Podcast
Questions and Answers
Which factor is not listed as a predisposing factor to candidal infection?
Which factor is not listed as a predisposing factor to candidal infection?
- Diabetes mellitus
- Stress (correct)
- Malnutrition/malabsorption
- Age
What is the normal presence of Candida albicans in healthy mouths attributed to?
What is the normal presence of Candida albicans in healthy mouths attributed to?
- Excessive saliva production
- Symbiotic relationship with lactobacillus acidophilus (correct)
- Poor oral hygiene
- High sugar diet
What is the most common oral fungal infection in humans?
What is the most common oral fungal infection in humans?
- Candidiasis (correct)
- Aspergillosis
- Histoplasmosis
- Cryptococcosis
What is the defined term for multiple diseases caused by the yeast fungus Candida?
What is the defined term for multiple diseases caused by the yeast fungus Candida?
What percentage of healthy people carry the infection of Candida albicans without clinical manifestations?
What percentage of healthy people carry the infection of Candida albicans without clinical manifestations?
What limits the proliferation of Candida albicans in the mouth?
What limits the proliferation of Candida albicans in the mouth?
In which group is the immune system not well developed, leading to a predisposition for candidal infection?
In which group is the immune system not well developed, leading to a predisposition for candidal infection?
Which antifungal agent is available as a cream and oral gel under the brand Daktarin?
Which antifungal agent is available as a cream and oral gel under the brand Daktarin?
Which antifungal agent is contraindicated in acute liver disease and pregnancy?
Which antifungal agent is contraindicated in acute liver disease and pregnancy?
Which antifungal agent is administered intravenously for deep and systemic candidosis?
Which antifungal agent is administered intravenously for deep and systemic candidosis?
Which antifungal agent is used with caution with anticoagulant, antiepileptic, and antidiabetic medications?
Which antifungal agent is used with caution with anticoagulant, antiepileptic, and antidiabetic medications?
Which antifungal agent is effective in angular stomatitis and should be taken 2 hours after antacids?
Which antifungal agent is effective in angular stomatitis and should be taken 2 hours after antacids?
Which antifungal agent acts by forming holes in the fungal cell membranes causing cell lysis?
Which antifungal agent acts by forming holes in the fungal cell membranes causing cell lysis?
Which antifungal agent is available as 200 mg tablet and as a cream?
Which antifungal agent is available as 200 mg tablet and as a cream?
Which antifungal agent is used for superficial, deep, and systemic mycosis?
Which antifungal agent is used for superficial, deep, and systemic mycosis?
Which antifungal agent is to be sucked four times a day or applied as a 3% ointment several times a day?
Which antifungal agent is to be sucked four times a day or applied as a 3% ointment several times a day?
Which factor can lead to secondary candida infection due to decreased salivary IgA?
Which factor can lead to secondary candida infection due to decreased salivary IgA?
Which condition can cause oral candidiasis by decreasing neutrophil function and blood flow?
Which condition can cause oral candidiasis by decreasing neutrophil function and blood flow?
Which drug type can lead to oral candidiasis?
Which drug type can lead to oral candidiasis?
Which form of candidosis is most frequently encountered, typically affecting infants, immunocompromised adults, and older individuals?
Which form of candidosis is most frequently encountered, typically affecting infants, immunocompromised adults, and older individuals?
Which condition can lead to postoperative oral candidiasis?
Which condition can lead to postoperative oral candidiasis?
Which factor can decrease lymphocytes and phagocytic activity, leading to oral candidiasis?
Which factor can decrease lymphocytes and phagocytic activity, leading to oral candidiasis?
Which disease can lead to oral candidiasis due to the effect of cytotoxic drugs on the immune system?
Which disease can lead to oral candidiasis due to the effect of cytotoxic drugs on the immune system?
What is a potential cause of angular cheilitis?
What is a potential cause of angular cheilitis?
Which antifungal treatment is recommended for mixed or recurrent infections of angular cheilitis?
Which antifungal treatment is recommended for mixed or recurrent infections of angular cheilitis?
What is a characteristic symptom of median rhomboid glossitis?
What is a characteristic symptom of median rhomboid glossitis?
Why is systemic therapy considered for symptomatic median rhomboid glossitis?
Why is systemic therapy considered for symptomatic median rhomboid glossitis?
What is chronic hyperplastic candidosis associated with?
What is chronic hyperplastic candidosis associated with?
What characterizes chronic mucocutaneous candidosis (CMCC)?
What characterizes chronic mucocutaneous candidosis (CMCC)?
Which antifungal drug is mentioned as part of the treatment for oral candidosis?
Which antifungal drug is mentioned as part of the treatment for oral candidosis?
Flashcards are hidden until you start studying
Study Notes
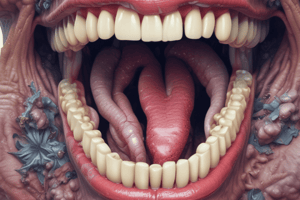
Oral Candidosis: Types, Etiology, and Treatment
- Angular cheilitis is caused by reduced vertical face height due to old dentures, severe attrition of natural dentition, nutritional deficiencies, oral dryness, or drooling.
- Topical antifungal treatment for angular cheilitis includes nystatin or amphotericin suspension and cream, while miconazole gel is used for mixed or recurrent infections.
- Median rhomboid glossitis is a symptomless, pink rhomboid area lacking lingual papillae, associated with immunosuppression, corticosteroid inhalers, tobacco use, dry mouth, or diabetes.
- Systemic therapy is considered for symptomatic median rhomboid glossitis, as topical antifungal therapy is ineffective.
- Chronic hyperplastic candidosis, potentially malignant, presents as a thick, white plaque with rough surface and is associated with heavy smoking in middle-aged men.
- Chronic mucocutaneous candidosis (CMCC) is characterized by recurrent Candida infections due to impaired cell-mediated immunity and can be caused by thymic aplasia, endocrinopathies, or defective cell-mediated immunity.
- CMCC types include familial, diffuse candidal granuloma, candidosis endocrinopathy syndrome, late-onset CMCC, and CMCC associated with primary immunodeficiency or HIV infection.
- CMCC treatment includes imidazole antifungal drugs, but it responds poorly to topical treatment and rapidly reappears after discontinuation.
- Rare systemic fungal infections of the mouth include aspergillosis, histoplasmosis, blastomycosis, cryptococcosis, paracoccidioidomycosis, and mucormycosis.
- The diagnosis of candidosis involves a case history, clinical examination, bacterial smear and culture, candidal antibody titer, and biopsy for candidal leukoplakia.
- Treatment of oral candidosis includes eliminating predisposing factors, using topical or systemic antifungal agents, and adjusting the duration of treatment based on the type of candidosis.
- Antifungal agents for oral candidosis include nystatin, amphotericin, imidazole antifungal agents (miconazole, ketoconazole, fluconazole, itraconazole), and chlorhexidine. Nystatin can be administered as a suspension or pastille.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.