Podcast
Questions and Answers
What are potential adverse reactions to Neostigmine?
What are potential adverse reactions to Neostigmine?
- Abdominal cramping (correct)
- Headaches
- Weight gain
- Vision impairment
Which consequence is NOT a risk associated with the improper use of neuromuscular blocking agents?
Which consequence is NOT a risk associated with the improper use of neuromuscular blocking agents?
- Respiratory arrest
- Death
- Nausea (correct)
- Permanent injury
Which strategies are recommended to ensure the safe use of neuromuscular blocking agents?
Which strategies are recommended to ensure the safe use of neuromuscular blocking agents?
- Prolong dosing intervals
- Proper product labeling (correct)
- Increase storage temperatures
- Limit patient interaction
What characterizes the positive symptoms of spasticity?
What characterizes the positive symptoms of spasticity?
Which of the following is NOT a recommended practice for pharmacy handling of neuromuscular blocking agents?
Which of the following is NOT a recommended practice for pharmacy handling of neuromuscular blocking agents?
What is the primary neurotransmitter involved in neuromuscular transmission?
What is the primary neurotransmitter involved in neuromuscular transmission?
Which medical condition is commonly associated with increased muscle spasticity?
Which medical condition is commonly associated with increased muscle spasticity?
What type of muscle relaxant acts predominantly at the peripheral level?
What type of muscle relaxant acts predominantly at the peripheral level?
Which of the following describes a mechanism of action for neuromuscular blocking drugs?
Which of the following describes a mechanism of action for neuromuscular blocking drugs?
What is a potential adverse effect of neuromuscular blocking agents?
What is a potential adverse effect of neuromuscular blocking agents?
Which drug classification includes agents primarily used to relieve persistent muscle spasms?
Which drug classification includes agents primarily used to relieve persistent muscle spasms?
How do central-acting muscle relaxants achieve their effect?
How do central-acting muscle relaxants achieve their effect?
What is the purpose of acetylcholinesterase in the context of neuromuscular transmission?
What is the purpose of acetylcholinesterase in the context of neuromuscular transmission?
What is one of the phases in the pathophysiology of spasticity?
What is one of the phases in the pathophysiology of spasticity?
Which of the following conditions is NOT typically associated with spasticity?
Which of the following conditions is NOT typically associated with spasticity?
What generally occurs after the shock period following a spinal cord injury?
What generally occurs after the shock period following a spinal cord injury?
What is a likely cause of spasticity in conditions like stroke or cerebral palsy?
What is a likely cause of spasticity in conditions like stroke or cerebral palsy?
What does damage to myelinated nerves in multiple sclerosis lead to regarding spasticity?
What does damage to myelinated nerves in multiple sclerosis lead to regarding spasticity?
What effect does increased calcium have on acetylcholine (ACh) release in muscle interactions?
What effect does increased calcium have on acetylcholine (ACh) release in muscle interactions?
Which of the following statements about neuromuscular blocking agents is true?
Which of the following statements about neuromuscular blocking agents is true?
What is the primary mechanism of action for peripheral-acting muscle relaxants?
What is the primary mechanism of action for peripheral-acting muscle relaxants?
What is a common side effect associated with botulinum toxin type A?
What is a common side effect associated with botulinum toxin type A?
How do depolarizing blocking agents affect acetylcholine receptors?
How do depolarizing blocking agents affect acetylcholine receptors?
What is the role of anticholinesterase drugs in neuromuscular blockade reversal?
What is the role of anticholinesterase drugs in neuromuscular blockade reversal?
Which agent is an example of a nondepolarizing muscle relaxant?
Which agent is an example of a nondepolarizing muscle relaxant?
What is one of the primary uses of peripheral-acting skeletal muscle relaxants?
What is one of the primary uses of peripheral-acting skeletal muscle relaxants?
What adverse effect can result from the use of high doses of ethanol?
What adverse effect can result from the use of high doses of ethanol?
Which physiological event occurs when the endplate potential exceeds 15 mV?
