Podcast
Questions and Answers
What is the main role of the ventral/anterior spinothalamic tract?
What is the main role of the ventral/anterior spinothalamic tract?
- Conduction of pressure and crude touch (correct)
- Regulation of muscle tone
- Conduction of pain sensations
- Coordination of fine motor skills
What condition is characterized by paraplegia in flexion during the late stage of disease progression?
What condition is characterized by paraplegia in flexion during the late stage of disease progression?
- Ventral spinal artery occlusion
- Brown Sequard Syndrome
- Extrapyramidal tract involvement (correct)
- Corticospinal tract involvement
In Brown Sequard Syndrome, what sensory loss occurs on the ipsilateral side?
In Brown Sequard Syndrome, what sensory loss occurs on the ipsilateral side?
- Crude touch sensation
- Motor weakness (correct)
- Pain and temperature sensation
- Vibration sense
Which artery supplies blood to the anterior part of the spinal cord?
Which artery supplies blood to the anterior part of the spinal cord?
The corticospinal tract primarily controls which type of motor action?
The corticospinal tract primarily controls which type of motor action?
What is the most common cause of acute transverse myelitis?
What is the most common cause of acute transverse myelitis?
Which of the following are clinical features associated with acute transverse myelitis?
Which of the following are clinical features associated with acute transverse myelitis?
What does the term 'definite sensory level' in acute transverse myelitis refer to?
What does the term 'definite sensory level' in acute transverse myelitis refer to?
Which dermatomes correspond to the level of the nipples?
Which dermatomes correspond to the level of the nipples?
In acute transverse myelitis, brisk reflexes below the level of involvement may indicate which of the following?
In acute transverse myelitis, brisk reflexes below the level of involvement may indicate which of the following?
What is the primary difference in the onset of symptoms between conus medullaris and cauda equina syndrome?
What is the primary difference in the onset of symptoms between conus medullaris and cauda equina syndrome?
Which of the following accurately describes the sensory loss characteristic of cauda equina syndrome?
Which of the following accurately describes the sensory loss characteristic of cauda equina syndrome?
What is a key symptom of epiconus involving knee and ankle reflexes?
What is a key symptom of epiconus involving knee and ankle reflexes?
Which cause of non-compressive myelopathy is associated with vitamin deficiency?
Which cause of non-compressive myelopathy is associated with vitamin deficiency?
Which statement correctly distinguishes the deep tendon reflexes (DTR) in conus medullaris?
Which statement correctly distinguishes the deep tendon reflexes (DTR) in conus medullaris?
What characterizes the pathology of the Lateral Corticospinal Tract?
What characterizes the pathology of the Lateral Corticospinal Tract?
Which of the following describes the action of the Rubrospinal Tract?
Which of the following describes the action of the Rubrospinal Tract?
In the case of a lesion below the Rubrospinal Tract, what is the effect on the lower limb posture?
In the case of a lesion below the Rubrospinal Tract, what is the effect on the lower limb posture?
In decerebrate rigidity, what is the general posture of the upper limb?
In decerebrate rigidity, what is the general posture of the upper limb?
Which of the following tracts is described as the only extrapyramidal pathway located in the lateral column?
Which of the following tracts is described as the only extrapyramidal pathway located in the lateral column?
What is a major cause of extradural compressive myelopathy?
What is a major cause of extradural compressive myelopathy?
Which condition is associated with intramedullary compressive myelopathy?
Which condition is associated with intramedullary compressive myelopathy?
What type of compressive myelopathy most commonly results from intervertebral disc pathology?
What type of compressive myelopathy most commonly results from intervertebral disc pathology?
Which of the following tumors is NOT typically associated with intradural compressive myelopathy?
Which of the following tumors is NOT typically associated with intradural compressive myelopathy?
Which symptom is most commonly associated with myelopathy?
Which symptom is most commonly associated with myelopathy?
What characterizes root pain/girdle pain?
What characterizes root pain/girdle pain?
What exacerbates Lhermitte sign?
What exacerbates Lhermitte sign?
What condition is indicated by increased CSF protein levels?
What condition is indicated by increased CSF protein levels?
Which pathway is characterized by dissociative sensory loss?
Which pathway is characterized by dissociative sensory loss?
Which symptom indicates early lower motor neuron findings?
Which symptom indicates early lower motor neuron findings?
