Podcast
Questions and Answers
What is the median age of onset for ovarian cancer?
What is the median age of onset for ovarian cancer?
- 63 years (correct)
- 55 years
- 45 years
- 70 years
Which imaging method is most commonly used for the evaluation of ovarian masses?
Which imaging method is most commonly used for the evaluation of ovarian masses?
- X-ray
- CT scan
- MRI
- Transvaginal ultrasound (correct)
What indicates a higher risk of malignancy in postmenopausal women with adnexal masses?
What indicates a higher risk of malignancy in postmenopausal women with adnexal masses?
- Size of the mass being larger than 10 cm (correct)
- Presence of ascites
- Unilateral pelvic pain
- Presence of a cystic mass
Which condition is most likely associated with elevated CA-125 in a premenopausal woman?
Which condition is most likely associated with elevated CA-125 in a premenopausal woman?
For a 35-year-old woman with a single affected family member, what is her risk of developing ovarian cancer?
For a 35-year-old woman with a single affected family member, what is her risk of developing ovarian cancer?
In which circumstance is CA-125 most useful regarding malignancy likelihood?
In which circumstance is CA-125 most useful regarding malignancy likelihood?
Which of the following is NOT a reason for referral to gynecologic oncology?
Which of the following is NOT a reason for referral to gynecologic oncology?
Which symptom may indicate ovarian torsion?
Which symptom may indicate ovarian torsion?
What is the risk of ovarian cancer for a woman with a BRCA1 gene mutation by age 70?
What is the risk of ovarian cancer for a woman with a BRCA1 gene mutation by age 70?
What is a common characteristic of a mucinous cystadenoma?
What is a common characteristic of a mucinous cystadenoma?
Which symptom is commonly associated with tubo-ovarian abscess?
Which symptom is commonly associated with tubo-ovarian abscess?
What fluid characteristic is associated with endometriomas?
What fluid characteristic is associated with endometriomas?
Which management option is NOT appropriate for a mature cystic teratoma?
Which management option is NOT appropriate for a mature cystic teratoma?
What is a key diagnostic characteristic of malignant ovarian masses on ultrasound?
What is a key diagnostic characteristic of malignant ovarian masses on ultrasound?
In the case of ovarian torsion, which sign is most commonly observed during examination?
In the case of ovarian torsion, which sign is most commonly observed during examination?
Which condition is NOT considered when managing tubo-ovarian abscesses?
Which condition is NOT considered when managing tubo-ovarian abscesses?
What is the most significant independent risk factor for ovarian cancer?
What is the most significant independent risk factor for ovarian cancer?
Which of the following is NOT a symptom that may suggest a malignant ovarian mass?
Which of the following is NOT a symptom that may suggest a malignant ovarian mass?
What is the likely management approach for an asymptomatic benign ovarian mass?
What is the likely management approach for an asymptomatic benign ovarian mass?
Which diagnostic imaging technique is useful for detecting endometriomas?
Which diagnostic imaging technique is useful for detecting endometriomas?
Which condition is most likely to cause an acute surgical emergency due to sepsis?
Which condition is most likely to cause an acute surgical emergency due to sepsis?
What is a common complication associated with untreated pelvic inflammatory disease (PID)?
What is a common complication associated with untreated pelvic inflammatory disease (PID)?
Which finding would prompt urgent referral to a gynecologic oncologist?
Which finding would prompt urgent referral to a gynecologic oncologist?
What is a characteristic feature of a follicular cyst?
What is a characteristic feature of a follicular cyst?
Which of the following is NOT a type of benign ovarian cyst?
Which of the following is NOT a type of benign ovarian cyst?
How are theca lutein cysts typically characterized?
How are theca lutein cysts typically characterized?
What is a possible symptom of a corpus luteum cyst?
What is a possible symptom of a corpus luteum cyst?
Which imaging technique is primarily used for diagnosing a follicular cyst?
Which imaging technique is primarily used for diagnosing a follicular cyst?
