Podcast
Questions and Answers
Significant impairments in memory and executive function after a closed head injury decline overall IQ performance.
Significant impairments in memory and executive function after a closed head injury decline overall IQ performance.
False (B)
Personality changes such as irritability and apathy are common after severe injuries involving the temporal lobe.
Personality changes such as irritability and apathy are common after severe injuries involving the temporal lobe.
False (B)
Depression and anxiety are reported to be very common after brain damage, with widely varying prevalence estimates.
Depression and anxiety are reported to be very common after brain damage, with widely varying prevalence estimates.
True (A)
Head injuries have been linked to a higher occurrence of violence and suicide.
Head injuries have been linked to a higher occurrence of violence and suicide.
Post-head-injury mania is a very common occurrence following brain damage.
Post-head-injury mania is a very common occurrence following brain damage.
Transient psychosis symptoms are frequently observed immediately after head injury.
Transient psychosis symptoms are frequently observed immediately after head injury.
The prevalence of depression after a stroke is about 30% and can remain stable for over a decade.
The prevalence of depression after a stroke is about 30% and can remain stable for over a decade.
Personality changes following a stroke include increased flexibility in coping with problems.
Personality changes following a stroke include increased flexibility in coping with problems.
Post-stroke depression has no effect on the quality of life of stroke survivors.
Post-stroke depression has no effect on the quality of life of stroke survivors.
Antidepressants can enhance recovery after a stroke independent of their mood effects.
Antidepressants can enhance recovery after a stroke independent of their mood effects.
Emotional stress is suspected to precipitate a subarachnoid haemorrhage in some cases.
Emotional stress is suspected to precipitate a subarachnoid haemorrhage in some cases.
The risk of developing depression is confirmed to be greater following a left frontal stroke.
The risk of developing depression is confirmed to be greater following a left frontal stroke.
Lability of mood is a symptom that can occur after a stroke.
Lability of mood is a symptom that can occur after a stroke.
Cognitive impairment, personality change, and anxiety are uncommon in survivors of subarachnoid haemorrhage.
Cognitive impairment, personality change, and anxiety are uncommon in survivors of subarachnoid haemorrhage.
Cognitive deficits after a stroke are primarily due to a single stroke event.
Cognitive deficits after a stroke are primarily due to a single stroke event.
Patients recovering from a stroke may experience spontaneous laughter and crying that does not match their mood.
Patients recovering from a stroke may experience spontaneous laughter and crying that does not match their mood.
Subdural haematomas commonly occur without any history of trauma.
Subdural haematomas commonly occur without any history of trauma.
The severity of non-penetrating head injury can be accurately measured by the duration of post-traumatic amnesia.
The severity of non-penetrating head injury can be accurately measured by the duration of post-traumatic amnesia.
A PTA of less than one week usually predicts a poor outcome for returning to work.
A PTA of less than one week usually predicts a poor outcome for returning to work.
Post-concussional syndrome affects 30-50% of patients after mild head injury.
Post-concussional syndrome affects 30-50% of patients after mild head injury.
Delusional misidentification can occur after severe head injury.
Delusional misidentification can occur after severe head injury.
A normal MRI scan guarantees that there is no brain damage after a head injury.
A normal MRI scan guarantees that there is no brain damage after a head injury.
The risk of suicide increases threefold after a head injury.
The risk of suicide increases threefold after a head injury.
Symptoms of post-concussional syndrome include only physical issues like headaches and dizziness.
Symptoms of post-concussional syndrome include only physical issues like headaches and dizziness.
Deposition of β-amyloid is linked to the development of Alzheimer's disease following head injury.
Deposition of β-amyloid is linked to the development of Alzheimer's disease following head injury.
Chronic psychological effects of head injury are solely determined by the severity of the physical injury.
Chronic psychological effects of head injury are solely determined by the severity of the physical injury.
Study Notes
Subdural Haematoma
- Common in elderly patients, especially those with a history of alcoholism, often lacks a significant history of head trauma.