Which physiological event occurs when the endplate potential exceeds 15 mV?
What is the primary role of acetylcholine in muscle function?
What is the primary role of acetylcholine in muscle function?
What happens to muscle fibers in the case of spinal cord injury?
What happens to muscle fibers in the case of spinal cord injury?
How do GABAergic drugs like baclofen exert their effects?
How do GABAergic drugs like baclofen exert their effects?
What is a common adverse reaction associated with tizanidine?
What is a common adverse reaction associated with tizanidine?
What neurotransmitter is associated with hyperpolarization and inhibition of action potentials?
What neurotransmitter is associated with hyperpolarization and inhibition of action potentials?
What effect do botulinum toxins have at the neuromuscular junction?
What effect do botulinum toxins have at the neuromuscular junction?
What is the mechanism of action of dantrolene?
What is the mechanism of action of dantrolene?
Glycine is primarily known as which type of neurotransmitter?
Glycine is primarily known as which type of neurotransmitter?
Which drug binds to GABA receptors to decrease nerve excitability?
Which drug binds to GABA receptors to decrease nerve excitability?
What is a potential effect of using central-acting muscle relaxants?
What is a potential effect of using central-acting muscle relaxants?
What condition can be triggered by the use of succinylcholine or anesthetic inhalation gases?
What condition can be triggered by the use of succinylcholine or anesthetic inhalation gases?
What is a key function of glutamate in the nervous system?
What is a key function of glutamate in the nervous system?
What neurotransmitter is associated with increased endplate potential?
What neurotransmitter is associated with increased endplate potential?
Flashcards
Neuromuscular Blockade
Neuromuscular Blockade
A temporary interruption of the communication between nerves and muscles, preventing muscle contraction.
Muscle Spasms
Muscle Spasms
Involuntary and sometimes painful muscle contractions.
Neuromuscular Junction
Neuromuscular Junction
The specialized synapse (connection) between a motor neuron and a muscle fiber where communication happens.
Acetylcholine (ACh)
Acetylcholine (ACh)
Signup and view all the flashcards
Acetylcholinesterase
Acetylcholinesterase
Signup and view all the flashcards
Spasticity
Spasticity
Signup and view all the flashcards
Motor Neuron Endplate
Motor Neuron Endplate
Signup and view all the flashcards
Peripheral Nerves
Peripheral Nerves
Signup and view all the flashcards
Neostigmine
Neostigmine
Signup and view all the flashcards
Pyridostigmine (Mestinon®)
Pyridostigmine (Mestinon®)
Signup and view all the flashcards
Neuromuscular Blocking Agents (NMBAs)
Neuromuscular Blocking Agents (NMBAs)
Signup and view all the flashcards
What are the effects of spasticity?
What are the effects of spasticity?
Signup and view all the flashcards
Calcium's effect on ACh release
Calcium's effect on ACh release
Signup and view all the flashcards
Muscle relaxation (drugs)
Muscle relaxation (drugs)
Signup and view all the flashcards
Neuromuscular blocking agents
Neuromuscular blocking agents
Signup and view all the flashcards
Botulinum toxin
Botulinum toxin
Signup and view all the flashcards
Peripheral-acting muscle relaxants
Peripheral-acting muscle relaxants
Signup and view all the flashcards
Nondepolarizing agents
Nondepolarizing agents
Signup and view all the flashcards
Depolarizing agents
Depolarizing agents
Signup and view all the flashcards
Anticholinesterase drugs
Anticholinesterase drugs
Signup and view all the flashcards
Spinal Cord Injury & Spasticity
Spinal Cord Injury & Spasticity
Signup and view all the flashcards
Spasticity: Decreased Reflex Excitability
Spasticity: Decreased Reflex Excitability
Signup and view all the flashcards
Spasticity: Stages
Spasticity: Stages
Signup and view all the flashcards
Stroke & Spasticity
Stroke & Spasticity
Signup and view all the flashcards
Multiple Sclerosis & Spasticity
Multiple Sclerosis & Spasticity
Signup and view all the flashcards
What happens when muscle fibers atrophy?
