Podcast
Questions and Answers
Which of the following best describes the pain associated with neuralgia?
Which of the following best describes the pain associated with neuralgia?
- A constant, dull ache that worsens with activity.
- Sudden attacks of excruciating, 'lightning-like' or throbbing pain. (correct)
- Mild tingling sensation with occasional sharp twinges.
- A deep, burning pain that is present at all times.
Which of the following is a key characteristic of neuralgia that distinguishes it from other types of nerve pain?
Which of the following is a key characteristic of neuralgia that distinguishes it from other types of nerve pain?
- Objective signs of nerve damage are always present.
- The pain is typically bilateral and symmetrical.
- It primarily affects motor function rather than sensory.
- The absence of objective signs or structural damage to the nerve. (correct)
A patient reports experiencing sharp, stabbing pain along their rib cage that is triggered by a light touch. Based on the information provided, which condition is most likely?
A patient reports experiencing sharp, stabbing pain along their rib cage that is triggered by a light touch. Based on the information provided, which condition is most likely?
- Costochondritis
- Intercostal neuralgia (correct)
- Muscular strain
- Myofascial pain syndrome
Which of the following conditions is most commonly associated with causing intercostal neuralgia?
Which of the following conditions is most commonly associated with causing intercostal neuralgia?
A patient reports experiencing sudden, sharp, lightning-like pain along their ribs. Which of the following signs is most indicative of intercostal neuralgia, rather than another musculoskeletal issue?
A patient reports experiencing sudden, sharp, lightning-like pain along their ribs. Which of the following signs is most indicative of intercostal neuralgia, rather than another musculoskeletal issue?
Which of the following scenarios would be LEAST likely to be associated with the development of neuralgia?
Which of the following scenarios would be LEAST likely to be associated with the development of neuralgia?
A massage therapist is treating a patient with suspected trigeminal neuralgia. What is the MOST important precaution they should take during the session?
A massage therapist is treating a patient with suspected trigeminal neuralgia. What is the MOST important precaution they should take during the session?
During the acute phase of intercostal neuralgia, what is the MOST appropriate treatment strategy?
During the acute phase of intercostal neuralgia, what is the MOST appropriate treatment strategy?
Before considering any direct treatment near the trigger zone of a patient with intercostal neuralgia, what is the MOST important step to take?
Before considering any direct treatment near the trigger zone of a patient with intercostal neuralgia, what is the MOST important step to take?
Which of the following is the MOST accurate description of a trigger zone in the context of neuralgia?
Which of the following is the MOST accurate description of a trigger zone in the context of neuralgia?
A patient with intercostal neuralgia presents with pain that is exacerbated by deep breathing and twisting movements. Which anatomical structures are MOST likely involved in the patient's pain experience?
A patient with intercostal neuralgia presents with pain that is exacerbated by deep breathing and twisting movements. Which anatomical structures are MOST likely involved in the patient's pain experience?
Which of the following treatment approaches should be prioritized LAST when addressing intercostal neuralgia?
Which of the following treatment approaches should be prioritized LAST when addressing intercostal neuralgia?
A patient describes their neuralgia pain as feeling like "electric shocks" along the affected nerve pathway. What aspect of the nerve's function is MOST likely disrupted in this type of pain?
A patient describes their neuralgia pain as feeling like "electric shocks" along the affected nerve pathway. What aspect of the nerve's function is MOST likely disrupted in this type of pain?
What type of home care is MOST suitable for a patient recovering from intercostal neuralgia?
What type of home care is MOST suitable for a patient recovering from intercostal neuralgia?
Which of the following describes the correct palpation technique for identifying the supraorbital branch of the trigeminal nerve?
Which of the following describes the correct palpation technique for identifying the supraorbital branch of the trigeminal nerve?
A patient with intercostal neuralgia is experiencing muscle spasms in the thoracic region. When is rib springing contraindicated?
A patient with intercostal neuralgia is experiencing muscle spasms in the thoracic region. When is rib springing contraindicated?
A patient reports numbness in the cheek and lower lip. Which branch of the trigeminal nerve is MOST likely involved?
