Podcast
Questions and Answers
What is a primary characteristic of emphysema?
What is a primary characteristic of emphysema?
- Inflammation of the airways
- Formation of fibrous tissue in the lungs
- Increased mucus production in the bronchi
- Permanent enlargement of air spaces (correct)
Which type of emphysema is most strongly associated with alpha-1 antitrypsin deficiency?
Which type of emphysema is most strongly associated with alpha-1 antitrypsin deficiency?
- Panacinar emphysema (correct)
- Distal acinar emphysema
- Centriacinar emphysema
- Chronic bronchitis
In which area of the lungs is centriacinar emphysema most commonly found?
In which area of the lungs is centriacinar emphysema most commonly found?
- Central acini
- Lower lobes
- Distal alveoli
- Apical segments of the upper lobes (correct)
What is a significant risk factor for developing centriacinar emphysema?
What is a significant risk factor for developing centriacinar emphysema?
Which statement about distal acinar emphysema is correct?
Which statement about distal acinar emphysema is correct?
How does panacinar emphysema differ from centriacinar emphysema in terms of distribution?
How does panacinar emphysema differ from centriacinar emphysema in terms of distribution?
What is the common association found with distal acinar emphysema?
What is the common association found with distal acinar emphysema?
What is the underlying problem in emphysema that affects gas exchange?
What is the underlying problem in emphysema that affects gas exchange?
What is the primary effect of interleukin-8 released by airway epithelial cells?
What is the primary effect of interleukin-8 released by airway epithelial cells?
In chronic bronchitis, what is a key histological change observed in the airway epithelium?
In chronic bronchitis, what is a key histological change observed in the airway epithelium?
What is the Reid Index and its values for chronic bronchitis?
What is the Reid Index and its values for chronic bronchitis?
Which of the following symptoms is characteristic of chronic bronchitis-related complications?
Which of the following symptoms is characteristic of chronic bronchitis-related complications?
What differentiates extrinsic from intrinsic asthma?
What differentiates extrinsic from intrinsic asthma?
How does chronic hypoxemia affect red blood cell production in patients with chronic bronchitis?
How does chronic hypoxemia affect red blood cell production in patients with chronic bronchitis?
Which type of asthma is most commonly associated with a family history of atopy?
Which type of asthma is most commonly associated with a family history of atopy?
What is a common feature of asthma regardless of its type?
What is a common feature of asthma regardless of its type?
What is the primary cause of airway remodeling in asthma?
What is the primary cause of airway remodeling in asthma?
What is the role of eotaxin in the late-phase reaction of asthma?
What is the role of eotaxin in the late-phase reaction of asthma?
Which of the following is NOT a characteristic of bronchiectasis?
Which of the following is NOT a characteristic of bronchiectasis?
Which of the following changes occurs during airway remodeling in asthma?
Which of the following changes occurs during airway remodeling in asthma?
What types of crystals are associated with eosinophils in asthma?
What types of crystals are associated with eosinophils in asthma?
What is a key characteristic of emphysema's morphology?
What is a key characteristic of emphysema's morphology?
Which factor is primarily responsible for the protease-anti-protease imbalance in emphysema?
Which factor is primarily responsible for the protease-anti-protease imbalance in emphysema?
What type of emphysema is characterized by the formation of large subpleural bullae?
What type of emphysema is characterized by the formation of large subpleural bullae?
Which inflammatory mediator is significantly increased due to cigarette smoke exposure?
Which inflammatory mediator is significantly increased due to cigarette smoke exposure?
What is the primary pathological process in chronic bronchitis?
What is the primary pathological process in chronic bronchitis?
What condition is defined by a productive cough lasting for at least 3 months in two consecutive years?
What condition is defined by a productive cough lasting for at least 3 months in two consecutive years?
Which of the following contributes to oxidative stress in the lungs?
Which of the following contributes to oxidative stress in the lungs?
What is commonly absent in the inflammatory response associated with chronic bronchitis?
What is commonly absent in the inflammatory response associated with chronic bronchitis?
What is a symptom commonly associated with both atopic and non-atopic asthma?
What is a symptom commonly associated with both atopic and non-atopic asthma?
Which of the following is a common trigger for non-atopic asthma?
Which of the following is a common trigger for non-atopic asthma?
What type of asthma is primarily triggered by pharmacologic agents?
What type of asthma is primarily triggered by pharmacologic agents?
Which interleukin is responsible for promoting IgE antibody production in asthma?