What happens when muscle fibers atrophy?
Signup and view all the flashcards
What causes desensitization of motor nerves in ALS?
What causes desensitization of motor nerves in ALS?
Signup and view all the flashcards
What is the role of GABA in spasticity?
What is the role of GABA in spasticity?
Signup and view all the flashcards
How does glycine contribute to spasticity?
How does glycine contribute to spasticity?
Signup and view all the flashcards
What is the role of glutamate in spasticity?
What is the role of glutamate in spasticity?
Signup and view all the flashcards
Botulinum Toxins A and B: How do they work?
Botulinum Toxins A and B: How do they work?
Signup and view all the flashcards
What is the mechanism of action for dantrolene?
What is the mechanism of action for dantrolene?
Signup and view all the flashcards
What are GABAergic drugs and how do they work?
What are GABAergic drugs and how do they work?
Signup and view all the flashcards
How do alpha2-adrenergic drugs work?
How do alpha2-adrenergic drugs work?
Signup and view all the flashcards
What are skeletal muscle relaxants used for?
What are skeletal muscle relaxants used for?
Signup and view all the flashcards
What are some common adverse reactions to skeletal muscle relaxants?
What are some common adverse reactions to skeletal muscle relaxants?
Signup and view all the flashcards
What is the MOA of baclofen?
What is the MOA of baclofen?
Signup and view all the flashcards
What is the MOA of diazepam?
What is the MOA of diazepam?
Signup and view all the flashcards
What is the MOA of tizanidine?
What is the MOA of tizanidine?
Signup and view all the flashcards
Study Notes
Neuromuscular Blockade and Muscle Spasms
-
Neuromuscular blockade learning points include terminology, neuromuscular transmission, spasticity-causing medical conditions, neuromuscular blocking drugs, and skeletal muscle relaxation mechanism.
-
Muscle spasms treatment also includes drug uses, reversal mechanisms, safe pharmacy management, look-alike/sound-alike issues, and warnings.
Key Terms
- Acetylcholinesterase
- Anaphylactic shock
- Botulinum toxin
- Central-acting muscle relaxants
- Clonus
- Depolarizing neuromuscular blockers
- Endotracheal intubation
- End plate
- Neuromuscular junction
- Nondepolarizing competitive blockers
- Peripheral-acting muscle relaxants
- Sarcomere
- Sole plate
- Spasticity
- Amyotrophic lateral sclerosis (ALS)
- Cerebral palsy
- Multiple sclerosis
- Tetanus
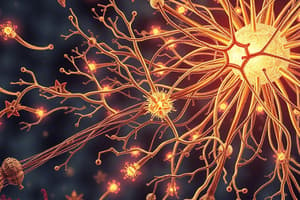
Overview of Neuromuscular Function
- Skeletal muscle contraction results from communication between peripheral nerves and muscles.
- Acetylcholine (ACh) carries messages between nerve cells and muscle cells.
- Acetylcholine-filled vesicles are found in the motor neuron's endplate.
- Calcium is released to cause ACh release, and drugs that affect ACh release/depletion cause muscle relaxation.
Overview of Neuromuscular Blockade
- ACh binds to nicotinic receptor sites on the muscle soleplate.
- ACh binding triggers sodium, calcium, and potassium ion influx, increasing endplate potential.
- Endplate potential exceeding 15 mV produces an action potential, leading to muscle contraction.
Overview of Botulinum Toxin
- Found naturally (e.g., botulinum toxin, black widow spider venom)
- Decreases acetylcholine release.
- Used to temporarily remove wrinkles, treat excessive sweating, uncontrollable blinking, or migraines.
Skeletal Muscle Relaxants
- Categorized by site of action and mechanism of action.
- Two primary mechanisms involve central nervous system depression or blockade of nerve transmission between the motor endplate and skeletal muscle receptors.
