Podcast
Questions and Answers
Which statement best describes the difference in action between opioid agonists and agonist-antagonists?
Which statement best describes the difference in action between opioid agonists and agonist-antagonists?
- Agonists are only effective in acute pain management, while agonist-antagonists are used for chronic pain.
- Agonists fully activate opioid receptors, whereas agonist-antagonists only partially activate them. (correct)
- Agonists prevent opioid-induced respiratory depression, whereas agonist-antagonists potentiate their effects.
- Agonists have a higher risk of misuse, while agonist-antagonists are safer for long-term pain management.
A patient is experiencing respiratory depression due to an opioid overdose. Which medication would be most appropriate to reverse this effect?
A patient is experiencing respiratory depression due to an opioid overdose. Which medication would be most appropriate to reverse this effect?
- Butorphanol, as it is an example of an agonist-antagonist.
- Buprenorphine, as it acts as a partial agonist.
- Naloxone, as it has a stronger affinity to the opioid receptors than opioids. (correct)
- Pentazocine, since it provides some pain relief while reversing effects.
How do opioid agonist-antagonists differ from pure opioid agonists regarding effects on pain relief and potential for misuse?
How do opioid agonist-antagonists differ from pure opioid agonists regarding effects on pain relief and potential for misuse?
- Antagonist-agonists provide more effective pain relief with a lower potential for misuse compared to agonists.
- Agonists provide more effective pain relief but have a higher potential for misuse compared to agonist-antagonists. (correct)
- Both agonists and agonist-antagonists have similar levels of pain relief and potential for misuse.
- Agonist-antagonists offer stronger pain relief and thus have a higher risk of misuse.
Why is naloxone able to reverse opioid effects?
Why is naloxone able to reverse opioid effects?
In the context of obstetrical procedures, which type of opioid is more likely to be used for short-term pain control?
In the context of obstetrical procedures, which type of opioid is more likely to be used for short-term pain control?
Which of the following best describes the primary mechanism of action for opioid agonists?
Which of the following best describes the primary mechanism of action for opioid agonists?
What is a key characteristic of opioid agonist-antagonists compared to full opioid agonists?
What is a key characteristic of opioid agonist-antagonists compared to full opioid agonists?
Which statement accurately describes the action of opioid antagonists?
Which statement accurately describes the action of opioid antagonists?
How do opioid agonist-antagonists interact with full opioid agonists at the receptor level?
How do opioid agonist-antagonists interact with full opioid agonists at the receptor level?
Which of the following is the most accurate reason why opioid antagonists are used in cases of overdose?
Which of the following is the most accurate reason why opioid antagonists are used in cases of overdose?
Which of the following lists ONLY examples of full opioid agonists?
Which of the following lists ONLY examples of full opioid agonists?
What is the primary difference in receptor affinity between opioid agonists and antagonists?
What is the primary difference in receptor affinity between opioid agonists and antagonists?
Why are opioid agonist-antagonists considered to have a lower risk of misuse and addiction compared to full opioid agonists?
Why are opioid agonist-antagonists considered to have a lower risk of misuse and addiction compared to full opioid agonists?
According to the provided content, which of the following best describes the concept of pain?
According to the provided content, which of the following best describes the concept of pain?
What is the primary role of nociceptors in the pain pathway?
What is the primary role of nociceptors in the pain pathway?
Which of the following best represents the process of transduction in pain transmission?
Which of the following best represents the process of transduction in pain transmission?
According to the gate control theory, where does the modulation of pain signals primarily occur?
According to the gate control theory, where does the modulation of pain signals primarily occur?
Which of these chemical substances is NOT specifically mentioned as being released by injured cells that triggers nociceptors?
Which of these chemical substances is NOT specifically mentioned as being released by injured cells that triggers nociceptors?
What role do enkephalins and endorphins play in the context of pain modulation?
What role do enkephalins and endorphins play in the context of pain modulation?
In the context of understanding the process of pain, what distinguishes 'transmission' from 'transduction'?
