Podcast
Questions and Answers
What is the main purpose of CamScanner?
What is the main purpose of CamScanner?
- To scan and digitize documents (correct)
- To edit videos
- To take high-resolution photographs
- To create graphic designs
Which feature is NOT associated with CamScanner?
Which feature is NOT associated with CamScanner?
- Document sharing
- Cloud storage options
- Video editing capabilities (correct)
- Optical character recognition
How does CamScanner enhance the quality of scanned documents?
How does CamScanner enhance the quality of scanned documents?
- By adding watermarks
- By adjusting lighting and cropping edges (correct)
- By using filters to modify colors
- By applying sound effects
What is a common use case for CamScanner in a professional setting?
What is a common use case for CamScanner in a professional setting?
Which of these capabilities allows CamScanner to be effective for mobile users?
Which of these capabilities allows CamScanner to be effective for mobile users?
What is the primary function of CamScanner?
What is the primary function of CamScanner?
Which of the following features is NOT typically associated with CamScanner?
Which of the following features is NOT typically associated with CamScanner?
What type of files can be generated by using CamScanner?
What type of files can be generated by using CamScanner?
In what way does CamScanner utilize Optical Character Recognition (OCR)?
In what way does CamScanner utilize Optical Character Recognition (OCR)?
Flashcards
CamScanner App
CamScanner App
A mobile application for scanning documents.
Scanning Documents
Scanning Documents
Converting paper documents into digital format.
Digitization
Digitization
Converting physical information into digital form.
Mobile Application
Mobile Application
Signup and view all the flashcards
Document Management
Document Management
Signup and view all the flashcards
Study Notes
Pain Management Definition
- Pain is a personal, subjective sensory and emotional experience associated with actual or potential tissue damage.
- It's defined as "whatever the experiencing person says it is, existing whenever he says it does." (McCaffery, 1999).
- All pain is real.
- Medically, pain is an unpleasant sensation ranging from mild, localized discomfort to agony.
- Pain has physical (nerve stimulation) and emotional components.
- Pain can be localized or diffuse.
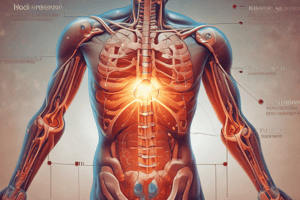
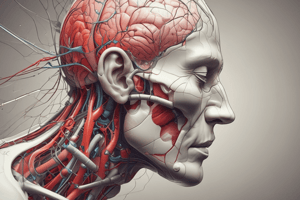
Pathophysiology of Pain
- Pain transmission involves three components: peripheral nervous system (afferent pathways), central nervous system and descending control system (efferent pathways).
- Nociceptors (pain receptors) are nerve endings that respond to intense stimuli.
- Nociceptors in every part of the body except large internal organs respond to inflammation, ischemia or stretching.
- Stimuli (mechanical, thermal, or chemical) trigger electrical activity (action potentials).
- Two types of afferent nerve fibers (Aδ and C fibers) transmit pain signals:
- Aδ fibers are smaller and myelinated, transmitting "fast pain" rapidly and precisely.
- C fibers are larger and unmyelinated, transmitting "slow pain" (dull, aching, burning) more diffusely.
- When nociceptors are stimulated, histamine and other algogenic (pain-causing) substances are released.
- These substances cause vasodilation (redness, warmth) and increased vascular permeability (swelling). Key chemicals include histamine, bradykinin, acetylcholine, serotonin, and substance P.
Ascending Pain Pathways
- Tissue damage stimulates nociceptors, transmitting pain signals to spinal cord dorsal horn, then lamina II (substantia gelatinosa).
- Signals are relayed to other parts of the spinal cord (reticular formation, hypothalamus, limbic system, cerebral cortex).
Descending Pain Pathways
- Descending fibers originate in the lower and midbrain, terminating in the dorsal horn of the spinal cord.
- These fibers block nociceptors.
- Endorphins and enkephalins reduce or inhibit pain transmission and perception. Endorphin receptors are present in ascending and descending pathways.
Gate Control Theory
- Peripheral nerve fibers carrying pain signals to the spinal cord can be modified before transmission to the brain.
- Gating mechanisms can either permit or inhibit pain transmission.
- Larger fibers (A-alpha and A-beta) inhibit pain transmission (gate closed), while smaller fibers (A-delta and C) facilitate it (gate open).
Neurophysiology of Pain - Neurotransmitters
- Substance P is necessary for pain transmission.
- Serotonin inhibits pain transmission.
- Prostaglandins increase pain sensitivity.
- Neuromodulators like endorphins and dynorphins cause analgesia (pain relief).
- Bradykinin and histamine increase pain sensation.
Types of Pain Stimuli
- Mechanical stimuli (trauma, surgery, inflammation, pressure on pain receptors, tumor pressure, muscle spasms).
- Thermal stimuli (extreme heat or cold).
- Chemical stimuli (tissue ischemia, lactic acid, chemicals, muscle spasms).
Types of Pain
- Classified by duration (acute or chronic).
- Classified by location (cutaneous, deep, visceral, radiating, referred, intractable, neuropathic, phantom).
Characteristics of Pain -
- Pain Intensity: The duration or intensity a person is willing to endure. Influenced by destruction, consciousness, activity, and expectations. Assess using pain scales.
- Pain Threshold: The smallest stimulus that elicits a pain response.
- Pain Tolerance: The maximum intensity or duration of pain a person can endure.
- Location: Determined by where the patient points to the affected area. Referred pain is felt in an area distant from the stimulus.
- Quality: Patients describe the pain in their own words (burning, aching, throbbing, stabbing, etc.).
- Aggravating/Alleviating Factors: Factors that increase or reduce pain (activity, medication, heat/cold, massage, etc.).
Factors Affecting Pain Experience
- Past experiences, anxiety, depression.
- Cultural values, age, gender, placebo effect, environment.
- Meaning of pain.
Physiologic Responses to Pain
- Autonomic nervous system response (e.g., dilated pupils, increased heart rate, blood pressure).
Pain Assessment
- Pain History: Previous pain treatments, when and what analgesics were last taken, and allergies.
- Location: Defining the location of the pain.
- Intensity: Using a scale (0-10).
- Quality: Describing the pain.
- Pattern: Onset, duration, recurrence.
- Precipitating and alleviating factors: Identifying factors that increase or decrease pain.
- Associated symptoms: Identifying other symptoms that accompany the pain.
- Effects on ADLs: Assessing impact on daily activities.
- Coping resources: Identifying resources for coping with pain.
- Affective responses: Assessing feelings like anxiety, fear.
Nursing Diagnoses
- Examples of potential diagnoses related to pain: ineffective airway clearance, activity intolerance, immobilization, self-care deficit, ineffective coping, deficient knowledge.
Pain Management Interventions
- Includes various strategies, including pain medication, massage, heat/cold therapy, distraction, and relaxation techniques.
Planning and Goals (for pain management)
- Examples of goals: patient will report reduced pain, express satisfaction with pain control, use of pain management strategies.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.