Which spinal tracts are affected in cases of sacral sparing?
Which spinal tracts are affected in cases of sacral sparing?
What type of pain is described as constant and dull, originating from within?
What type of pain is described as constant and dull, originating from within?
What type of compression is a likely cause for root pain/girdle pain?
What type of compression is a likely cause for root pain/girdle pain?
What area of the spinal cord is primarily supplied by the anterior spinal artery?
What area of the spinal cord is primarily supplied by the anterior spinal artery?
Which artery is the largest radicular artery supplying the lower half of the spinal cord?
Which artery is the largest radicular artery supplying the lower half of the spinal cord?
Which of the following conditions is associated with anterior spinal artery thrombosis?
Which of the following conditions is associated with anterior spinal artery thrombosis?
What is the primary function of radicular arteries?
What is the primary function of radicular arteries?
What effect does the ligamentum denticulatum have on the spinal cord?
What effect does the ligamentum denticulatum have on the spinal cord?
Which of the following symptoms is NOT associated with Guillain-Barré Syndrome (GBS)?
Which of the following symptoms is NOT associated with Guillain-Barré Syndrome (GBS)?
Which investigation finding would most likely indicate Subacute Combined Degeneration (SACD)?
Which investigation finding would most likely indicate Subacute Combined Degeneration (SACD)?
What is the first sign of sensory loss in Subacute Combined Degeneration (SACD)?
What is the first sign of sensory loss in Subacute Combined Degeneration (SACD)?
In the context of plasma exchange for Guillain-Barré Syndrome, which of the following conditions would be an indication for the procedure?
In the context of plasma exchange for Guillain-Barré Syndrome, which of the following conditions would be an indication for the procedure?
What complication may arise if Subacute Combined Degeneration (SACD) is left untreated?
What complication may arise if Subacute Combined Degeneration (SACD) is left untreated?
What abnormal finding indicates a positive Beevor's sign?
What abnormal finding indicates a positive Beevor's sign?
Which symptoms are characteristic of intramedullary compression compared to extramedullary compression?
Which symptoms are characteristic of intramedullary compression compared to extramedullary compression?
Which of the following findings is consistent with upper motor neuron lesions below the level of involvement?
Which of the following findings is consistent with upper motor neuron lesions below the level of involvement?
How does sacral sparing differ between intramedullary and extramedullary compression?
How does sacral sparing differ between intramedullary and extramedullary compression?
What reflex findings would be expected below a lesion affecting the upper limb at T1?
What reflex findings would be expected below a lesion affecting the upper limb at T1?
Chronic back pain associated with neurogenic claudication is typically:
Chronic back pain associated with neurogenic claudication is typically:
Which sensory symptoms are associated with neurogenic claudication?
Which sensory symptoms are associated with neurogenic claudication?
Which of the following statements accurately describes vascular claudication?
Which of the following statements accurately describes vascular claudication?
What reflex finding is typically observed in individuals with neurogenic claudication?
What reflex finding is typically observed in individuals with neurogenic claudication?
Which of the following is a potential complication in cases of intramedullary compression?
Which of the following is a potential complication in cases of intramedullary compression?
How does the bicycle test differ between neurogenic claudication and vascular claudication?
How does the bicycle test differ between neurogenic claudication and vascular claudication?
In relation to the pattern of weakness, what is a common finding in neurogenic claudication?
In relation to the pattern of weakness, what is a common finding in neurogenic claudication?
What characteristic of muscle power is observed in upper limbs for individuals with lower limb compression?
What characteristic of muscle power is observed in upper limbs for individuals with lower limb compression?