A patient reports numbness in the cheek and lower lip. Which branch of the trigeminal nerve is MOST likely involved?
During history taking, which question would be MOST important to ask a patient suspected of having intercostal neuralgia?
During history taking, which question would be MOST important to ask a patient suspected of having intercostal neuralgia?
When assessing the motor function of the trigeminal nerve, which action would NOT be evaluated?
When assessing the motor function of the trigeminal nerve, which action would NOT be evaluated?
During palpation, where should you place your fingers to locate the mental branch of the trigeminal nerve?
During palpation, where should you place your fingers to locate the mental branch of the trigeminal nerve?
A patient presents with sharp, stabbing pain along the cheek and jaw. Which condition involving the trigeminal nerve is the MOST likely cause?
A patient presents with sharp, stabbing pain along the cheek and jaw. Which condition involving the trigeminal nerve is the MOST likely cause?
In addition to the muscles of mastication, which other muscle's function is related to the trigeminal nerve?
In addition to the muscles of mastication, which other muscle's function is related to the trigeminal nerve?
What is the primary sensory function associated with the trigeminal nerve?
What is the primary sensory function associated with the trigeminal nerve?
To palpate the zygomaticotemporal branch of the trigeminal nerve, where should you position your fingers?
To palpate the zygomaticotemporal branch of the trigeminal nerve, where should you position your fingers?
During a massage for a client with Bell's Palsy, which of the following precautions is MOST crucial to prevent further nerve irritation?
During a massage for a client with Bell's Palsy, which of the following precautions is MOST crucial to prevent further nerve irritation?
When treating the unaffected side of a client with Bell's Palsy, what is the MOST important direction of pressure and stroking to consider?
When treating the unaffected side of a client with Bell's Palsy, what is the MOST important direction of pressure and stroking to consider?
Which hydrotherapy application is BEST suited to stimulate facial muscles and reduce edema on the affected side of a client with Bell's Palsy?
Which hydrotherapy application is BEST suited to stimulate facial muscles and reduce edema on the affected side of a client with Bell's Palsy?
Why is it important to 'block' and protect affected tissues during the treatment of Bell's Palsy?
Why is it important to 'block' and protect affected tissues during the treatment of Bell's Palsy?
A client with Bell's Palsy is experiencing difficulty closing their affected eye. What is the MOST appropriate recommendation for ADLs (Activities of Daily Living)?
A client with Bell's Palsy is experiencing difficulty closing their affected eye. What is the MOST appropriate recommendation for ADLs (Activities of Daily Living)?
During the treatment of a client with Bell's Palsy, the therapist cues and assists with facial expressions. What is the primary goal of this technique?
During the treatment of a client with Bell's Palsy, the therapist cues and assists with facial expressions. What is the primary goal of this technique?
A patient presents with unilateral facial paralysis, including the inability to wrinkle their forehead and close their eye. Which condition is MOST likely indicated by these symptoms?
A patient presents with unilateral facial paralysis, including the inability to wrinkle their forehead and close their eye. Which condition is MOST likely indicated by these symptoms?
A massage therapist is treating a client with Bell's Palsy. The client reports increased sensitivity around the stylomastoid foramen on the affected side. Which modification to the treatment setup is MOST appropriate?
A massage therapist is treating a client with Bell's Palsy. The client reports increased sensitivity around the stylomastoid foramen on the affected side. Which modification to the treatment setup is MOST appropriate?
Which of the following cranial nerves is directly implicated in the motor deficits observed in Bell's Palsy?
Which of the following cranial nerves is directly implicated in the motor deficits observed in Bell's Palsy?
A client with Bell's Palsy is performing facial exercises at home. Which of the following exercises would be MOST appropriate?
A client with Bell's Palsy is performing facial exercises at home. Which of the following exercises would be MOST appropriate?
A pregnant woman in her third trimester reports sudden onset of unilateral facial paralysis. Besides Bell's Palsy, what other systemic condition should be considered as a potential contributing factor?