During which phase of the ovarian cycle do follicular cysts primarily occur?
During which phase of the ovarian cycle do follicular cysts primarily occur?
What is the general management approach for asymptomatic follicular cysts?
What is the general management approach for asymptomatic follicular cysts?
What distinguishes a tubo-ovarian abscess from a benign cyst?
What distinguishes a tubo-ovarian abscess from a benign cyst?
Which type of cyst is most frequently encountered in the normal ovary during the reproductive age?
Which type of cyst is most frequently encountered in the normal ovary during the reproductive age?
What characteristic is commonly associated with theca lutein cysts?
What characteristic is commonly associated with theca lutein cysts?
What is a primary reason a functional cyst, such as a corpus luteum cyst, may present with acute pain?
What is a primary reason a functional cyst, such as a corpus luteum cyst, may present with acute pain?
Which symptom is most commonly associated with larger follicular cysts?
Which symptom is most commonly associated with larger follicular cysts?
What distinguishes a benign ovarian cyst from a malignant one during ultrasound evaluation?
What distinguishes a benign ovarian cyst from a malignant one during ultrasound evaluation?
Which classification of ovarian cysts includes conditions like tubo-ovarian abscess and endometrioma?
Which classification of ovarian cysts includes conditions like tubo-ovarian abscess and endometrioma?
What is the typical management approach for an asymptomatic follicular cyst?
What is the typical management approach for an asymptomatic follicular cyst?
Which type of ovarian cyst is associated with prolonged secretion of progesterone post-ovulation?
Which type of ovarian cyst is associated with prolonged secretion of progesterone post-ovulation?
Which factor is least likely to affect the utility of CA-125 as a biomarker for ovarian cancer in postmenopausal women?
Which factor is least likely to affect the utility of CA-125 as a biomarker for ovarian cancer in postmenopausal women?
What is the most critical aspect determining the likelihood of malignancy in an adnexal mass of a postmenopausal woman?
What is the most critical aspect determining the likelihood of malignancy in an adnexal mass of a postmenopausal woman?
In which scenario is imaging considered least effective for evaluating ovarian cancer risk?
In which scenario is imaging considered least effective for evaluating ovarian cancer risk?
For women with a history of family cancer, what is the least significant genetic factor related to ovarian cancer risk?
For women with a history of family cancer, what is the least significant genetic factor related to ovarian cancer risk?
What aspect of CA-125 elevation makes it particularly complex in interpreting results in premenopausal women?
What aspect of CA-125 elevation makes it particularly complex in interpreting results in premenopausal women?
Which of the following imaging characteristics is not typically concerning when evaluating an adnexal mass?
Which of the following imaging characteristics is not typically concerning when evaluating an adnexal mass?
What symptom is most indicative of a non-malignant condition associated with adnexal masses?
What symptom is most indicative of a non-malignant condition associated with adnexal masses?
How effective is transvaginal ultrasound in the early evaluation of masses in asymptomatic postmenopausal women?
How effective is transvaginal ultrasound in the early evaluation of masses in asymptomatic postmenopausal women?
Elevated CA-125 is least likely to be associated with which of the following conditions?
Elevated CA-125 is least likely to be associated with which of the following conditions?
What is the primary reason that biomarker panels are not beneficial as an initial assessment tool for ovarian cancer?
What is the primary reason that biomarker panels are not beneficial as an initial assessment tool for ovarian cancer?
What is typically the most common symptom associated with mucinous cystadenomas?
What is typically the most common symptom associated with mucinous cystadenomas?
Which of the following statements accurately describes the management of tubo-ovarian abscesses?
Which of the following statements accurately describes the management of tubo-ovarian abscesses?
What is a distinguishing feature of mature cystic teratomas?
What is a distinguishing feature of mature cystic teratomas?
What type of fluid is typically found in endometriomas?
What type of fluid is typically found in endometriomas?
Which condition is associated with the risk of ovarian torsion?
