Podcast
Questions and Answers
What is the primary embryological event that is disrupted in neural tube defects (NTDs)?
What is the primary embryological event that is disrupted in neural tube defects (NTDs)?
- Failure of the neural tube to completely close during early pregnancy. (correct)
- Disruption in the formation of somites, affecting the development of the vertebral column.
- Abnormal proliferation of neurons in the developing brain leading to cortical dysplasia.
- Improper migration of neural crest cells affecting craniofacial development.
A pregnant woman with a history of NTD in a previous pregnancy is planning her next pregnancy. What is the MOST important recommendation regarding folic acid intake?
A pregnant woman with a history of NTD in a previous pregnancy is planning her next pregnancy. What is the MOST important recommendation regarding folic acid intake?
- She should take the standard prenatal vitamin containing 0.4mg of folic acid daily.
- She should only consume foods naturally rich in folate, avoiding synthetic folic acid.
- She should avoid folic acid supplements to prevent excessive levels in the fetus.
- She should take a higher dose of folic acid (e.g., 4mg daily) starting at least one month before conception and continuing through the first trimester. (correct)
Which of the following assessment findings in a newborn is MOST indicative of anencephaly?
Which of the following assessment findings in a newborn is MOST indicative of anencephaly?
- Complete or partial absence of the cerebral hemispheres and overlying skull. (correct)
- Enlarged head circumference with bulging fontanelles.
- Dimpling and tufts of hair on the lower back.
- Presence of a sac-like protrusion on the lower back containing spinal fluid and neural tissue.
A newborn is diagnosed with myelomeningocele. What immediate nursing intervention is MOST critical to prevent complications?
A newborn is diagnosed with myelomeningocele. What immediate nursing intervention is MOST critical to prevent complications?
A child with myelomeningocele is being evaluated for hydrocephalus. Which clinical manifestation would MOST strongly suggest the presence of hydrocephalus?
A child with myelomeningocele is being evaluated for hydrocephalus. Which clinical manifestation would MOST strongly suggest the presence of hydrocephalus?
Infants with myelomeningocele are at high risk for developing latex allergy due to repeated exposure during surgeries and procedures. Which intervention is MOST important to minimize this risk?
Infants with myelomeningocele are at high risk for developing latex allergy due to repeated exposure during surgeries and procedures. Which intervention is MOST important to minimize this risk?
In a newborn with myelomeningocele awaiting surgical repair, which nursing action is CONTRAINDICATED?
In a newborn with myelomeningocele awaiting surgical repair, which nursing action is CONTRAINDICATED?
A child with cerebral palsy (CP) exhibits increased muscle tone, particularly in the lower extremities, leading to scissoring gait. Which type of CP is MOST consistent with this presentation?
A child with cerebral palsy (CP) exhibits increased muscle tone, particularly in the lower extremities, leading to scissoring gait. Which type of CP is MOST consistent with this presentation?
A child with cerebral palsy has difficulty coordinating movements needed for feeding, often choking or aspirating food. Which intervention is MOST important to ensure safe nutrition?
A child with cerebral palsy has difficulty coordinating movements needed for feeding, often choking or aspirating food. Which intervention is MOST important to ensure safe nutrition?
A child with cerebral palsy is prescribed baclofen. What is the PRIMARY therapeutic effect of this medication?
A child with cerebral palsy is prescribed baclofen. What is the PRIMARY therapeutic effect of this medication?
What is a key difference between spastic and dyskinetic cerebral palsy concerning the nature of motor impairments?
What is a key difference between spastic and dyskinetic cerebral palsy concerning the nature of motor impairments?
A preterm infant is born at 30 weeks gestation. Which common condition associated with prematurity is MOST directly related to immature lung development?
A preterm infant is born at 30 weeks gestation. Which common condition associated with prematurity is MOST directly related to immature lung development?
A preterm infant is receiving supplemental oxygen. Which potential complication requires careful monitoring to prevent long-term visual impairment?
A preterm infant is receiving supplemental oxygen. Which potential complication requires careful monitoring to prevent long-term visual impairment?
A nurse is caring for a preterm infant born at 32 weeks gestation. Which intervention BEST supports neurodevelopment and minimizes stress?
A nurse is caring for a preterm infant born at 32 weeks gestation. Which intervention BEST supports neurodevelopment and minimizes stress?
A preterm infant develops apnea of prematurity (AOP). If apneic spells worsen following infection, which intervention is MOST important?
A preterm infant develops apnea of prematurity (AOP). If apneic spells worsen following infection, which intervention is MOST important?