A pregnant woman in her third trimester reports sudden onset of unilateral facial paralysis. Besides Bell's Palsy, what other systemic condition should be considered as a potential contributing factor?
Which physical assessment finding would be LEAST expected in a patient diagnosed with Bell's Palsy affecting the right side of their face?
Which physical assessment finding would be LEAST expected in a patient diagnosed with Bell's Palsy affecting the right side of their face?
A patient with Bell's Palsy reports heightened sensitivity to low-pitched sounds. What is the MOST likely explanation for this symptom?
A patient with Bell's Palsy reports heightened sensitivity to low-pitched sounds. What is the MOST likely explanation for this symptom?
During an assessment of a patient suspected of having Bell's Palsy, which of the following instructions would be MOST helpful in differentiating the condition from a stroke?
During an assessment of a patient suspected of having Bell's Palsy, which of the following instructions would be MOST helpful in differentiating the condition from a stroke?
A massage therapist is treating a patient with Bell's Palsy. Which of the following considerations is MOST important before initiating treatment?
A massage therapist is treating a patient with Bell's Palsy. Which of the following considerations is MOST important before initiating treatment?
A patient with Bell's Palsy reports difficulty with eating and drinking. What is the MOST likely underlying cause of this issue?
A patient with Bell's Palsy reports difficulty with eating and drinking. What is the MOST likely underlying cause of this issue?
A patient reports experiencing sensory loss over the forehead and upper nasal cavity. Which branch of the trigeminal nerve is most likely affected?
A patient reports experiencing sensory loss over the forehead and upper nasal cavity. Which branch of the trigeminal nerve is most likely affected?
Which area is innervated by the maxillary division (V2) of the trigeminal nerve?
Which area is innervated by the maxillary division (V2) of the trigeminal nerve?
Loss of hearing due to paralysis of tensor tympani is a possible manifestation of trigeminal neuralgia. Paralysis of teonsor tympani affects which branch of trigeminal nerve?
Loss of hearing due to paralysis of tensor tympani is a possible manifestation of trigeminal neuralgia. Paralysis of teonsor tympani affects which branch of trigeminal nerve?
A patient presents with 'nerve-pain' but no visible structural damage. This presentation aligns with which condition?
A patient presents with 'nerve-pain' but no visible structural damage. This presentation aligns with which condition?
During an assessment, a patient reports experiencing sharp, 'lightning-like' pain fits in the face with no apparent cause. Which condition is most indicated?
During an assessment, a patient reports experiencing sharp, 'lightning-like' pain fits in the face with no apparent cause. Which condition is most indicated?
Which of the following questions is MOST relevant when taking the history of a patient with suspected trigeminal neuralgia?
Which of the following questions is MOST relevant when taking the history of a patient with suspected trigeminal neuralgia?
A therapist is treating a patient with diagnosed trigeminal neuralgia. During the session, which action is MOST appropriate?
A therapist is treating a patient with diagnosed trigeminal neuralgia. During the session, which action is MOST appropriate?
Which symptom is LEAST likely to be associated with trigeminal neuralgia?
Which symptom is LEAST likely to be associated with trigeminal neuralgia?
Flashcards
Post-herpes zoster
Post-herpes zoster
Reactivation of the virus from the dorsal root ganglion at a time of immune suppression.
Intercostal Neuralgia trigger zone
Intercostal Neuralgia trigger zone
Distribution of the affected segment at the spine and laterally along the intercostal space.