Which condition is associated with the risk of ovarian torsion?
Which ultrasound finding is suggestive of a malignant ovarian mass?
Which ultrasound finding is suggestive of a malignant ovarian mass?
What is the primary risk factor associated with the incidence of ovarian cancer?
What is the primary risk factor associated with the incidence of ovarian cancer?
In what scenario would it be critical to refer a patient to a gynecologic oncologist?
In what scenario would it be critical to refer a patient to a gynecologic oncologist?
Which condition may lead to chronic complications such as infertility and ectopic pregnancy?
Which condition may lead to chronic complications such as infertility and ectopic pregnancy?
What symptom commonly suggests ovarian cancer in women?
What symptom commonly suggests ovarian cancer in women?
Which type of cyst is characterized by multiloculated fluid collection?
Which type of cyst is characterized by multiloculated fluid collection?
Which surgical intervention is most appropriate for a suspected ruptured tubo-ovarian abscess?
Which surgical intervention is most appropriate for a suspected ruptured tubo-ovarian abscess?
What typically distinguishes serous cystadenomas from other ovarian tumors?
What typically distinguishes serous cystadenomas from other ovarian tumors?
What is the typical approach for managing a benign functional cyst?
What is the typical approach for managing a benign functional cyst?
Flashcards are hidden until you start studying
Study Notes
Ovarian Disorders: Benign
-
Follicular Cyst (Functional Cyst): Most common ovarian cyst in reproductive-aged women. Occurs when a follicle persists (doesn't ovulate) or an immature follicle fails to degenerate.
- Symptoms: Mostly asymptomatic, larger cysts can cause pelvic heaviness and dull pain. Delayed menses followed by heavy bleeding can occur if estrogen production from the follicle continues. Severe pain may indicate hemorrhage, rupture, or torsion.
- Diagnosis: Pelvic exam, transvaginal ultrasound (TUS).
- Management: Expectant for asymptomatic, simple cysts. Follow-up exam and ultrasound in 6-12 weeks. Oral contraceptives can be helpful to reduce cyst development but are not effective for reducing the size of an existing cyst. Surgery is indicated for acute pain suggestive of torsion or suspicion of malignancy.
-
Corpus Luteum Cyst (Functional Cyst): Results from bleeding within a follicle after ovulation. Can be associated with normal endocrine function or prolonged progesterone secretion.
- Complications: Acute pain and rupture with intraperitoneal bleeding.
-
Theca Lutein Cysts (Functional): Almost always bilateral and can be massive (20-30 cm). Develop due to prolonged or excessive ovarian stimulation from endogenous or exogenous gonadotropins (Gn).
- Important: The large ovaries can lead to ascites (fluid accumulation in the abdomen) and hemoconcentration (increased blood thickness), which increases the risk of clotting.
-
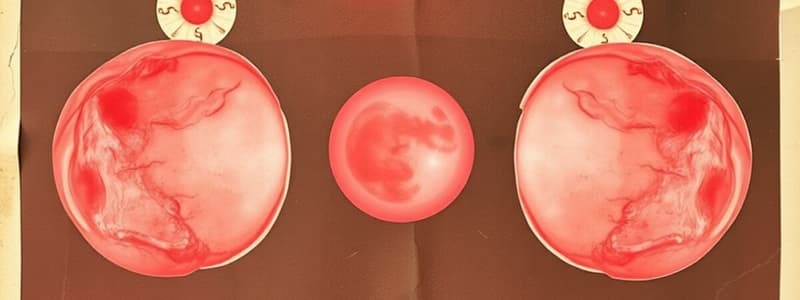
Cystadenoma (Serous or Mucinous): Benign tumor of ovarian surface epithelium. Lined by simple epithelium that can be serous or mucinous.
- Serous cystadenoma: Filled with pale yellow serous fluid, usually unilocular (single chamber).
- Mucinous cystadenoma: Filled with sticky mucin, typically multiloculated (multiple chambers). Can be very large (over 20 cm), the largest of all ovarian tumors.
