Varices
Signup and view all the flashcards
hepatic encephalopathy
hepatic encephalopathy
Signup and view all the flashcards
Asterixis
Asterixis
Signup and view all the flashcards
Caput Medusae
Caput Medusae
Signup and view all the flashcards
Lactulose
Lactulose
Signup and view all the flashcards
Transjugular Intrahepatic Portosystemic Shunt (TIPS)
Transjugular Intrahepatic Portosystemic Shunt (TIPS)
Signup and view all the flashcards
Diagnostic Tests for Cirrhosis
Diagnostic Tests for Cirrhosis
Signup and view all the flashcards
Bilirubin Fate
Bilirubin Fate
Signup and view all the flashcards
Jaundice
Jaundice
Signup and view all the flashcards
Hepatitis
Hepatitis
Signup and view all the flashcards
Hepatitis A
Hepatitis A
Signup and view all the flashcards
Hepatitis B
Hepatitis B
Signup and view all the flashcards
Hepatitis C
Hepatitis C
Signup and view all the flashcards
Symptoms of Hepatitis
Symptoms of Hepatitis
Signup and view all the flashcards
Hepatitis Diagnosis
Hepatitis Diagnosis
Signup and view all the flashcards
Preventing Hepatitis A and B
Preventing Hepatitis A and B
Signup and view all the flashcards
Complications of Hepatitis
Complications of Hepatitis
Signup and view all the flashcards
Study Notes
Nursing Management of Adults with Liver and Biliary Tract Disorders
- This course focuses on the nursing management of adults with disorders of the liver and biliary tract.
- Specific conditions like Cholelithiasis, Cholecystitis, Pancreatitis, Hepatitis, and Cirrhosis are used as examples.
- The objectives for the course include interpreting assessment data and diagnostic testing for liver and biliary tract conditions, developing comprehensive nursing care plans that include discharge plans, analyzing the impact of these disorders on physiological, psychological, and social domains, summarizing common drugs used for these conditions and their side effects, analyzing nursing research and ethical/legal considerations, and determining economic factors.
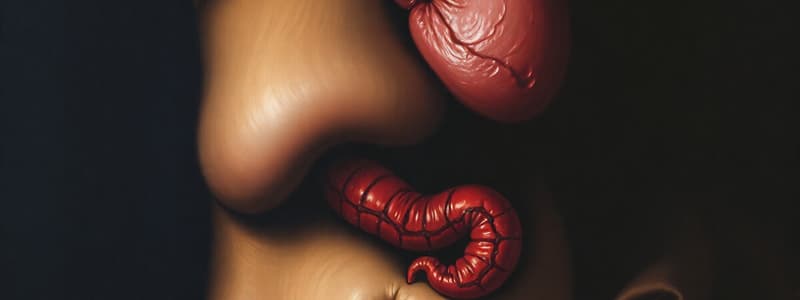
Anatomy Review
- Diagram of the liver, gallbladder, pancreas, cystic duct, common bile duct, pancreatic duct, and duodenum is provided in the anatomy review section.
- Illustrations help visualize the key locations and relationships of these organs.
The Gallbladder
- The gallbladder is a sac-like organ that stores and concentrates bile.
- Hormones from digestion stimulate the gallbladder to release bile.
- Gallstones are made of cholesterol, bilirubin, and calcium salts.
Cholecystitis
- Cholecystitis: Inflammation of the gallbladder
- Cholelithiasis: Gallstones in the gallbladder
- Choledocholithiasis: Gallstones in the common bile duct
- Cholangitis: Inflammation of the common bile duct
Acute Cholecystitis Pathophysiology
- Diffuse inflammation of the gallbladder.
- Usually due to obstruction of the cystic duct by gallstones.
- Inflammation develops behind the obstruction.
- Treatment involves removing the obstruction.
- May resolve spontaneously but can recur.
Chronic Cholecystitis Pathophysiology
- Repeated episodes of acute cholecystitis.
- Varying symptoms.
- Treatment typically involves cholecystectomy (gallbladder removal).
Cholecystitis Risk Factors & Assessment
- Women more frequently affected than men.
- Age as a risk factor.
- Pregnancy as a risk factor.
- Obesity.
- Stones vs No stones as underlying causes
Cholecystitis Diagnostic Tests
- X-rays can be used to rule out other causes but gallstones are rarely visible
- Ultrasound helps determine the size and presence of masses in abdominal organs.
- Magnetic Resonance Cholangiopancreatography (MRCP) visualises biliary tree and detects obstructions.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) visualises biliary & pancreatic structures via endoscopy.
- Cholecystogram and cholangiogram help visualize gallbladder and bile duct.
- Laparoscopy allows for visualization of liver, gallbladder, and surrounding structures.
Cholecystitis Medical Management
- Surgical procedures such as cholecystectomy are outlined as the standard of treatment.
- Collaboration is crucial with supportive measures such as rest, intravenous fluids, and nutritional support.