Which interleukin is responsible for promoting IgE antibody production in asthma?
What characterizes the early-phase reaction in asthma?
What characterizes the early-phase reaction in asthma?
Which of the following is a critical mediator released during asthma's inflammatory response?
Which of the following is a critical mediator released during asthma's inflammatory response?
What is the likely involvement of aspirin in drug-induced asthma?
What is the likely involvement of aspirin in drug-induced asthma?
In occupational asthma, symptoms typically appear after what kind of exposure?
In occupational asthma, symptoms typically appear after what kind of exposure?
Flashcards
Emphysema
Emphysema
A lung disease causing the permanent enlargement of air sacs and destruction of their walls, decreasing gas exchange.
Centriacinar Emphysema
Centriacinar Emphysema
Emphysema affecting the central parts of air sacs, often seen in smokers, in the upper lungs.
Panacinar Emphysema
Panacinar Emphysema
Emphysema uniformly affecting all parts of air sacs, often linked to a genetic condition (alpha-1 antitrypsin deficiency).
Distal Acinar Emphysema
Distal Acinar Emphysema
Signup and view all the flashcards
Respiratory Bronchioles
Respiratory Bronchioles
Signup and view all the flashcards
Alveolar Duct
Alveolar Duct
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Alpha-1 Antitrypsin Deficiency
Alpha-1 Antitrypsin Deficiency
Signup and view all the flashcards
Emphysema pathogenesis
Emphysema pathogenesis
Signup and view all the flashcards
Protease-Anti-Protease Imbalance
Protease-Anti-Protease Imbalance
Signup and view all the flashcards
Oxidative Stress in Emphysema
Oxidative Stress in Emphysema
Signup and view all the flashcards
Inflammatory Cells' Role in Emphysema
Inflammatory Cells' Role in Emphysema
Signup and view all the flashcards
Bullous Emphysema
Bullous Emphysema
Signup and view all the flashcards
Chronic Bronchitis Definition
Chronic Bronchitis Definition
Signup and view all the flashcards
Chronic Bronchitis Hypertrophy
Chronic Bronchitis Hypertrophy
Signup and view all the flashcards
Normal Bronchiole Structure
Normal Bronchiole Structure
Signup and view all the flashcards
Inflammatory Mediators
Inflammatory Mediators
Signup and view all the flashcards
Cytokine Mediators
Cytokine Mediators
Signup and view all the flashcards
Reid Index
Reid Index
Signup and view all the flashcards
Chronic Bronchitis
Chronic Bronchitis
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
Atopic Asthma
Atopic Asthma
Signup and view all the flashcards
Blue Bloaters
Blue Bloaters
Signup and view all the flashcards
Secondary Polycythemia Vera
Secondary Polycythemia Vera
Signup and view all the flashcards
Increased mucus production
Increased mucus production
Signup and view all the flashcards
Vasodilation
Vasodilation
Signup and view all the flashcards
Eotaxin
Eotaxin
Signup and view all the flashcards
Airway Remodeling in Asthma
Airway Remodeling in Asthma
Signup and view all the flashcards
Bronchiectasis
Bronchiectasis
Signup and view all the flashcards
Non-Atopic Asthma
Non-Atopic Asthma
Signup and view all the flashcards
Drug-Induced Asthma
Drug-Induced Asthma
Signup and view all the flashcards
Occupational Asthma
Occupational Asthma
Signup and view all the flashcards
IL-4 in Asthma
IL-4 in Asthma
Signup and view all the flashcards
IL-5 in Asthma
IL-5 in Asthma
Signup and view all the flashcards
IL-13 in Asthma
IL-13 in Asthma
Signup and view all the flashcards
Early-Phase Asthma Reaction
Early-Phase Asthma Reaction
Signup and view all the flashcards
Study Notes
Obstructive Lung Diseases
- Obstructive lung diseases involve four main disorders: emphysema, chronic bronchitis, asthma, and bronchiectasis.
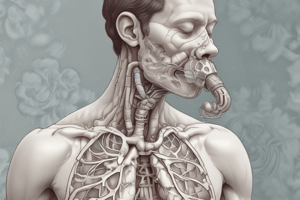
Emphysema
- Emphysema is a lung condition characterized by the permanent enlargement of air spaces distal to terminal bronchioles, along with destruction of their walls.
- This occurs without significant fibrosis, reducing the lungs' ability to exchange gases effectively and causing breathing problems.
- Emphysema's damage includes destruction of alveolar air sacs and loss of elastic recoil.