-
Tubo-ovarian Abscess (TOA): Infectious disorder of the upper genital tract (pelvic inflammatory disease, PID). Results in an inflammatory mass involving the fallopian tube and ovary.
- Incidence: Often bilateral due to ascending infection.
- Symptoms/Complications: Symptoms of PID, adnexal pain and mass. Can become a surgical emergency if sepsis or rupture occurs. Chronic complications include tubal occlusion, infertility, ectopic pregnancy, and chronic pelvic pain due to adhesions.
- Diagnosis: Pelvic exam and TUS.
- Management: Inpatient intravenous antibiotics with coverage for gonorrhea, chlamydia, and anaerobes. Laparoscopy is not indicated unless there is no improvement or worsening symptoms suspicious for rupture or if the diagnosis is in question.
-
Endometrioma (Chocolate Cyst): Ovarian cyst arising from ectopic endometrial tissue within the ovary. Contain thick, brown, tar-like fluid. Often densely adherent to surrounding structures.
- Symptoms/Complications: Symptoms of endometriosis, pelvic pain, dysmenorrhea, dyspareunia.
- Diagnosis: TUS with characteristic internal echogenicity.
- Management: Surgical intervention for pain relief, exclusion of malignancy, and infertility. Conservative surgery includes cystectomy at laparoscopy or laparotomy. Definitive surgery involves oophorectomy.
-
Mature Cystic Teratoma (Dermoid): Benign neoplasm arising from a single germ cell containing tissue from all three germ layers: ectoderm, mesoderm, and endoderm.
- Incidence: Most common benign neoplasm in women under 35, including adolescents. 10-15% are bilateral.
- Symptoms/Complications: Torsion (twisting) with pain in 15%.
- Diagnosis: Often discovered incidentally on pelvic exam, abdominal X-ray or TUS.
- Management: Observation is not appropriate. Operative laparoscopy with cystectomy or oophorectomy (conserve ovary if fertility is desired). Avoid spillage of cyst contents to prevent peritonitis. Laparotomy is only indicated if malignancy is suspected.
-
Paraovarian Cyst or Fibroid: Simple epithelial-lined cyst (rarely complex) or benign fibroid located adjacent to the ovary, usually within the broad ligament.
-
Ovarian (Adnexal) Torsion: Rotation of the ovary or ovary and fallopian tube to a degree that occludes blood supply. Can be partial, intermittent, or complete, resulting in necrosis.
- Incidence: Most common in reproductive-aged women. Ovaries that are enlarged are more susceptible. Rare in malignancy.
- Diagnosis: Pelvic exam, TUS with Doppler flow studies.
- Management: Surgical emergency. Laparoscopy or laparotomy.
Ovarian Disorders: Malignant
-
History Suggesting a Malignant Ovarian Mass: Abdominal pain, dyspepsia, bloating, increased abdominal girth, early satiety, weight loss, fatigue, dyspnea (due to ascites or pleural effusion). Important to note the history of any benign cysts, as malignant masses may present similarly.
-
Physical Exam Findings Suggesting a Malignant Ovarian Mass: Weight loss, pleural effusion, jaundice, ascites, abdominal distention, nodular or fixed pelvic mass, possibly very large.
-
Ultrasound Findings Suggesting a Malignant Ovarian Mass: Thick septations, papillary projections into the cyst lumen, intramural nodule, cystic and solid components, increased overall ovarian volume, increased Doppler blood flow.
-
When to Refer to a Gynecologic Oncologist: Any woman with a pelvic mass and any of the following characteristics should be referred:
- Elevated CA 125 level: >35 in postmenopausal women, >200 in premenopausal women.
Cancer of the Ovary
-
Detection: Most ovarian cancers are detected incidentally on physical exam or during pelvic imaging (ultrasound, CT, MRI).
