Podcast
Questions and Answers
Which portion of the pancreas makes up 90% of the organ and is a major source of enzymes essential for digestion?
Which portion of the pancreas makes up 90% of the organ and is a major source of enzymes essential for digestion?
- Acinar cells
- Exocrine portion (correct)
- Islets of Langerhans
- Endocrine portion
What do Islets of Langerhans secrete?
What do Islets of Langerhans secrete?
- Digestive enzymes
- Insulin, glucagon, and somatostatin (correct)
- Antibodies
- Hormones for growth
What is the main clinical manifestation of pancreatitis?
What is the main clinical manifestation of pancreatitis?
- Mild self-limited disease
- Digestive disorders
- Life-threatening idiopathic acute inflammatory process
- Inflammation of the pancreas (correct)
Which disorders are most significant for the endocrine pancreas?
Which disorders are most significant for the endocrine pancreas?
Which portion of the pancreas secretes enzymes essential for digestion?
Which portion of the pancreas secretes enzymes essential for digestion?
What characterizes the severity range of pancreatitis?
What characterizes the severity range of pancreatitis?
What is the most common cause of chronic pancreatitis?
What is the most common cause of chronic pancreatitis?
Which mutations are associated with potential hereditary factors in idiopathic chronic pancreatitis?
Which mutations are associated with potential hereditary factors in idiopathic chronic pancreatitis?
What are the clinical features of chronic pancreatitis?
What are the clinical features of chronic pancreatitis?
What are the complications associated with chronic pancreatitis?
What are the complications associated with chronic pancreatitis?
What is the mortality rate over 20 to 25 years for those with chronic pancreatitis?
What is the mortality rate over 20 to 25 years for those with chronic pancreatitis?
What dietary recommendation should be given to patients with chronic pancreatitis?
What dietary recommendation should be given to patients with chronic pancreatitis?
Which of the following is a common cause of chronic pancreatitis?
Which of the following is a common cause of chronic pancreatitis?
What are the typical laboratory findings in acute pancreatitis?
What are the typical laboratory findings in acute pancreatitis?
What is the most likely diagnosis for a 60-year-old alcoholic man with recurrent epigastric pain, weight loss, and foul smelling diarrhea, and X-ray revealing multiple areas of calcification in the mid-abdomen?
What is the most likely diagnosis for a 60-year-old alcoholic man with recurrent epigastric pain, weight loss, and foul smelling diarrhea, and X-ray revealing multiple areas of calcification in the mid-abdomen?
What is the primary triggering event in acute pancreatitis?
What is the primary triggering event in acute pancreatitis?
What is a possible cause of acute hemorrhagic pancreatitis?
What is a possible cause of acute hemorrhagic pancreatitis?
Which of the following symptoms is not typically associated with chronic pancreatitis?
Which of the following symptoms is not typically associated with chronic pancreatitis?
Which of the following is a characteristic feature of fat necrosis in acute pancreatitis?
Which of the following is a characteristic feature of fat necrosis in acute pancreatitis?
What is the result of fat necrosis in acute pancreatitis?
What is the result of fat necrosis in acute pancreatitis?
Where can fat necrosis occur in acute pancreatitis?
Where can fat necrosis occur in acute pancreatitis?
What are the consequences of acute pancreatitis?
What are the consequences of acute pancreatitis?
What laboratory findings are associated with acute pancreatitis?
What laboratory findings are associated with acute pancreatitis?
What complications can arise from acute pancreatitis?
What complications can arise from acute pancreatitis?
Which condition is associated with irreversible loss of exocrine pancreatic parenchyma?
Which condition is associated with irreversible loss of exocrine pancreatic parenchyma?
What can lead to local fat necrosis in acute pancreatitis?
What can lead to local fat necrosis in acute pancreatitis?
What can cause primary acinar cell injury in acute pancreatitis?
What can cause primary acinar cell injury in acute pancreatitis?
What alterations are seen in acute pancreatitis histology?
What alterations are seen in acute pancreatitis histology?
What can contribute to the development of acute pancreatitis?
What can contribute to the development of acute pancreatitis?
What is the incidence rate of acute pancreatitis in Western countries?
What is the incidence rate of acute pancreatitis in Western countries?
Flashcards are hidden until you start studying
Study Notes
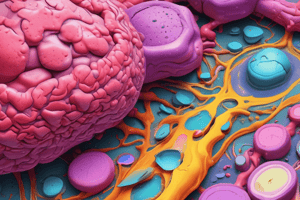
- Acute Pancreatitis: Reversible injury to the pancreas associated with inflammation, relatively common with an incidence rate of 10 to 20 cases per 100,000 people in Western countries. Common causes include biliary tract diseases and alcoholism.
- Chronic Pancreatitis: Irreversible loss of exocrine pancreatic parenchyma.
- Acute Pancreatitis Pathology:
- Caused by autodigestion of the pancreas by inappropriately activated pancreatic enzymes.
- Three pathways can incite the initial enzyme activation: pancreatic duct obstruction, primary acinar cell injury, and direct trauma.
- Pancreatic Duct Obstruction:
- Gallstones or biliary sludge impaction, or compression of the ductal system by a mass, resulting in increased intraductal pressure and accumulation of an enzyme-rich interstitial fluid.
- Lipase, secreted in an active form, can lead to local fat necrosis, contributing to local inflammation, interstitial edema, and vascular insufficiency.
- Primary Acinar Cell Injury:
- Impacts acute pancreatitis caused by ischemia, viral infections, drugs, and direct trauma to the pancreas.
- Defective intracellular transport of proenzymes within acinar cells can lead to blockage of ductal flow, increased intraductal pressure, and accumulation of enzyme-rich interstitial fluid.
- Acute Pancreatitis Histology:
- Alterations include microvascular leakage causing edema, fat necrosis by lipolytic enzymes, acute inflammation, proteolytic destruction of pancreatic parenchyma, and destruction of blood vessels resulting in interstitial hemorrhage.
- Acute necrotizing pancreatitis and hemorrhagic pancreatitis can lead to shock and fat necrosis in extra-pancreatic fat, the omentum, pancreatitis bowel mesentery, and even outside the abdominal cavity.
- Etiologic Factors:
- Alcoholism, hyperlipoproteinemia, hypercalcemia, medications (85 drugs), germline mutations in the cationic trypsinogen and trypsin inhibitor genes, mechanical issues (gallstones and obstruction of the pancreatic duct), trauma, iatrogenic injury, perioperative injury, endoscopic procedures with dye injection, vascular issues, and infections.
Overall, acute pancreatitis is a reversible inflammatory condition affecting the pancreas, while chronic pancreatitis is an irreversible condition with exocrine parenchyma loss. Acute pancreatitis is caused by autodigestion of the pancreas by inappropriately activated pancreatic enzymes, and it is associated with microvascular leakage, fat necrosis, acute inflammation, and proteolytic destruction of pancreatic parenchyma. Multiple etiologic factors can contribute to the development of acute pancreatitis, including alcoholism, biliary tract diseases, and medications, among others.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.