Flashcards are hidden until you start studying
Study Notes
Ventral/Anterior Tracts
- Ascending tracts carry sensations of pressure and crude touch
- Descending tracts include Extrapyramidal and Corticospinal tracts
- Extrapyramidal tracts involve the Vestibulospinal, Ventral reticulospinal, and Tectospinal tracts
- Corticospinal tracts control extension
Pathology of Descending Tracts
- Early stage: Paraplegia in extension due to corticospinal tract involvement
- Late stage: Paraplegia in flexion due to progression of disease and involvement of extrapyramidal tracts
Brown Sequard Syndrome
- Hemisection of the spinal cord can result in:
- Ipsilateral loss of posterior column sensation and motor weakness
- Contralateral loss of lateral spinothalamic sensation (pain and temperature)
Blood Supply of Spinal Cord
- Arteries:
- Superior cerebellar artery, Middle cerebellar artery, Posterior inferior cerebellar artery, Posterior cerebral artery
- Basilar artery, Vertebral arteries
- Ascending cervical, Intercostal, Lumbar arteries
- Anterior spinal artery, Posterior spinal artery, Dorsal radicular artery, Ventral radicular artery
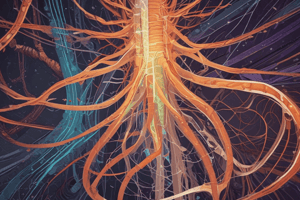
Cross-section of Spinal Cord
- Sensory and motor pathways:
- Fasciculus cuneatus
- Fasciculus gracilis
- Dorsal root
- Dorsal spinocerebellar tract
- Ventral spinocerebellar tract
- Lateral spinothalamic tract
- Ventral spinothalamic tract
- Anterior horn
- Lateral corticospinal tract (pyramidal tract)
- Rubrospinal tract
- Lateral reticulospinal tract
- Vestibulospinal tract
- Ventral reticulospinal tract
- Tectospinal tract
Root pain/girdle pain vs Lhermitte sign
- Root pain/girdle pain:
- Brief shock-like pain along a distribution, initially unilateral, then bilateral
- Exacerbated by coughing/Valsalva maneuver
- Lhermitte sign:
- Shooting pain along the spinal cord, extending to the sacrum
- Exacerbated by flexion of the neck
Useful for Localization
- Funicular pain/tract pain: Constant, dull aching pain from within
- Suspended sensory loss: Loss or crossing over of sensory tract fibers above and below the level of the spinal cord involvement; sensation below the level is considered normal
- Dissociative sensory loss: Loss of spinothalamic tract sensation with intact posterior column
- Early LMN findings (Lower Motor Neuron): When lesions reach the anterior horn cells
- Spinothalamic tract fibers: These fibers are organized centrally to peripherally (e.g., cervical, thoracic, lumbar, sacral) and therefore, sacral sparing may be present when involvement is intramedullary. Bowel and bladder fibers are also centrally located, indicating early involvement. Corticospinal tracts are peripherally located, implying late involvement.
Other observations
- CSF protein: Increased protein levels might suggest root involvement
- Intramedullary: Extension of the pathology can damage sympathetic fibers in the cervical level, causing Horner's syndrome
Acute Transverse Myelitis
- Rapid onset full thickness/segmented monophasic inflammation of the spinal cord (myelitis: Inflammation of cord)
- Demyelinating disease which can affect variable number of segments
- Causes:
- Post infectious (most common)
- Vaccination
- Multiple sclerosis
- Sarcoidosis
- Paraneoplastic
- Neuromyelitis optica
- Behçet's disease
Levels of Principal Dermatomes
- C5: Clavicles
- C5,6,7: Lateral parts of upper limbs
- C8, T1: Medial sides of upper limbs
- C6: Thumb
- C6,7,8: Hand
- C8: Ring and little fingers
- C8, T4: Level of nipples
- T10: Level of umbilicus
- T12: Inguinal or groin regions
- L1,2,3,4: Anterior and inner surfaces of lower limbs