-
Differential Diagnosis of a Pelvic Mass: May be gynecologic or non-gynecologic in origin. Consider location of the mass, patient age, and reproductive status:
- Gynecologic causes: Benign or malignant ovarian lesions, tubal or paratubal processes (hydrosalpinges or ectopic pregnancy), uterine abnormalities (leiomyomas or Mullerian abnormalities).
- Non-gynecologic causes: Less common. May be related to other systems like the gastrointestinal (GI) or urologic systems, or metastatic cancer (especially breast, colon, gastric).
-
Risk factors:
- Most important independent risk factor: Age. Incidence increases sharply after menopause. Median age of onset is 63.
- Most important personal risk factor: Strong family history of breast or ovarian cancer.
-
Evaluation:
-
Symptoms: Can help refine differential diagnosis.
- Acute onset of abdominal or pelvic pain may suggest hemorrhagic or bleeding ovarian cyst. Important to assess for pregnancy as ectopic pregnancy is a possibility.
- Unilateral, intermittent, then acutely worsening pelvic pain may indicate ovarian torsion.
- Indolent, progressive pelvic pain with fever, chills, vomiting, and vaginal discharge may indicate an infectious etiology like TOA.
- Acute or chronic dysmenorrhea or pain with intercourse may suggest an endometrioma.
-
Imaging:
- Transvaginal ultrasound (TUS): Most commonly used. Assess size, composition, laterality, presence of septations, nodules, papillary excrescences, and free fluid in the pelvis. Consider Doppler characteristics.
- MRI: Not routinely recommended. May be useful for better characterization of origin.
- CT: Best for detecting abdominal metastatic disease or determining origin.
-
Serum Marker Testing: Used in conjunction with imaging.
- CA-125: Most commonly used protein associated with epithelial ovarian malignancies. Also expressed at lower levels in non-malignant tissue. Elevation can occur in endometriosis, pregnancy, PID, non-gynecologic cancer. Most useful in postmenopausal women. Elevated in 80% of patients with epithelial ovarian cancer but only 50% with stage 1 disease.
-
-
Utility of CA-125: Not useful as a screening test for ovarian cancer, even in high-risk women. Pelvic ultrasound is also not useful as a screening test. CA-125 can be helpful when used in conjunction with other findings. CA-125 elevation is more likely to indicate malignancy in postmenopausal women. A referral to a gynecologic oncologist should be considered if a postmenopausal woman presents with a mass and elevated CA-125.
-
Biomarker Panels: Less useful as an initial assessment tool but may be more appropriate in cases where surgery has been performed to further determine if a gynecologic oncology referral is needed. Many of these tests are still under investigation and their clinical utility is being studied.
-
Ovarian Cancer Risk with Family History:
- For a 35-year-old woman with a single affected family member, the lifetime risk increases from 1.6% to 5%.
- For a woman with a BRCA1 gene mutation, the lifetime risk of ovarian cancer, fallopian tube cancer, or peritoneal cancer is 41-46% by age 70.
Ovarian Disorders
- Benign Ovarian Disorders: These disorders can be physiologic (functional) or non-functional.
- Follicular Cyst:
- Most common cystic structure in normal ovaries
- Occurs in women of reproductive age (ovulatory).
- Arises from a persistent unovulated follicle or an immature follicle that fails to undergo atresia.
- Often asymptomatic, but can cause pelvic heaviness, dull pain, and irregular periods.
- Management: Expectant (if asymptomatic) or oral contraceptives (if recurring or symptomatic).
- Corpus Luteum Cyst:
- Occurs after ovulation due to intrafollicular bleeding.
- Associated with normal endocrine function or prolonged progesterone secretion.
- Can cause acute pain and may rupture, leading to bleeding.
- Theca Lutein Cyst:
- Typically bilateral.
- Can grow large (up to 20-30 cm) and are easily identified by ultrasound.
- Result from prolonged or excessive stimulation of ovaries by hormones (like those used for fertility treatments).
- Can cause ascites and hemoconcentration.