In the context of understanding the process of pain, what distinguishes 'transmission' from 'transduction'?
What distinguishes opioid antagonists from non-opioid analgesics in the context of overdose management?
What distinguishes opioid antagonists from non-opioid analgesics in the context of overdose management?
Which of the following best describes a potential risk associated with using opioid antagonists in individuals physically dependent on opioids?
Which of the following best describes a potential risk associated with using opioid antagonists in individuals physically dependent on opioids?
Which therapeutic approach is MOST focused on influencing the 'gate' mechanism described by the Gate Control Theory?
Which therapeutic approach is MOST focused on influencing the 'gate' mechanism described by the Gate Control Theory?
In the event of a suspected opioid overdose, what does a failure of opioid antagonists to reverse the effects suggest?
In the event of a suspected opioid overdose, what does a failure of opioid antagonists to reverse the effects suggest?
Which of the following is a primary indication for the use of opioid analgesics as described in the content?
Which of the following is a primary indication for the use of opioid analgesics as described in the content?
In what context are opioid analgesics often considered first-line agents, according to the information provided?
In what context are opioid analgesics often considered first-line agents, according to the information provided?
What does the term 'balanced anesthesia' refer to in the context of opioid analgesic use?
What does the term 'balanced anesthesia' refer to in the context of opioid analgesic use?
Besides pain relief, which other therapeutic use does the content specifically mention for opioid analgesics?
Besides pain relief, which other therapeutic use does the content specifically mention for opioid analgesics?
What is a key difference between acetaminophen and NSAIDs discussed in the context of potential adverse effects?
What is a key difference between acetaminophen and NSAIDs discussed in the context of potential adverse effects?
What is the most serious adverse effect of opioid toxicity?
What is the most serious adverse effect of opioid toxicity?
Which of the following drugs is specifically indicated for reversing opioid-induced respiratory depression?
Which of the following drugs is specifically indicated for reversing opioid-induced respiratory depression?
What is an important consideration when administering naloxone in cases of opioid overdose?
What is an important consideration when administering naloxone in cases of opioid overdose?
Which symptom is NOT typical of opioid overdose?
Which symptom is NOT typical of opioid overdose?
How long can the effects of naloxone typically last?
How long can the effects of naloxone typically last?
What can be inferred if naloxone fails to reverse the effects of a presumed opioid overdose?
What can be inferred if naloxone fails to reverse the effects of a presumed opioid overdose?
What is likely to occur when someone who is physically dependent on opioids receives naloxone?
What is likely to occur when someone who is physically dependent on opioids receives naloxone?
When do withdrawal symptoms typically begin in opioid-naive patients who abruptly stop opioids?
When do withdrawal symptoms typically begin in opioid-naive patients who abruptly stop opioids?
Which opioid is primarily recommended for detoxification in opioid-dependent individuals?
Which opioid is primarily recommended for detoxification in opioid-dependent individuals?
What is a primary concern regarding transdermal patches for pain management?
What is a primary concern regarding transdermal patches for pain management?
Which of the following opioids is significantly more potent than morphine?
Which of the following opioids is significantly more potent than morphine?
Which mechanism of action is primarily associated with both oxycodone and methadone?
Which mechanism of action is primarily associated with both oxycodone and methadone?
What is a notable pharmacokinetic feature of methadone?
What is a notable pharmacokinetic feature of methadone?
Which opioid is indicated for effective pain management in opioid-tolerant individuals?
Which opioid is indicated for effective pain management in opioid-tolerant individuals?
Which of the following is the function of naloxone hydrochloride?
Which of the following is the function of naloxone hydrochloride?
Which opioid formulation is available in both immediate-release and sustained-release forms?
Which opioid formulation is available in both immediate-release and sustained-release forms?
Flashcards
Full Opioid Agonists
Full Opioid Agonists
These medications bind to opioid receptors and cause a full analgesic response, effectively reducing pain. Examples: Morphine, hydromorphone, oxycodone, fentanyl, methadone.