Key sign of Intercostal Neuralgia
Key sign of Intercostal Neuralgia
Horrible, lightning-like pain that comes on in fits for little to no reason
Manifestation of Shingles
Manifestation of Shingles
Signup and view all the flashcards
Precaution for Intercostal Neuralgia
Precaution for Intercostal Neuralgia
Signup and view all the flashcards
Treatment during acute phase
Treatment during acute phase
Signup and view all the flashcards
Neuralgia
Neuralgia
Signup and view all the flashcards
Relaxation focus
Relaxation focus
Signup and view all the flashcards
Touching the trigger zone
Touching the trigger zone
Signup and view all the flashcards
Neuralgia Pain
Neuralgia Pain
Signup and view all the flashcards
Common Neuralgia Sites
Common Neuralgia Sites
Signup and view all the flashcards
Trigger zone
Trigger zone
Signup and view all the flashcards
Causes of Neuralgia
Causes of Neuralgia
Signup and view all the flashcards
Neuralgia Precaution
Neuralgia Precaution
Signup and view all the flashcards
Neuralgia Pain Duration
Neuralgia Pain Duration
Signup and view all the flashcards
Trigger Zone Stimuli
Trigger Zone Stimuli
Signup and view all the flashcards
Trigeminal Nerve (CN V) Branches
Trigeminal Nerve (CN V) Branches
Signup and view all the flashcards
Ophthalmic Branch Cutaneous Branches
Ophthalmic Branch Cutaneous Branches
Signup and view all the flashcards
Supraorbital Branch Palpation Point
Supraorbital Branch Palpation Point
Signup and view all the flashcards
Supratrochlear Branch Palpation
Supratrochlear Branch Palpation
Signup and view all the flashcards
Infraorbital Branch Palpation
Infraorbital Branch Palpation
Signup and view all the flashcards
Mental Branch Palpation
Mental Branch Palpation
Signup and view all the flashcards
Zygomaticotemporal Branch Palpation
Zygomaticotemporal Branch Palpation
Signup and view all the flashcards
Trigeminal Nerve (CN V) Motor Functions
Trigeminal Nerve (CN V) Motor Functions
Signup and view all the flashcards
Bell's Palsy: Eye Closure
Bell's Palsy: Eye Closure
Signup and view all the flashcards
Bell's Palsy: Facial Droop
Bell's Palsy: Facial Droop
Signup and view all the flashcards
Bell's Palsy: Facial Appearance
Bell's Palsy: Facial Appearance
Signup and view all the flashcards
Stroke: Forehead Wrinkles & Eye Closure
Stroke: Forehead Wrinkles & Eye Closure
Signup and view all the flashcards
Bell's Palsy: Observation
Bell's Palsy: Observation
Signup and view all the flashcards
Facial Expression AROM/RROM
Facial Expression AROM/RROM
Signup and view all the flashcards
Bell's Palsy: Risk Factors
Bell's Palsy: Risk Factors
Signup and view all the flashcards
Bell's Palsy: Sensory Changes
Bell's Palsy: Sensory Changes
Signup and view all the flashcards
V1 Sensory Function
V1 Sensory Function
Signup and view all the flashcards
V2 Sensory Function
V2 Sensory Function
Signup and view all the flashcards
V3 Sensory Function
V3 Sensory Function
Signup and view all the flashcards
Trigeminal Neuralgia Trigger Zone
Trigeminal Neuralgia Trigger Zone
Signup and view all the flashcards
Key Sign: Trigeminal Neuralgia
Key Sign: Trigeminal Neuralgia
Signup and view all the flashcards
Manifestation of Trigeminal Neuralgia
Manifestation of Trigeminal Neuralgia
Signup and view all the flashcards
Motor Fibres Cranial Nerve V
Motor Fibres Cranial Nerve V
Signup and view all the flashcards
Bell's Palsy Precaution
Bell's Palsy Precaution
Signup and view all the flashcards
Bell's Palsy Position
Bell's Palsy Position
Signup and view all the flashcards
Bell's Palsy Hydrotherapy
Bell's Palsy Hydrotherapy
Signup and view all the flashcards
Bell's Palsy Treatment
Bell's Palsy Treatment
Signup and view all the flashcards
Breathing Emphasis
Breathing Emphasis
Signup and view all the flashcards
Unaffected Side Treatment
Unaffected Side Treatment
Signup and view all the flashcards
Home Exercise for Bell's Palsy
Home Exercise for Bell's Palsy
Signup and view all the flashcards
Home Hydrotherapy
Home Hydrotherapy
Signup and view all the flashcards
Study Notes
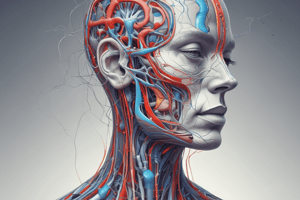
- Neuralgia is a type of nerve dysfunction, also described as "nerve-pain."