- Medications such as analgesics, antibiotics, and ursodeoxycholic acid may also be employed in treatment.
- Extracorporeal shock wave lithotripsy is also an option.
The Pancreas
- The pancreas has exocrine and endocrine functions.
- Exocrine functions involve producing digestive enzymes that are secreted into the small intestine (enzymes such as amylase, protease and Lipase).
- Endocrine functions involve releasing hormones into the bloodstream (such as insulin, glucagon, somatostatin, and pancreatic polypeptide).
Acute Pancreatitis Pathophysiology
- Pancreatic enzymes are activated within the pancreas itself causing autodigestion and inflammation.
- This can lead to damage and scarring in the pancreas
- Obstruction is a common cause, for example, by gallstones.
Acute Pancreatitis Risk Factors
- Gallstones
- Alcohol abuse
- Biliary tract disease
- Bacterial or viral infection
- Trauma
- Drug toxicities
- Smoking
Acute Pancreatitis Clinical Manifestations
- Severe abdominal pain (often radiating to the back)
- Nausea and vomiting
- Fever
- Hypotension
- Tachycardia
- Jaundice
- Decreased or absent bowel sounds
- Cullen's sign (bluish discoloration around the umbilicus)
- Grey Turner's sign (bluish discoloration along the flanks)
Acute Pancreatitis Diagnostic Tests
- X-rays (abdominal and chest)
- CT scans
- ERCP
- Ultrasound
- Laboratory tests (Serum amylase, Serum lipase, Blood glucose, WBC, Serum bilirubin, and Serum calcium).
Acute Pancreatitis Medical Management
- Pain management
- Correcting fluid and electrolyte imbalances
- Preventing or reducing pancreatic secretions
- Removing the precipitating cause (e.g., gallstones)
- Providing adequate nutritional support either enterally or parenterally
- Supportive measures of pain control, position, IV fluids and electrolytes.
Chronic Pancreatitis Pathophysiology
- Ongoing inflammation and fibrosis.
- Destruction of pancreatic cells.
- Possible strictures and calcifications
- Impairment in digestive function and absorption.
Chronic Pancreatitis Medical Treatment
- Medication administration (non-opioid analgesics, insulin therapy)
- Pancreatic enzyme replacement therapy
- Balanced nutrition and lifestyle support (NPO, low-fat/ bland diet, etc.)
- Surgery (e.g., choledochojejunostomy, Roux-en-Y) when other interventions fail.
The Liver
- The liver is a vital organ, performing numerous functions.
- Functions include metabolism of drugs, production of bile, storing minerals & vitamins, carbohydrate & fat metabolism, filtering of the blood, and metabolism of steroid hormones.
- Detailed diagrams show the liver's anatomy.
Portal Circulation
- Blood from the gastrointestinal tract, pancreas, and spleen flows into the liver.
- Total blood flow through the liver is considerable.
- Blood flows into the hepatic portal vein.
- From the liver it exits through the hepatic vein to the vena cava
Fate of Bilirubin
- Breakdown of old red blood cells (RBCs) produces bilirubin
- Bilirubin is transported by the liver, conjugated, and excreted into the bile (important for stool colour)
Jaundice
- High levels of unconjugated bilirubin in the blood leads to jaundice.
- Jaundice causes a yellowing of skin and eyes
Hepatitis
- Inflammation of the liver.
- Caused by toxins, bacteria, or viruses including Hepatitis A, B, C, D, and E.
- Diagnostics may include but are not limited to serum amylase, alanine transaminase, direct bilirubin and urine bilirubin.
Hepatitis Medical Management
- Rest, adequate nutrition, limited medication and supportive care for liver metabolism.
Cirrhosis
- Extensive, irreversible scarring of the liver.
- Often due to chronic liver damage from conditions like alcoholism, Hepatitis B & C, or autoimmune diseases.
Portal Hypertension
- Increased pressure in the portal venous system.
- Liver damage leads to poor circulation and can cause fluid to build up in the abdomen which is known as ascites.
- Portal hypertension can cause varices (enlarged veins) in the esophagus and other areas.
- Diagnosed through a variety of tests, such as imaging (e.g., ultrasound) and blood tests
Cirrhosis Clinical Manifestations
- Portal Hypertension, Ascites, Hepatic Encephalopathy, Esophageal Varices, and other symptoms
Liver Failure
- Complete liver failure results in an array of symptoms related to liver function impairment.
Liver Transplant
- Surgical procedures involve replacing the diseased liver with a healthy one.
- Potential donors can be either deceased or living.
- Immunosuppressive therapy is essential to prevent rejection.
Issues Related to Liver Transplantation
- Rigorous selection processes for suitable donors and recipients.
- Ethical considerations regarding organ allocation.
- Complications, such as bleeding, infection, and rejection, are potential risks.
Nursing Process, Interventions, and Education
- Nursing diagnoses, overall goals, and nursing interventions related to liver diseases are addressed.
- Patient education regarding different aspects of liver diseases and treatment are discussed
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.