Opioid Agonist-Antagonists
Opioid Agonist-Antagonists
They bind to opioid receptors but produce a weaker analgesic response compared to full agonists. Also known as partial agonists or mixed agonists.
How do Opioid Agonist-Antagonists work?
How do Opioid Agonist-Antagonists work?
They compete with full agonists for binding sites on opioid receptors, potentially reducing the effects of those agonists. This lowers the risk of misuse and addiction.
Opioid Antagonists
Opioid Antagonists
Signup and view all the flashcards
How do Opioid Antagonists Work?
How do Opioid Antagonists Work?
Signup and view all the flashcards
Affinity (in drug action)
Affinity (in drug action)
Signup and view all the flashcards
Opioid Antagonists and Overdose
Opioid Antagonists and Overdose
Signup and view all the flashcards
Opioid Antagonists and Addiction
Opioid Antagonists and Addiction
Signup and view all the flashcards
Opioid Agonists
Opioid Agonists
Signup and view all the flashcards
Opioid Dependence
Opioid Dependence
Signup and view all the flashcards
Opioid Overdose
Opioid Overdose
Signup and view all the flashcards
Pain
Pain
Signup and view all the flashcards
Acute Pain
Acute Pain
Signup and view all the flashcards
Persistent Pain
Persistent Pain
Signup and view all the flashcards
Nociceptors
Nociceptors
Signup and view all the flashcards
Transduction
Transduction
Signup and view all the flashcards
Transmission
Transmission
Signup and view all the flashcards
Perception
Perception
Signup and view all the flashcards
Gate Theory
Gate Theory
Signup and view all the flashcards
What is the mechanism of action of opioid antagonists?
What is the mechanism of action of opioid antagonists?
Signup and view all the flashcards
What is the primary use of opioid antagonists?
What is the primary use of opioid antagonists?
Signup and view all the flashcards
What does it mean if an opioid antagonist doesn't reverse a presumed opioid overdose?
What does it mean if an opioid antagonist doesn't reverse a presumed opioid overdose?
Signup and view all the flashcards
What is a potential adverse effect of opioid antagonists?
What is a potential adverse effect of opioid antagonists?
Signup and view all the flashcards
What is the primary use of opioid analgesics?
What is the primary use of opioid analgesics?
Signup and view all the flashcards
What is a specific example of an opioid analgesic used for a non-pain condition?
What is a specific example of an opioid analgesic used for a non-pain condition?
Signup and view all the flashcards
When are opioid analgesics typically the first choice for pain management?
When are opioid analgesics typically the first choice for pain management?
Signup and view all the flashcards
What are some alternatives to opioid analgesics for pain relief?
What are some alternatives to opioid analgesics for pain relief?
Signup and view all the flashcards
Opioid Toxicity
Opioid Toxicity
Signup and view all the flashcards
Respiratory Depression
Respiratory Depression
Signup and view all the flashcards
Naloxone
Naloxone
Signup and view all the flashcards
Managing Opioid Overdose
Managing Opioid Overdose
Signup and view all the flashcards
Opioid Withdrawal
Opioid Withdrawal
Signup and view all the flashcards
Naltrexone
Naltrexone
Signup and view all the flashcards
Physical Dependence on Opioids
Physical Dependence on Opioids
Signup and view all the flashcards
What is Oxycodone?
What is Oxycodone?
Signup and view all the flashcards
Why is Oxycodone's oral bioavailability negligible?
Why is Oxycodone's oral bioavailability negligible?
Signup and view all the flashcards
What's Methadone's primary use?
What's Methadone's primary use?
Signup and view all the flashcards
What's unique about Dilaudid (hydromorphone)?
What's unique about Dilaudid (hydromorphone)?
Signup and view all the flashcards
What role does Naloxone (Narcan) play?
What role does Naloxone (Narcan) play?
Signup and view all the flashcards
How do opioids work?
How do opioids work?
Signup and view all the flashcards
What's the major risk associated with opioid use?
What's the major risk associated with opioid use?
Signup and view all the flashcards
Who might benefit from transdermal opioid patches?