Neuralgia Overview:
- Pain occurs in the distribution of nerves without objective signs or structural damage.
- Any nerve is susceptible, though neuralgia is common in trigeminal (Cranial Nerve 5) and intercostal nerves.
- Appears as sudden, excruciating attacks described as "lightning-like" or throbbing.
- No tissue damage or injury exists in the affected nerve.
- Trigger zones cause attacks when stimulated.
Causes of Neuralgia:
- Local compression from neuroma or previous injury.
- Demyelinating conditions like MS, which can lead to scar tissue formation.
- Bony callus from a previous injury.
- Prolonged exposure to cold.
Key Characteristics of Neuralgia:
- Produces paroxysmal, intense, unilateral pain along the nerve distribution, often described like a knife or electric shock.
- Pain lasts from seconds to minutes.
- Neuralgias are often clustered and have trigger zones
Trigger Zones:
- Stimuli include light touch, temperature extremes (especially cold), and intense light.
- Sometimes movement stimulates trigger zones
Precaution:
- Avoid stimulating the trigger zone during assessment, manual techniques, or positioning.
Intercostal Neuralgia:
- Characterized by a trigger zone distributed along the affected spinal segment and laterally in the intercostal space.
Intercostal Neuralgia:
- Described as horrible, lightning-like pain with no apparent cause.
- Shingles, marked by skin eruptions turning into scabs, can be a cause, with pain fading as vesicles heal.
- Manifests as unilateral pain in nerve distribution
- It is not a condition of nerve degeneration but requires extreme caution due to trigger zones.
History Questions for Neuralgia:
- Identifying triggers (stimuli, location, predictability, patterns)
- Sensitivity to touch and pressure
- Doctor's diagnosis, prognosis, and ongoing treatments
- Onset, progression (better, worse, same), and rate of change
Assessment for Neuralgia:
- Avoid touching trigger zones, especially if a diagnosis exists
Differential Diagnosis:
- None specified
Treatment for Neuralgia:
- During acute phase and immediately following the most recent attack, focus on treating areas other than the affected site.
- Relaxation techniques, including diaphragmatic breathing
- Abdominal massage with diaphragm release
- Rib springing for thoracic mobility, unless contraindicated by osteoporosis, bone conditions, or muscle spasm
- Only touch the trigger zone if you have asked about the triggers and you are sure your touch will not trigger pain
- Work around the trigger zone with diaphragm, then rib, intercostal, and thoracic work that does not touch the trigger zone
- Treat intercostal muscle TrPs that are not trigger zones
Home Care for Intercostal Neuralgia:
- Diaphragmatic breathing.
- Pain-free thoracic mobility exercises that do not trigger pain.
Trigeminal Neuralgia Trigger Zone:
- Includes lips, face, and tongue.
- Most commonly involves areas innervated by the maxillary division (V2), or sometimes the maxillary and mandibular divisions (V3).
Key Sign of Trigeminal Neuralgia:
- Horrible, lightning-like pain with no apparent cause
Manifestations of Trigeminal Neuralgia:
- Unilateral pain in nerve distribution
- Facial tics
- Inflammation of sclera or iris, possibly glaucoma
- Hearing loss due to paralysis of the tensor tympani
- Locked jaw due to paralysis of muscles of mastication
Differential Diagnosis for Trigeminal Neuralgia:
- Acute migraine and cluster headaches
- Myofascial pain
Treatment for Trigeminal Neuralgia:
- Avoid treatment over the trigger zone.
- Address muscle spasms and trigger points to reduce facial tics
- Warm face cloth to reduce tension.
- Promote relaxation, including diaphragmatic breathing.
- Decrease facial pain with light massage of the face or scalp.
- Decrease trigger points in muscles of mastication
- Decrease tension using warm compress on affected area
Home Care for Trigeminal Neuralgia:
- Facial exercises
Cranial Nerve 5 (V) (Trigeminal):
- Has three main branches: ophthalmic, maxillary, and mandibular.
