Podcast
Questions and Answers
What is the primary purpose of fluorescein angiography in eye examinations?
What is the primary purpose of fluorescein angiography in eye examinations?
- Record blood flow to the retina (correct)
- Asses for macular degeneration
- Evaluate intraocular pressure
- Detect cataracts
Which of the following is NOT a risk factor associated with developing myopia?
Which of the following is NOT a risk factor associated with developing myopia?
- Prolonged use of corticosteroids
- Trauma to the eye (correct)
- Family history of myopia
- Thin cornea
What is the normal range for intraocular pressure (IOP) measured in mm Hg?
What is the normal range for intraocular pressure (IOP) measured in mm Hg?
- 15 - 25
- 8 - 14
- 20 - 30
- 10 - 21 (correct)
Which of the following medications promotes aqueous outflow in the treatment of glaucoma?
Which of the following medications promotes aqueous outflow in the treatment of glaucoma?
What condition is indicated by the presence of neovascularization in the retina?
What condition is indicated by the presence of neovascularization in the retina?
In which condition would an increase in intraocular pressure commonly occur?
In which condition would an increase in intraocular pressure commonly occur?
What eye condition does miosis primarily help to treat?
What eye condition does miosis primarily help to treat?
Which imaging technique provides high-resolution, cross-sectional color images of the interior surfaces of the eye?
Which imaging technique provides high-resolution, cross-sectional color images of the interior surfaces of the eye?
Flashcards
Fluorescein drops
Fluorescein drops
Used to identify abrasions on the eye.
Fluorescein angiography
Fluorescein angiography
Records blood flow to the retina, showing new blood vessels.
Intraocular Pressure (IOP)
Intraocular Pressure (IOP)
Pressure within the eye, usually measured between 10-21 mmHg.
Angle Closure Glaucoma
Angle Closure Glaucoma
Signup and view all the flashcards
Pilocarpine (cholinergic)
Pilocarpine (cholinergic)
Signup and view all the flashcards
Beta-blockers (e.g., timolol)
Beta-blockers (e.g., timolol)
Signup and view all the flashcards
Causes of glaucoma
Causes of glaucoma
Signup and view all the flashcards
Normal angle
Normal angle
Signup and view all the flashcards
Study Notes
Sensory Challenges - Chapters 60 & 61 (4th Ed.)
- Chapter 60: Assessment and Management of Patients with Eye and Vision Disorders
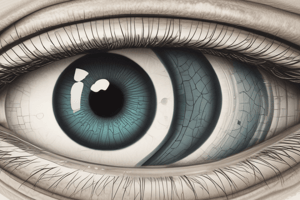
- External Structures of the Eye: Includes the cornea, sclera, conjunctiva, iris, pupil, lacrimal gland, upper and lower lids, canthus, caruncle, lacrimal sac, and nasolacrimal duct. Detailed anatomical diagram provided.
- Cross-Section of the Eye: Inner eye structures such as the retina, choroid, sclera, optic nerve, central retinal arteries and veins, macular area, vitreous body, and structures related to lens and ciliary body are shown in a detailed cross-section diagram.
- Assessment and Evaluation of Vision: Provides details on ocular history (using Chart 60-1), Visual acuity testing (using Snellen chart), recording 20/20 vision, and finger counting/hand motion as visual acuity options.
- Examination of External Structures: Includes assessment for irritation, inflammation, discharge from the eye, eyelids, sclera, pupils and pupillary response (in a dark room), eye gaze and position, and extraocular movements. Specific terms like ptosis (drooping eyelid) and nystagmus (oscillating movement of eyeball) are referenced.
- Diagnostic Evaluation: Includes ophthalmoscopy (direct/indirect), slit-lamp examination (for cataracts), color vision testing, Amsler grid (for macular degeneration), ultrasonography (for tumours/retinal detachments), optical coherence tomography (high-resolution images/cross-sections), color fundus photography, laser scanning (images of the eye's surface), indocyanine green angiography (blood flow to the choroid), tonometry (intraocular pressure), gonioscopy (angle of anterior chamber), and perimetry (evaluating field of vision).
Impaired Vision
- Refractive Errors: Include emmetropia (normal vision), myopia (near-sightedness), hyperopia (far-sightedness), and astigmatism (distortion due to irregular cornea curvature).
- Low Vision and Blindness: Differentiates low vision (BCVA of 20/40 or worse, requiring assistive devices) from legal blindness (BCVA of 20/400 or worse, or field of vision 20 degrees or less).
- Assessment of Low Vision: Emphasizes history taking (distance/near vision, visual field, contrast sensitivity, glare, color perception, and refraction), using specialized charts, and thorough nursing assessments of functional ability, coping mechanisms, and emotional/social well-being.
- Management of Low Vision: Includes strategies like adjusting placement of items in a room, clock method for arranging objects, communication strategies (details available in Chart 60-3), collaboration with specialists (low vision, occupational therapist or others), assistive methods (braille or sign language), and service animals.
Glaucoma
- Description: Groups of eye conditions where optic nerve damage is linked to increased intraocular pressure (IOP) caused by aqueous humor congestion.
- Prevalence: A major cause of blindness in adults. Its incidence rises with age.
- Risk factors: Includes thin cornea, African heritage, prolonged steroid use, family history, cardiovascular disease, migraines, myopia and eye trauma. (Chart 60-5)
- Pathophysiology: Imbalance in aqueous humor production and drainage resulting in buildup and increased pressure in the eye.