- Acute cases may result in coma, fluctuating consciousness, hemiparesis, and oculomotor signs.
- Chronic syndromes often present as headaches, poor concentration, vague physical complaints, fluctuating consciousness, with fewer neurological signs.
- Important to consider as a cause of accelerated decline in patients with neurodegenerative dementia.
- Treatment involves surgical evacuation, which can reverse symptoms.
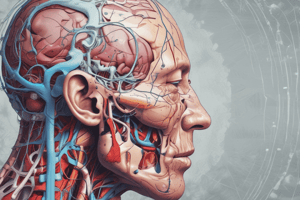
Head Injury
- Two primary groups of patients:
- Small group with severe cognitive and behavioral sequelae.
- Larger group experiencing emotional symptoms and personality changes.
- Severity of closed head injury measured by the duration of post-traumatic amnesia (PTA):
- PTA less than one week correlates with better outcomes like returning to work.
- PTA over one month often leads to inability to return to work.
- Retrograde amnesia (loss of prior memory) is less indicative of outcomes.
- MRI scans help assess brain injury extent, but normal results don't rule out damage.
- Closed head injuries mainly arise from acceleration and deceleration forces.
- Loss of consciousness for seconds often due to disrupted cholinergic transmission in the brainstem.
- Severe injuries can show hemorrhagic damage and diffuse axonal injury in white matter, affecting coma duration.
- Additional complications include extradural and subdural hemorrhages and anoxia.
- Link between head injury and Alzheimer’s disease may involve β-amyloid deposition; apoE4 genotype increases death risk and cognitive deficits post-injury.
Acute Psychological Effects
- Delirium phase may follow severe injury and awakening from coma; prolonged delirium can cause confabulation.
- Occasional delusional misidentification or reduplicative paramnesia may occur, such as mistaking staff for friends.
- Agitation and disinhibition, including sexual behaviors, may last from days to weeks.
Chronic Psychological Effects
- Neurological and cognitive deficits result from both primary and secondary damage.
- Long-term outcomes influenced by premorbid personality, social support, and compensation issues.
- Post-traumatic epilepsy can complicate recovery; suicide risk increases threefold.
Post-Concussional Syndrome
- Post-injury, 15-30% of patients experience post-concussional syndrome with symptoms like anxiety, depression, irritability, headache, fatigue, and insomnia.
Stroke
Cognitive Deficits
- Strokes can lead to vascular dementia and result in various neuropsychiatric issues.
- Presenting symptoms include hemiparesis and dysphasia as neurological emergencies.
Personality Change
- Common behavioral changes include irritability, apathy, mood lability, and emotional instability, often mirroring residual physical symptoms.
- Emotional displays may be incongruent with mood; antidepressants can aid treatment.
Post-Stroke Depression
- Depression occurs in about 30% of stroke survivors, with cumulative incidence reaching 45% within five years.
- Risk factors include the extent of impairment in daily activities, cognitive deficits, and a history of depression.
- Associated with reduced quality of life and increased disability; SSRIs are effective for managing symptoms but need cautious use due to potential side effects.
Subarachnoid Haemorrhage
- Survivors face cognitive impairment, personality changes, anxiety, and depression, with poor long-term outcomes and significant psychosocial issues.
Lasting Cognitive Impairment
- Vulnerability of frontal and temporal lobes leads to neuropsychological deficits, particularly in memory and executive functions.
Personality Change
- Commonly occurs post-severe injury with frontal lobe damage; symptoms include irritability, apathy, and impulsivity issues.
- Increased rates of violence and suicide linked to head injury; management requires significant social support and rehabilitation resources.
Depression and Emotional Disorder
- Depression, anxiety, and emotional lability are frequent following brain damage, though estimates of prevalence vary widely.
- Post-head-injury mania is less prevalent compared to other emotional disorders.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the significant cognitive and psychological effects of closed head injuries, including memory impairments, personality changes, and the prevalence of depression and anxiety. Additionally, it highlights the associations between brain damage and increased violence, suicide, and transient psychotic symptoms.