- Each main branch divides into several named cutaneous nerves.
Cranial Nerve 7 (VII) (Facial):
- Branches include: temporal, zygomatic, buccal, marginal mandibular, and cervical.
- Pathway: Pons > internal acoustic meatus > inner ear > stylomastoid foramen > through parotid gland.
- Has general somatic sensory fibers innervating the skin of the ear canal and tympanic membrane.
- Has special sensory fibers which supply taste to the anterior two thirds of the tongue.
- Compression sites: Inner ear (intracranial) and parotid gland
- Functions:
- Motor (Facial expression, Mastication)
- Sensory (Taste)
- Autonomic Lacrimation, Sweating)
Palpation for Cranial Nerve 7:
- Palpate or percuss the parotid gland or zygomatic arch
- Assess flaccidity of muscles around forehead, eye, nose & mouth
- Detect boggy edema around parotid gland on affected side
Bell's Palsy:
- Neurological condition affecting 25 out of 100,000 people each year, most common between ages 15 and 45.
- Rapid onset of symptoms, progressing quickly from weakness to flaccidity
Key Signs of Bell's Palsy:
- Eye closure is difficult or impossible (orbicularis oculi).
- Eye opening is fine because of different innervation (levator palpebrae superioris via cranial nerve 3).
Manifestations of Bell's Palsy:
- All are unilateral
- Forehead wrinkles disappear
- Overall droopy appearance
- Difficult or impossible to blink
- Nose runs and constantly feels stuffed
- Difficulty speaking, eating, drinking
- Sensitivity to low tones (hyperacusis)
- Excess or reduced salivation (autonomic)
- Facial swelling
- Pain in or near the ear
- Drooling
- Excessive or reduced tearing (autonomic)
- Brow droop
- Lower eyelid droop
- Sensitivity to light
- Loss of taste in anterior 2/3 of tongue
Etiology of Bell's Palsy:
- Cause is not well understood
- Herpes simplex or zoster reactivation or other infection in inner ear
- Parotid gland infection (mumps)
- Trauma, especially to temporal bone
- Tumors (acoustic neuroma, parotid gland)
- Increased risk with diabetes mellitus and pregnancy (3rd trimester).
History Questions for Bell's Palsy:
- Systemic disorders (diabetes, pregnancy, cardiovascular conditions)
- Doctor's diagnosis, prognosis, and treatments.
- Approved for local massage
- Onset, progression (better, worse, same), and rate of change
- Sensory changes (taste, hearing)
- Changes to normal function (sweating, lacrimation, dry eyes)
- Pain (not common)
Assessment for Bell's Palsy:
- Observation:(Drooping/downward pulling on affected side, eye and mouth droop, loss of wrinkles, excessive lacrimation)
- AROM and RROM of facial expression muscles
Differential Diagnosis for Bell's Palsy:
- Stroke typically affects lower muscles of the face, whereas Bell’s Palsy affects all muscles
Precautions for Bell's Palsy Treatment:
- It is a condition of nerve degeneration.
- Avoid prone positioning
- Modify pressure for flaccid tissue
- Prevent traction on the nerve with dragging strokes
- Work towards the affected side to prevent dragging
- Extra support around the stylomastoid foramen when supine
- Avoid traction of the supraclavicular area (platysma)
- Do not use fascial techniques
Treatment for Bell's Palsy:
- Supine position, towel for tearing and drooling, towel between therapist and affected side
- Warm cloth on affected area, cool washes on affected tissues, avoid local heat over unaffected side
- Block to protect tissues, encourage diaphragmatic breathing
- Treat unaffected side of chest, post neck, shoulder, scalp, and face with pressure towards lesion
- On affected side use techniques that move from mid-line toward the lesion , cue and assist with facial expressions and use light brushing/stroking towards lesion
Home Care for Bell's Palsy:
- Apply cool cloth before exercise, moist heat for relief.
- Practice facial expressions in mirror 2-3 times per days for 2-5min each time.
- Get MD for eye treatment and use eye cover
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.