- Cystadenoma (Serous or Mucinous):
- Benign tumor of ovarian surface epithelium.
- Serous cystadenomas are filled with clear fluid.
- Mucinous cystadenomas are filled with sticky mucin and tend to be multiloculated.
- Often asymptomatic, but larger tumors can cause bloating or pelvic pressure.
- Management: Surgical removal with frozen section for staging (oncologist).
- Tubo-ovarian Abscess (TOA):
- Infectious disorder of the upper genital tract.
- Can be bilateral and present with symptoms of Pelvic Inflammatory Disease (PID), adnexal pain, and mass.
- Can be a surgical emergency if sepsis or rupture occurs.
- Management: Inpatient IV antibiotics and laparoscopy (if no improvement or suspicion of rupture).
- Endometrioma (Chocolate Cyst):
- Benign mass that occurs from growth of ectopic endometrial tissue within the ovary.
- Typically contain thick brown fluid and may be adherent to surrounding tissues.
- Often presents with symptoms of endometriosis like pelvic pain, dysmenorrhea, and dyspareunia.
- Management: Surgical removal (cystectomy or oophorectomy) for pain relief and preventing malignancy.
- Mature Cystic Teratoma (Dermoid):
- Benign tumor that arises from single germ cell containing tissue from all three germ layers (ectoderm, mesoderm, and endoderm).
- Most common benign tumor in women under 35, including adolescents.
- Often discovered incidentally on physical exam or imaging.
- Management: Surgical removal (cystectomy or oophorectomy) with precautions taken to avoid spillage of cyst contents.
- Paraovarian Cyst:
- Simple epithelial-lined cyst near the ovary, usually within the broad ligament.
- Ovarian (Adnexal) Torsion:
- Rotation of the ovary or ovary and fallopian tube that restricts blood flow.
- Most common in women of reproductive age who have enlarged ovaries.
- Can be an emergency.
- Management: Surgical intervention (laparoscopy or laparotomy) to restore blood flow.
- Follicular Cyst:
Ovarian Cancer
- Risk Factors:
- Age: Most important factor, with risk increasing after menopause (~63 years old).
- Family History: Strong family history of breast or ovarian cancer is a significant risk factor.
- Symptoms:
- Early Stages: Often asymptomatic.
- Later Stages: Abdominal pain, bloating, early satiety, weight loss, fatigue, dyspnea.
- Diagnosis:
- Imaging: Transvaginal ultrasound is the most common, looking for size, composition, laterality, and other features indicative of malignancy.
- Serum Marker Testing: CA-125 is a protein associated with epithelial ovarian malignancies.
- Biomarker Panels: Although under investigation, may help determine if further assessment (by gynecologic oncologist) is necessary.
- Management:
- Referral to Gynecologic Oncologist: Women with a pelvic mass and elevated CA-125 level in postmenopausal women or any woman with symptoms suggestive of malignancy should be referred to a gynecologic oncologist.
- Prognosis:
- Age, stage of cancer, and underlying health condition play a significant role.
- Early detection and treatment offer the best chance of survival.
Ovarian Disorders - Important Considerations
- Differential Diagnosis: When encountering a pelvic mass, it's important to consider both gynecologic and non-gynecologic causes (e.g., ectopic pregnancy, endometriosis, fibroids, gastrointestinal conditions, and metastatic cancer).
- Conservative Treatment: For many benign ovarian disorders, expectant management or conservative treatment (e.g., oral contraceptives) may be appropriate. However, regular follow-up and close monitoring are crucial.
- Surgical Intervention: Surgical intervention becomes necessary for certain conditions like TOA, endometriomas, dermoid cysts, and ovarian torsion.
- Importance of Referral: Depending on the findings, referral to specialists (e.g., gynecologic oncologist) may be critical for timely diagnosis and treatment, especially for suspected malignancies.
- Screening: At this time, there are no effective screening methods for routine detection of ovarian cancer. However, understanding risk factors and being aware of symptoms can help with early detection.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.