Types of Emphysema
- Centriacinar (centrilobular): Primarily affects central parts of the acini (respiratory bronchioles), sparing distal alveoli. Lesions are more common in the upper lobes, especially apical areas. Frequently occurs in cigarette smokers and associated with chronic bronchitis. Can also affect distal acinus in severe cases.
- Panacinar (panlobular): Uniform enlargement of acini, affecting respiratory bronchioles, alveolar ducts, and terminal alveoli. Predominantly impacts the lower lung zones. Associated with alpha-1 antitrypsin deficiency.
- Distal acinar (paraseptal): Predominantly affects distal parts of the acini, with normal proximal portions. More prominent around the pleura, lobular connective tissue septa, and margins of lobules. Often occurs near fibrotic, scarred, or atelectatic areas and is more severe in the upper half of the lungs. Associated with spontaneous pneumothorax.
Chronic Bronchitis
- A long-term condition defined by a productive cough lasting at least three months in two consecutive years.
- Commonly affects smokers and those in polluted environments (e.g., sulfur dioxide, nitrogen dioxide).
- Key feature: Hypertrophy of mucous glands and increased goblet cells leading to mucus hypersecretion in large airways of the lungs.
Asthma
- A chronic inflammatory disorder of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night and/or early morning.
- Involves reversible airway obstruction, increased mucus production, and inflammation primarily involving eosinophils and mast cells.
Bronchiectasis
- Permanent dilation of bronchi and bronchioles caused by destruction of smooth muscle and elastic tissue.
- Typically linked to chronic necrotizing infections.
- It's not a primary disorder, but a secondary result from persistent infection or obstruction caused by various conditions.
- Especially affects the lower lobes bilaterally, targeting vertical air passages.
Pathology Notes
- Reid Index: A measurement of the thickness of the glands and walls of the bronchi to determine the presence of chronic bronchitis. A Reid index above 40% indicates chronic bronchitis.
- Blue Bloater: A clinical presentation of chronic bronchitis, characterized by cyanosis and hypoxia due to poor oxygenation and carbon dioxide retention, often with increased body weight and puffiness.
- Status Asthmaticus: A severe, life-threatening episode of asthma, often requiring emergency medical intervention. In this state, the patient's lungs appear hyper-inflated, distended or distended with air, despite outward appearance.
- Atopic Asthma: The most common type, characterized by IgE-mediated hypersensitivity to allergens. Triggers include allergens (dust, pollen, animal dander, food) and respiratory infections. Begins consistently during childhood and often has a family history.
- Non-Atopic Asthma: Asthma without evidence of allergen sensitization. Triggers include viral respiratory infections and inhaled pollutants. May be triggered by viral inflammation within respiratory mucosa, reducing the threshold to irritants.
- Occupational Asthma: Asthma triggered by exposure to specific antigens in the workplace. Common causes include fumes (e.g., epoxy resins), organic dusts (e.g., wood, cotton), and chemicals (e.g., toluene).
- Airway Remodeling: Structural changes in bronchial walls as a result of repeated inflammation, including thickening of walls, increased smooth muscle and collagen deposition, mucus hypersecretion, epithelial cell changes, airway narrowing, and vascular changes.
- Morphology:
-Curschmann Spirals: Dense, tenacious mucus plugs with shed epithelium whorls in asthma and often associated with airway plugging.- Charcot-Leyden Crystals: Crystalloids made up of eosinophil protein galectin-10, found in asthma.
- Bronchioles/Bronchi Dilation: Dilation occurring in bronchiectasis, stretching up to four times normal diameter and often visible reaching to the pleural surface.
Pathogenesis
- Emphysema: Protease-anti-protease imbalance, oxidative stress, and inflammatory cells are key factors. Smoking and genetic conditions can contribute.
- Chronic Bronchitis: Environmental irritants cause inflammation, with macrophages, neutrophils, and lymphocytes infiltrating the airways. Inflammatory mediators, and cytokine mediators exacerbate the issue.
- Asthma: Activation of Type 2 Helper T (TH2) cells triggers cytokine production leading to IgE antibody production, mast cell activation and release of mediators like histamine, leukotrienes, and prostaglandins. Eosinophil activation and mucus production further exacerbate the narrowing of the airways. -Bronchiectasis: Chronic inflammation and infection damage the smooth muscle and elastic tissue of bronchi and bronchioles, causing lasting dilation of the affected airways. Infection is the leading cause.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.