Podcast
Questions and Answers
What is the primary cause of pyogenic osteomyelitis?
What is the primary cause of pyogenic osteomyelitis?
- Fungal infection
- Viral infection
- Parasitic infection
- Bacterial infection (correct)
Which bone area is most affected during the acute phase of pyogenic osteomyelitis?
Which bone area is most affected during the acute phase of pyogenic osteomyelitis?
- Epiphysis
- Metaphysis (correct)
- Diaphysis
- Periosteum
What pathological feature is characteristic of chronic pyogenic osteomyelitis?
What pathological feature is characteristic of chronic pyogenic osteomyelitis?
- Granulomatous inflammation
- Cyst formation
- Fibroblast activity
- Sequestrum formation (correct)
What is a common complication of osteomyelitis related to the spine?
What is a common complication of osteomyelitis related to the spine?
How does septic arthritis primarily spread?
How does septic arthritis primarily spread?
Which type of arthritis involves immune-related joint damage without direct infection?
Which type of arthritis involves immune-related joint damage without direct infection?
What is a significant complication associated with tuberculous osteomyelitis?
What is a significant complication associated with tuberculous osteomyelitis?
Which of the following pathogens is commonly associated with septic arthritis?
Which of the following pathogens is commonly associated with septic arthritis?
Flashcards are hidden until you start studying
Study Notes
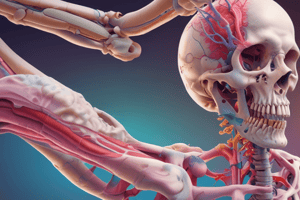
Osteomyelitis and Joint Infections
- Definition: Osteomyelitis is an inflammation of the bone and marrow caused by infection.
- Types:
- Pyogenic Osteomyelitis: Bacterial infection.
- Tuberculous Osteomyelitis: Mycobacterium tuberculosis infection.
- Septic Arthritis: Infection within a joint.
- Non-Infectious Arthritis: Immune-mediated joint damage without direct infection.
Pyogenic Osteomyelitis
- Transmission:
- Hematogenous: Spread through the bloodstream.
- Direct Extension: From nearby infections.
- Trauma: Injury to the bone.
- Pathogenesis:
- Commonly affects long bones: Especially around growth plates where blood flow is slower.
- Acute Phase: Bacteria enters and proliferates in the metaphysis (ends of long bones).
- Chronic Phase: Leads to:
- Sequestrum: Necrotic bone.
- Involucrum: New bone surrounding necrosis.
- Cloaca: Draining sinuses.
- Complications:
- Septicemia (blood poisoning).
- Bacterial arthritis.
- Pathological fractures.
- Amyloidosis (build-up of abnormal proteins).
Tuberculous Osteomyelitis
- Less common than pyogenic osteomyelitis.
- Usually secondary to tuberculosis in other parts of the body, like the lungs.
- Pathology:
- Granulomatous inflammation.
- Caseation (necrotic tissue).
- Commonly affects lower thoracic and lumbar vertebrae: Known as Pott's Disease.
- Complications:
- Vertebral collapse.
- Spinal cord compression.
- "Cold" abscesses (without acute inflammation).
Septic Arthritis
- Infection spreads to joints:
- Hematogenously: Through the bloodstream.
- Direct Extension: From osteomyelitis.
- Trauma: Injury to the joint.
- Common pathogens:
- Gonococcal bacteria: Often affects single joints.
- Brucella: May cause chronic arthritis.
- Complications:
- Progressive joint destruction.
- Fibrosis.
- Ankylosis (joint fusion).
Non-Infectious Arthritis
- Types:
- Rheumatoid arthritis: Autoimmune disease affecting joints.
- Spondyloarthropathies: Examples include ankylosing spondylitis.
- Key feature: Immune-related joint damage without direct infection.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.