- L4,5, S1: Foot
- L4: Medial side of great toe
- S1, 2, L5: Posterior and outer surfaces of lower limbs
- S1: Lateral margin of foot and little toe
- S2,3,4: Perineum
Clinical Features
- Paresthesia: Beginning in the feet and extending upward to trunk
- Back pain and paraesthesia: Evolve into spastic weakness
- Peak reached: Within 4 hours to 21 days
- Plateau phase: Mean duration 1 week
- Definite sensory level:
- Band-like constriction at the level
- Complete loss of all sensory modalities below the level
- If half thickness involvement: U/L posterior column loss + C/L spinothalamic loss
- Motor weakness: Below the level of involvement (Paraparesis: Symmetrical/asymmetrical)
- Significant bowel/bladder involvement: Urinary retention
- Brisk reflexes: Below the level of involvement
Descending Tracts
- Lateral Corticospinal Tract:
- Location: Pre-central gyrus
- Pathology:
- Extramedullary lesion: Early involvement
- Hemisection of spinal cord: 1/L motor weakness
- Rubrospinal Tract:
- Only extrapyramidal pathway in lateral column
- Action: Flexion of upper limb
- Pathology:
- Lesion w.r.t Red nucleus of mid Brain
- Decorticate rigidity: Upper limb is flexed; Lower limb is stretched
- Decerebrate rigidity: Upper limb is stretched; Lower limb is stretched
Spinal Cord Tracts
- Spino-cerebellar
- Spinotectal
- Spinoreticular
- Spino-olivary
Effects of Lesions on Spinal Cord Tracts
| Trait | Lesion Above | Lesion Below |
|---|---|---|
| Rubrospinal Tract | Spared | Affected |
| Posture - Upper Limb | Flexed | Extended |
| Posture - Lower Limb | Extended | Extended |
Conus Medullaris v/s Cauda Equina
| Feature | Conus medullaris | Cauda equina |
|---|---|---|
| Involvement | B/L S3 → C inside spinal cord | Asymmetrical La → C roots |
| Onset | Sudden onset | Insidious |
| Root pain | ||
| Sensory loss | ||
| Dissociated sensory loss | ||
| Motor | ||
| Deep tendon reflex (DTR) | Normal (Anal & bulbocavernous reflexes lost) | |
| Bladder | U/L in leg, thigh, bladder | |
| Saddle distribution | + | Saddle/any part of LL |
| Weakness | No weakness | Weakness & wasting of LL muscles |
| Loss of knee & ankle jerk | Loss of knee & ankle jerk (Depends on level) | |
| Bowel | ||
| Sexual |
Epiconus
- Involves: L4, L5, S1, S2
- Lower limb weakness: Hip flexion/adduction spared
- Knee & ankle jerk lost
- Sensory loss: Lower limb (Thigh spared)
- Bladder: UMN
Non Compressive Myelopathy
- Causes:
- Vascular & demyelinating:
- Vascular: Anterior spinal artery (ASA) thrombosis
- Demyelinating: Multiple sclerosis (ms), Neuromyelitis optica (NMO)
- Inherited: Friedreich's ataxia
- Toxin: Arsenic
- Autoimmune: Sarcoid
- Metabolic:
- Sub acute combined degeneration: Posterolateral cord syndrome, D/t vitamin B12 deficiency
- Differential diagnosis: Vitamin E deficiency, Copper deficiency
- Sub acute combined degeneration: Posterolateral cord syndrome, D/t vitamin B12 deficiency
- Other factors: HIV, HTLV-I
- Vascular & demyelinating:
Anatomy of Spinal Cord
- Origin: Vertebral Artery
- Branches:
- 2 posterior spinal arteries: Posterior 1/3rd of spinal cord
- 1 Anterior spinal artery: Anterior 2/3rd of spinal cord
- Radicular arteries (Feeder arteries):
- Reinforce blood supply at each level (Lower cervical segment and below)
- Artery of Adamkiewicz/Arteria radicularis magna (Largest radicular artery):
- Originates near T8-T12 vertebrae → Supplies entire lower half spinal cord
- T4-T5 Spinal Segments: Less radicular arteries → Increased risk of ischemia
- Arteria Vasocorona: Circumferential anastomotic channels around spinal cord.(Corticospinal tract in watershed area → myelopathy).