A preterm infant is being discharged home. What parental education is MOST critical regarding preventing infection?
A preterm infant is being discharged home. What parental education is MOST critical regarding preventing infection?
What is the MOST immediate risk associated with increased intracranial pressure (ICP)?
What is the MOST immediate risk associated with increased intracranial pressure (ICP)?
How does the body initially compensate for a small increase in intracranial pressure (ICP)?
How does the body initially compensate for a small increase in intracranial pressure (ICP)?
A child presents with a history of rapid head growth, bulging fontanelles, and irritability as an infant, along with vision changes, difficulty walking and poor memory as an older child. These findings are MOST indicative of what condition?
A child presents with a history of rapid head growth, bulging fontanelles, and irritability as an infant, along with vision changes, difficulty walking and poor memory as an older child. These findings are MOST indicative of what condition?
What is a key difference between communicating and non-communicating hydrocephalus?
What is a key difference between communicating and non-communicating hydrocephalus?
A child with hydrocephalus develops rapid onset of irritability, lethargy, and a high-pitched cry. Which complication should the nurse suspect?
A child with hydrocephalus develops rapid onset of irritability, lethargy, and a high-pitched cry. Which complication should the nurse suspect?
Following surgical placement of a ventriculoperitoneal (VP) shunt for hydrocephalus, a child should be positioned:
Following surgical placement of a ventriculoperitoneal (VP) shunt for hydrocephalus, a child should be positioned:
What is TRUE regarding the nature of Parkinson's Disease pathophysiology?
What is TRUE regarding the nature of Parkinson's Disease pathophysiology?
A patient with Parkinson's disease is prescribed levodopa/carbidopa. Which instruction is MOST important to provide regarding medication administration?
A patient with Parkinson's disease is prescribed levodopa/carbidopa. Which instruction is MOST important to provide regarding medication administration?
A patient with Parkinson's disease develops dysphagia. Which dietary modification is MOST appropriate to reduce the risk of aspiration?
A patient with Parkinson's disease develops dysphagia. Which dietary modification is MOST appropriate to reduce the risk of aspiration?
Following a stroke affecting the right side of the brain, a patient is MOST likely to exhibit:
Following a stroke affecting the right side of the brain, a patient is MOST likely to exhibit:
A patient experiencing sudden onset of right arm weakness, slurred speech, and facial droop is MOST likely experiencing:
A patient experiencing sudden onset of right arm weakness, slurred speech, and facial droop is MOST likely experiencing:
When using the BE FAST mnemonic to assess a potential stroke, what does the 'E' stand for?
When using the BE FAST mnemonic to assess a potential stroke, what does the 'E' stand for?
What is the primary difference between an ischemic and hemorrhagic stroke?
What is the primary difference between an ischemic and hemorrhagic stroke?
Which modifiable lifestyle factor contributes SIGNIFICANTLY to the risk of stroke?
Which modifiable lifestyle factor contributes SIGNIFICANTLY to the risk of stroke?
What is the PRIMARY goal of administering tissue plasminogen activator (tPA) in the treatment of ischemic stroke?
What is the PRIMARY goal of administering tissue plasminogen activator (tPA) in the treatment of ischemic stroke?
A patient with a history of transient ischemic attacks (TIAs) is MOST at risk for:
A patient with a history of transient ischemic attacks (TIAs) is MOST at risk for:
A key difference between ischemic and hemorrhagic stroke onset is:
A key difference between ischemic and hemorrhagic stroke onset is:
What is the potential danger if a patient with stroke tends to deny health problems after a stroke?
What is the potential danger if a patient with stroke tends to deny health problems after a stroke?
Which of the following is an appropriate intervention for stroke patients?
Which of the following is an appropriate intervention for stroke patients?
Flashcards
Neural Tube Defects (NTD)
Neural Tube Defects (NTD)
Defects that occur when the neural tube doesn't close completely during pregnancy, affecting the brain and spinal cord.
Anencephaly
Anencephaly
A severe NTD where the brain's cerebral hemispheres are absent; infants may be stillborn or die shortly after birth.
Spina Bifida
Spina Bifida
A NTD where the spinal cord doesn't close completely, potentially leading to neurological deficits.