Peripheral-Acting Skeletal Muscle Relaxants
- Includes non-depolarizing (e.g., atracurium, cisatracurium, pancuronium, rocuronium) and depolarizing (e.g., succinylcholine) agents.
- Used in surgery, general anesthesia, and intubation.
- Improper use can be dangerous, potentially fatal.
Botulinum Toxin Type A Uses
- Temporary wrinkle removal
- Excessive sweating control
- Treating uncontrollable blinking
- Treating migraines (not FDA approved for cerebral palsy related spasticity)
Neuromuscular Blocking Agent Adverse Reactions
- Allergic reactions (rash, redness, bronchospasm, laryngospasm, anaphylaxis)
- Muscle pain
- Respiratory depression
- Cardiac arrest
- Injection site reactions (itching, burning)
- Hypotension
- Vasodilation
- Tachycardia or bradycardia
- Pulmonary edema
- Hyperkalemia (depolarizing agents)
- Additional botulinum toxin-type A adverse reactions include droopy eyelids, headaches, nausea, flu-like symptoms, and redness.
Reversal of Neuromuscular Blockade
- Anticholinesterase drugs (neostigmine, pyridostigmine) inhibit ACh esterase, increasing acetylcholine.
- Adverse reactions include salivation, muscle twitching, weakness, abdominal cramping, nausea, increased bronchial secretions, and difficulty breathing.
Strategies for Safe Use of Neuromuscular Blocking Agents
- High-alert classification due to potential for harm from improper use.
- Risks include permanent injury, respiratory arrest, and death.
Recommendations for Pharmacy Practice with NMBAS
- Product selection, storage, and access limitations are crucial.
- Warning labels are necessary.
- Proper ordering and dispensing practices are essential.
Overview of Spasticity
- It is a debilitating motor disorder affecting 12 million worldwide.
- Interferes with daily living, inhibits walking, causes fatigue/stiffness, and disrupts sleep.
- Positive symptoms include increased muscle tone, exaggerated tendon reflexes, and hyperexcitable stretch reflexes.
- Negative symptoms include muscle weakness and reduced endurance.
Pathophysiology of Spasticity
- Four phases: decreased muscle contractility, increased muscle tone, decreased reflex excitability and stiff/contracted muscles are involved
Conditions That Produce Spasticity
- Spinal cord injury, stroke, cerebral palsy, amyotrophic lateral sclerosis (ALS), multiple sclerosis, and muscle strain lead to spasticity.
Spinal Cord Injury
- Initial paralysis.
- Loss of tendon reflexes below the injury level.
- Increased muscle tone, exaggerated tendon jerks, and involuntary muscle spasms.
- Stronger reflex connections develop.
Amyotrophic Lateral Sclerosis (ALS)
- Damage to upper motor neurons causes decreased acetylcholine release.
- Acetylcholine desensitization of motor nerves leads to muscle weakness and cell death.
Neurotransmitters Involved in Spasticity
- Acetylcholine, y-aminobutyric acid (GABA), glycine, and glutamate play roles in spasticity.
Drugs Used to Treat Spasticity
- Peripheral-acting drugs (e.g., botulinum toxins, dantrolene) and central-acting drugs (e.g., baclofen, diazepam, tizanidine) treat spasticity.
Drugs Used to Treat Muscle Strain
- Drugs like cyclobenzaprine, methocarbamol, orphenadrine, and chlorzoxazone+acetaminophen+codeine are used.
- Central acting drugs are often used.
Adverse Reactions and Warnings for Muscle Strain Treatments
- Dizziness, drowsiness, blurred vision, and urine discoloration are possible adverse reactions.
- Warnings include impairments to driving, alcohol avoidance, possible habit formation, and the need to take with food.
Additional Look-Alike Drug Warnings
- Be aware of look-alike/sound-alike drug names (e.g., baclofen and Bactroban, Lioresal and Lotensin, diazepam and Ditropan, tizanidine and nizatidine, and cyproheptadine and cyclobenzaprine) to avoid errors.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.