Pathology
- Anterior Spinal artery thrombosis:
- Onset: Acute
- Associated with: Generalized atherosclerosis
- Sparing of posterior column
- Posterior spinal artery injury: Traumatic accidents
Ligamentum denticulatum
- Extension of pia mater attaching spinal cord on duramater
- Compressive myelopathy: Denticulate ligament compresses corticospinal tract
### Compressive Myelopathy
- Chronic course
- Types & causes:
- Intramedullary:
- Cause:
- Tumors: Ependymoma, Oligodendroglioma, Medulloblastoma
- Expansion of cavity: Syringomyelia
- Cause:
- Extramedullary:
- Intradural:
- Cause: Neurofibroma, Meningioma
- Extradural (most common):
- Cause:
- Lesion of vertebrae: Fracture, Infection (TB, syphilis), Pyogenic abscess
- Metastasis (Prostate & ovary cancer)
- Disc pathology: IVDP (most common)
- Aneurysm of aorta
- Cause:
- Intradural:
- Intramedullary:
Clinical Features
- Chronic back pain: Moderate to severe intensity, worse in upright posture (neurogenic claudication; canal diameter decreases in standing/erect posture). Relief from bending (like cycling)
- Tingling, numbness, paresthesia: Typically on both lower limbs, depending on the affected spinal level
- Weakness in lower limbs
- Band-like sensation (hyperesthesia): At the level of involvement (e.g., umbilicus if T10 level is involved)
Neurogenic Claudication vs Vascular Claudication
| Feature | Neurogenic Claudication | Vascular Claudication |
|---|---|---|
| Walking distance | Variable | Fixed |
| Relieved on | Sitting/bending | Standing |
| Worsened on | Walking/standing (erect posture) | Walking |
| Bicycle test | Painless | Painful |
| Pulse | Negative | Positive (Painful) |
| Weakness | Present | Absent |
| Back pain | Occasionally | Rarely |
| Pain character | Numbness, aching, proximal to distal | Cramping; Distal to proximal |
Examination Findings
- Higher mental function (HMF), cranial nerves (CN): Normal
- Motor:
- Upper limb: Compression below T1 → power intact (5/5)
- Lower limb: Reduced power
- Sensory:
- Upper limb: Compression below T1 → sensation intact
- Lower limb:
- Spinothalamic tract loss
- Posterior column loss
- Reflexes:
- Lower limb: Exaggerated (knee jerk, ankle jerk)
- Plantar: Extensor
- Bowel & bladder involvement: Possible in cases of intramedullary compression
Differentiating Points from GBS
- GBS:
- Progressive lower limb weakness (Proximal > distal)
- Ascending paralysis
- Areflexia
- Normal sensory examination
- No band-like sensation (definite sensory level)
- No bladder symptoms
Investigations
- MRI T2 of spine: Hyperintensities at the level
- CSF: Pleocytosis (>10 cells), ↑ IgG index
Treatment
- No response
- High-dose methylprednisolone: (500-1000 mg IV in 100ml NS over 1 hour)
- Indications for plasma exchange:
- Inability to walk
- Markedly impaired autonomic function
- Sensory loss in lower extremities
SUBACUTE COMBINED DEGENERATION (SACD)
- AKA posterolateral cord syndrome (White matter)
- D/t vitamin B12 deficiency
Progression of disease
- Posterior tract: Posterior column sensations lost. Tingling, paresthesia of distal extremity: First symptom
- Vibration sense lost first: First sign
- Fine touch and proprioception lost
- Sensory ataxia, gait abnormality
- Lateral tract:
- Spinothalamic tract
- Corticospinal tract: umN findings (Babinski: extensor plantar)
- Motor manifestations
- Large fibre neuropathy: Reflex lost (Knee jerk, ankle jerk), glove & stocking neuropathy
- If not treated: Complication: Dementia, optic atrophy
Level Localization
- LMN findings: Wasting atrophy, band-like sensation, hyperesthesia, hypesthesia, hypoalgesia. At the level of the lesion
- UMN findings: Below the level of lesion (Superficial reflexes lost, deep reflexes exaggerated)
- Upper limb normal: Lesion below T1 (Above the level of involvement: spared)
- Sensory symptoms: In both lower limbs
- Weakness: Of both lower limbs
- Beevor's sign positive: Lesion below T10
- Once the spinal segment is localized: Localize compression to the corresponding vertebral segment
- Reflex level: Best localizing value
Beevor's Sign
- Procedure: Ask the patient to get up from a supine position
- Principle:
- Normal: Upper (T7-T9) and lower (T9-T12) abdominal muscles contract together. No deviation of the umbilicus
- Weakness of lower abdomen: Upper abdominal muscle contraction pulls umbilicus above (Beevor sign positive)
### Extramedullary vs Intramedullary Compression
| Damage | Intramedullary (Centrifugal, Centre → Periphery of spinal cord) | Extramedullary (Centripetal, Periphery → Centre) |
|---|---|---|
| Pain | + | Root pain |
| Dissociative sensory loss | + | - |
| Suspended sensory loss | + | - |
| Sacral sparing | + | - |
| Trophic changes (D/t pain & temperature loss) | + | + |
| Pyramidal signs (UMN) | Late | Early |
| LMN signs | Early | Late |
| Bowel/bladder | Early | Late |
| Spinal deformity | - | - |
| Spinal tenderness | - | + |
| CSF protein | - | + |
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.