Spina Bifida Occulta
Spina Bifida Occulta
Signup and view all the flashcards
Meningocele
Meningocele
Signup and view all the flashcards
Myelomeningocele
Myelomeningocele
Signup and view all the flashcards
Cerebral Palsy (CP)
Cerebral Palsy (CP)
Signup and view all the flashcards
Spastic CP
Spastic CP
Signup and view all the flashcards
Apnea of Prematurity (AOP)
Apnea of Prematurity (AOP)
Signup and view all the flashcards
Retinopathy of Prematurity (ROP)
Retinopathy of Prematurity (ROP)
Signup and view all the flashcards
Neonatal Sepsis
Neonatal Sepsis
Signup and view all the flashcards
Kangaroo Care
Kangaroo Care
Signup and view all the flashcards
Intracranial Regulation
Intracranial Regulation
Signup and view all the flashcards
Hydrocephalus
Hydrocephalus
Signup and view all the flashcards
Communicating Hydrocephalus
Communicating Hydrocephalus
Signup and view all the flashcards
Noncommunicating Hydrocephalus
Noncommunicating Hydrocephalus
Signup and view all the flashcards
Mobility
Mobility
Signup and view all the flashcards
Parkinson's Disease
Parkinson's Disease
Signup and view all the flashcards
Ischemic stroke
Ischemic stroke
Signup and view all the flashcards
Hemorrhagic Stroke
Hemorrhagic Stroke
Signup and view all the flashcards
Transient Ischemic Attack (TIA)
Transient Ischemic Attack (TIA)
Signup and view all the flashcards
BEFAST
BEFAST
Signup and view all the flashcards
Study Notes
- Development, Cognition, and Mobility, Week 7
Neural Tube Defects (NTD)
- NTD is when the neural tube fails to close completely during embryonic development.
- Neural tube is the structure in a developing embryo that becomes the infant's brain, spinal cord, and surrounding tissues.
- Neural tube folds and closes early in pregnancy, around weeks 3-4.
- Failure to close can occur anywhere along the brain, neck, or spine.
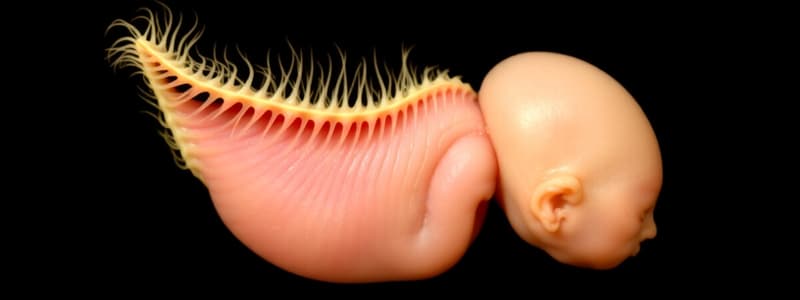
- NTD types include Anencephaly and Spina Bifida.
- Spina Bifida includes Spina Bifida Occulta, Meningocele, and Myelomeningocele.
- Etiology factors for NTD include folic acid deficiency, previous NTD pregnancy, maternal malnutrition, exposure to drugs/radiation/chemicals, and genetic mutation.
- Daily folic acid intake for childbearing women is 0.4mg.
- NTD causes and risk factors are not always known but are associated w/ factors interfering with CNS development such as folate deficiency, malnutrition, and maternal obesity
- Other causes and risk factors include Infections, Medications (Sodium Valproate & Methotrexate) and exposure to Chemicals.
Neural Tube Defects (NTD): Anencephaly
- It is a congenital malformation where both cerebral hemispheres are absent.
- Most infants are stillborn or die shortly after birth
- Infants are born with a portion of the brainstem.
- They can maintain temperature, cardiac, and respiratory function for hours to weeks, but will eventually die of respiratory failure.
- There is no specific treatment.
- Clinical manifestations include the infant born without a forebrain or cerebrum with remaining brain tissue exposed.
- The condition is incompatible with life, with most infants dying in the womb or within hours to weeks after birth.
- Background includes a fatal birth defect where the infant is born without most of the brain and overlying skull/scalp, resulting in death shortly after birth.
- Risk factors include genetics, environment, geography, nutrition, Hispanic ethnicity, female sex at birth, hot tub use during pregnancy, lack of folic acid, and use of anti-seizure medications.
- Signs & Symptoms
- Newborns born without parts of brain tissue, skull, and scalp. The superior part of the head is typically absent or particularly small.
- Some brain tissue may be exposed
- Resulting in the baby being unconscious, blind, deaf, and without pain sensitivity.
- If part of the brainstem evolves, reflexes like breathing or responding to touch/sound may be possible.
- Absent parts of the brain responsible for swallowing could lead to Polyhydraminos.
- Possible Fetal malpositioning, placental abruption, and premature birth.
- Diagnosis is made through ultrasound, elevated alpha-fetoprotein in maternal serum, and physical examination.