Who might benefit from transdermal opioid patches?
Signup and view all the flashcards
Study Notes
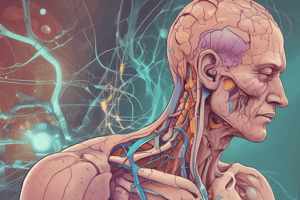
Pain Management with Drugs Affecting the Central Nervous System
- Pain is a complex, subjective experience influenced by factors beyond physiological stimuli.
- Pain is what the patient says it is.
- Acute and persistent pain require different management approaches.
- Other pain types include referred, neuropathic, phantom, and cancer pain.
- Nociception: The physiological process of pain perception involving specialized nerve fibers (nociceptors) that transmit pain signals to the brain.
- Tissue injury releases substances like bradykinin, histamine, prostaglandins, serotonin, substance P, and potassium.
- Gate Theory: Explains how pain signals are modulated in the spinal cord before reaching the brain. NSAIDs and antidepressants influence this gate mechanism.
Transduction
- Noxious stimuli transform into electrochemical energy.
- Injured cells release chemicals (prostaglandins, bradykinin, serotonin, substance P, histamine, and potassium), stimulating nociceptors.
- Nociceptors generate action potentials (electrical nerve impulses) in response to stimulation.
Transmission
- Action potentials travel along nociceptors and enter the spinal cord.
- The dorsal horn of the spinal cord acts as a gate, regulating the flow of the sensory impulses to the brain.
Perception
- Pain perception occurs if the spinal cord gate allows the impulses to reach the brain.
- Mu receptors are involved in the subjective sensation of pain.
Modulation
- The flow of pain impulses can be modulated at the dorsal horn.
- NSAIDs and antidepressants influence the gate mechanism, potentially reducing pain perception.
Pain Management
- World Health Organization's Three-Step Analgesic Ladder provides guidelines:
- Step 1: Nonopioids with or without adjuvant medications.
- Step 2: Opioids with or without nonopioids and adjuvants.
- Step 3: Opioids for moderate to severe pain with or without nonopioids or adjuvants.
Opioid Analgesics
- Potent painkillers that act on opioid receptors in the brain, reducing pain sensation.
- Agonists: Bind to opioid receptors (mu (μ), kappa (κ), and delta (δ)) and activate them for full analgesic response. Examples: Morphine, hydromorphone, oxycodone, fentanyl, methadone.
- Antagonists: Bind to opioid receptors but do not activate them; they block receptors, reversing opioid overdose and withdrawal symptoms. Examples: Naloxone, naltrexone.
- Agonist-Antagonists: Bind to opioid receptors but produce a weaker analgesic response. Examples: Buprenorphine, butorphanol, nalbuphine, pentazocine.
Adverse Effects of Opioids
- Respiratory depression, constipation, tolerance, and potential for addiction are significant risks.
- Other adverse effects include nausea, vomiting, and CNS depression like sedation, dizziness, and lightheadedness.
Opioid Overdose
- Toxicity occurs when excessive opioids are taken, resulting in severe adverse effects.
- Respiratory depression, altered mobility and speech, altered consciousness, and constricted pupils are involved.
- Naloxone (Narcan®) is used to reverse opioid-induced respiratory depression in overdose situations.
Opioid Withdrawal
- Withdrawal occurs when opioid use is stopped or significantly reduced.
- Symptoms include drug-seeking behavior, dilated pupils, sweating, runny nose, tearing, vomiting, diarrhea, insomnia, and elevated blood pressure/pulse.
Non-opioid Analgesics (NSAIDs)
- Common pain relievers that work by inhibiting COX enzymes (COX-1 and COX-2), which reduces inflammation.
- Examples: Aspirin, ibuprofen, and naproxen.
- Potential side effects include gastrointestinal bleeding, and interactions with other medications.
Acetaminophen
- Widely used analgesic and antipyretic that has little to no anti-inflammatory effects.
- Maximum daily dose should be considered for different age groups to avoid overdose.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.