- Types (based on angle between iris and cornea): Includes open-angle (usually bilateral, including normal-tension and ocular hypertension) and closed-angle (pupillary block, acute, subacute and chronic angle closure) glaucoma. (See Table 60-4).
- Clinical Manifestations: Characterized by the "silent thief" aspect, where patients are unaware of the condition until vision loss is advanced, including blurriness, halos, difficulty focusing with dim light, peripheral vision loss, aches and discomfort around the eyes/headache.
- Diagnostic Findings: Tonometry (IOP measurement), Gonioscopy (examination of anterior chamber angle), and Perimetry (field of vision assessment).
- Treatment: Aim to control IOP within a safe range to prevent further nerve damage. Often involves pharmacologic therapy, surgical interventions like laser trabeculoplasty, laser iridotomy, filtering procedures, trabeculectomy, and drainage implants. Details on medications see Table 60-5
Cataracts
- Definition: An opacity or cloudiness of the lens of the eye.
- Prevalence: Common cause of disability in older adults in Canada.
- Risk factors: Age, toxic factors, nutrition deficiencies, dehydration, and trauma to the eye are listed. (Chart 60-8).
- Manifestations: Painless, blurry vision, sensitivity to glare, reduced visual acuity, myopic shift, astigmatism, diplopia (double vision), and color shifts (like brunescens, to yellow-brown).
- Diagnostic findings: Decreased visual acuity, opacity of the lens via ophthalmoscopy, slit lamp, or direct inspection.
- Surgical management: Performed as outpatient and with local anesthesia. Includes intracapsular cataract extraction (ICCE), extracapsular cataract extraction (ECCE), and phacoemulsification (ultrasound) with lens replacement.
- Nursing management: Preoperative care (eye drops, medications), postoperative care (following clinical pathways and home care checklists, Chart 60-9), providing instructions, and monitoring for complications(like changes in vision, pain, drainage).
Other retinal disorders
-
Retinal detachment: Separation of sensory retina from pigment epithelium (RPE). Manifestations include flashes of light, floaters, and a shadow or curtain spreading across the vision of one eye. Diagnostics include assessing visual acuity, using indirect ophthalmoscopy, slit-lamp biomicroscopy, stereo fundus photography, fluorescein angiography (blood flow views), tomography and ultrasound. Surgical treatment (e.g., scleral buckle, pneumatic retinopexy, and pars plana vitrectomy).
-
Retinal vein/artery occlusion: Results from atherosclerosis, cardiac valvular issues, venous stasis, hypertension, increased blood viscosity, diabetes mellitus, glaucoma, and aging. Symptoms include loss of vision or decrease in visual acuity—often a sudden onset.
-
Age-related Macular Degeneration (AMD): The leading cause of vision loss in Canada. Characterized by slow degeneration of retinal layers in the macular area. Two main types: dry (non-exudative) and wet (exudative); the later has a rapid onset. CNV (Choroidal neovascularization) is a key characteristic of the wet AMD.
Ophthalmic Medications
- Ophthalmic Medications: Ability of the eye to absorb medications limited by conjunctival sac size, corneal barriers, tear/blink/drainage, and blood-ocular barriers. Intraocular injections or systemic medications sometimes needed to provide high concentration for treatment in certain eye structures. Topical medications (drops/ointments) are common due to fewest side effects and allow for self-administration. Details on specific types of topical anesthetics, mydriatics/cycloplegics, antibiotics, anti-infectives, and topical steroids.
Guidelines for Instilling Medications
- Stepwise instructions for proper medication instillation (drops, ointments) of eye medications, emphasizing cleanliness, correct positioning, and post-instillation eye care procedures.
Safety Measures and Teaching
- Importance of patient teaching, particularly post-eye surgery.
- Specific teaching includes complications sign/symptoms (e.g., increased IOP, infection); safety measures for visual impairment at home and hospital.
Chapter 61: Assessment and Management of Patients with Hearing and Balance Disorders
- Anatomy of the Ear (outer, middle and inner ear): Diagrams depicting the auricle, external auditory canal, tympanic membrane, ossicles (malleus, incus, stapes), cochlea, semicircular canals, and Eustachian tube.
- Anatomy of the inner ear: Detailed illustration of the bony labyrinth, and membranous labyrinth components like the semicircular canals, utricle, saccule, cochlea, and organ of Corti.
- Bone vs. Air Conduction: Diagrams outlining the pathways of sound transmission via air and bone (through the skull). Discusses the concept of “lag” time.
- Assessment: Details on assessing external ear, otoscopic examination, gross auditory acuity, whisper test, Weber (unilateral hearing loss), and Rinne tests (air and bone conductive hearing loss).
- Diagnostic Evaluation: Methods such as audiometry, tympanogram, auditory brain stem response (ABR), electronystagmography (ENG), platform posturography, sinusoidal harmonic acceleration, and middle ear endoscopy.
- Hearing Loss: (Type, causes, risk factors) and classifications such as conductive, sensorineural, mixed, and functional hearing loss, as well risk factors like, increased age and noise exposure.
- Manifestations: Defining tinnitus, difficulty interpreting sounds in groups, turning up TV volume, and the progressive nature of hearing loss in many cases.
- Communication Guidelines: Key steps for interacting with hearing-impaired individuals. (See Chart 61-4).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.