- There is no cure or treatment, but prevention is done to reduce incidence through early detection, diagnosis, and folic acid supplement.
Neural Tube Defects (NTD): Spina Bifida
- Spina Bifida Cystica types include of Meningocele and Myelomeningocele.
- Meningocele: the sac contains spinal fluid and meninges but no spinal contents, may or may not have neurological defects.
- Myelomeningocele: the sac contains spinal fluid, meninges, and nerve with decreased motor and sensory function depending on lesion location.
- In both Spina Bifida Cystica types the cyst can be seen visible as a cyst of the meninges through the Vertebrae.
- Myelomeningocele: the spinal cord herniates out of the vertebral defect, making it easier to damage
- Increasing the Risk of developing motor and sensory dysfunction below the defect.
- Possibility of meningitis, hemorrhage, and hypoxia
- Causing Bladder/ Bowel Incontinence
- Spina Bifida Occulta
- Frequently has no observable manifestations, but can be associated with cutaneous manifestations like skin depression/dimple, port-wine stain, dark tufts of hair, and soft, subcutaneous lipomas
- May have progressive neuromuscular disturbances such as gait problems and bowel/bladder difficulties.
- Spina Bifida Cystica symptoms depend on the anatomic level of the defect and nerves involved
- Leading to Bowel and bladder difficulties, flaccid extremities, and joint deformities from in utero positioning.
- Also causing Varied degrees of sensory deficits
- Hydrocephalus often present
- Spinal defects
- Spina Bifida Occulta:
- Posterior vertebral arches fail to close, but the spinal cord and meninges remain in place.
- The defect is not visible from the outside.
- Spina Bifida Cystica defects:
- Parts of the spinal cord herniate through an abnormal gap in the vertebrae, forming a cyst.
- Meningocele involves only meninges herniating into the cyst.
- Myelomeningocele contains meninges and spinal cord.
- Other associated conditions
- Latex allergy; repeated exposure during surgery and procedures
- Tethered spinal cord: the spinal cord attaches to the spinal canal and stretches as the child grows, creating spinal nerve damage.
- Paralysis and mobility limitations which vary depending on type and severity of the spina bifida.
- Hydrocephalus, seen most frequently in myelomeningoceles.
- Care for Newborns W/ Myelomeningocele priority goals: Psychological support, Prevent Complications, and minimize Heat & Fluid loss.
- Myelomeningocele Surgical Repair:
- Fetoscopic repair is a surgical repair that occurs while the fetus is still in utero
- Traditional repair is on baby right after birth
- Dressing changes post-op to prevent sac rupture, should consist of sterile, moist, non-adherent dressings.
- Ensuring the dressing should not dry out and Remaining in prone position prior/post surgery.
- Infant should be fed with head turned to side with NG placement while being monitored wit Axillary temps.
- Prevent skin breakdown with Gentle ROM, checking the head circumference.
- Spina Bifida is diagnosed prenatally with Amniotic Fluid & Maternal Blood test for AFP & Acetylcholinesterase.
- After Birth can be diagnosed with Physical Examination, Imaging, Cranial Ultrasound to asses for Hydrocephalus.
- This defect can be prevented wit Folic Acid Supplementations.
- Ideally through Cesarean Section
- priority nursing goals include minimizing heat & fluid loss, preventing complications and psychosocial suport.
- Client and Family Teaching shoul include how to care of the baby at home when to seek medical attention and how to prevent future NTDs in future pregnancies
Cerebral Palsy
- CP is a non-progressive, but not unchanging, neuromuscular disorder with posture and movement limitations from static brain injury prenatally or postnatally.
- Abnormal brain development or damage occurs to the cerebral cortex, basal ganglia, or cerebellum.
- Etiology, clinical features, and course vary but are characterized by abnormal muscle tone and coordination, often impacting sensation, perception, communication, cognition, and behavior.
- Many experience secondary musculoskeletal problems and epilepsy.
- Signs and symptoms include delayed gross motor development, abnormal motor performance, altered muscle tone and posture, reflex abnormalities, and visual/hearing/speech/intellectual problems or seizures.
Cerebral Palsy Risk Factors
- Prenatal risk factors: maternal diabetes/hyperthyroidism/infections/bleeding, gestational congenital malformations, fetal development abnormality, placental issues, and teratogens.
- Labor & Delivery risk factors: Premature delivery, Prolonged rupture of membranes, prolonged fetal heart rate depression, long labor, preeclampsia, Asphyxia, or abnormal presentation.
- Perinatal risk factors: sepsis/CNS infection, seizures, intraventricular hemorrhage, meconium aspiration, intrauterine growth restriction, low birth weight, or perinatal stroke.
- Childhood/Postnatal Risk Factors include Brain injury, Meningitis / Encephalitis, Toxins, Traumatic brain injury, Infections , and Stroke.
- Unknown prenatal factors can contribute to 70-80% of CP cases.
- Cerebral Palsy types:
- Spastic (Pyramidal): tense, contracted muscles with classifications into monoplegia, hemiplegia, diplegia, or quadriplegia.
- Dyskinetic: Constant, uncontrolled motion of limbs/head/eyes that interferes with feeding, swallowing, and speech.
- Ataxic: Poor sense of balance causing falls/stumbles with wide-based, unsteady gait.
- Mixed Type: Combination of spastic and dyskinetic CP.
Cerebral Palsy Complications and Nursing Considerations
- Complications includes, Aspiration because patients cant handle Drooling.
- Nurse can prepare action, keeping bed Elevated and Parents know CPR.
- Potential for Injury, Patient should be place on padded rails
- Nurse should be aware of seizure precautions and Encourage rest.
- Goals of Therapy incude, Early Recognition and enabling the children to attain potential.
- Nursing Care:
- Repositioning patient with Frequent skin assessment.
- When feeding, place put food to side of mouth
- The Nurse Should use Jaw control to assist with mouth closing by gentle pressure under chin.
- Seizure precautions and also Fall prevention should be take , cooridinating Home/School care
- Medications for this include; Baclofen (muscle spasticity), Diazepam (should be restricted to older children/adolescents), and Botulinum toxin A (used primarily for clients who only have spasticity in LE, monitor for temporary weakness and pain at injection site. Anti-epileptics
Prematurity
- Preterm: infant is born before 37 weeks of gestation.
- Late preterm: infant is born between 34 0/7 and 36 6/7 completed weeks of pregnancy.
- Common Conditions: Apnea, Respiratory distress syndrome, Retinopathy, Jaundice, Hemorrhage, Infection, Sepsis & Anemia.
- Maternal risk factors: previous premature birth, pregnancy with multiples, less than 6 months between pregnancies, IVF, uterus/cervix/placenta problems, smoking, illicit drug use, infections (amniotic fluid and lower genital tract), HTN/diabetes, under/over weight before pregnancy, stressful life events, miscarriages/abortions, trauma.
- Signs and symptoms: extended limbs, poorly developed ear cartilage, fine/feathery hair, lots of wrinkles on the sole of the foot and scarf sign.
- Apnea of Prematurity (AOP): "Apneic spells" are common in preterm babies, less than 32 weeks.
- Apnea is a spontaneous breathing lapse for >20 seconds or brief pauses alongside bradycardia or oxygen desaturations.
- It is attributed to undeveloped respiratory reflexes and muscle weakness.
- The Infection worsens apneic spells
- Often resolved around 37 weeks
- Management involves caffeine, closed monitoring and tactile stimulation of the baby.
- Retinopathy of Prematurity (ROP): primarily affects premature infants and can result in blindness. The more premature an infant is, the greater the ROP risk.
- High oxygen levels increase ROP risk in infants.
- Sepsis refers to generalized bacterial infection in the bloodstream, which preterm infants are highly susceptible to due to an immune system that still has not been fully developed.
- The IgG is normally acquired from the maternal system and stored in the fetus in the final weeks of gestation. -Early clinical manifestations are nonspecific, and can Hypothermia , Changes in color, tone, activity, feeding behavior, Sudden episodes of apnea and Unexplained oxygen desaturation events.
- Prevention should be aimed to be preformed using Hand hygiene and Breastfeeding
- General Care for Preemies:
- Minimize sensory stimuli by Decreasing sound, lights and using Clustering cares → after 30 weeks gestation
- Pain and stress reduction to avoid Increased sensitivity to pain. Frequent pain can lead to lifelong structural and functional Alterations in nervous systems/ pain responses
- Positioning similar to intrauterine environment with extremity flexion and hip adduction while containing the Neonate promotes healthy growing.
- Often improves vital sign, Breathing and deeper sleep while In prone position
Kangaroo Care
- A method of holding newborn skin to skin Stabilizing the infant's heart rate, Reducing illness and Infection, Enhancing breastfeeding, Improving breathing pattern/oxygen saturation levels, Better sleep, Decreased crying, and increased bonding.
Intracranial Regulation
- Balance of 3 components within the skull: brain tissue (80%), cerebrospinal fluid (CSF) (10%), and blood (10%).
- If any component's volume increases, another must decrease to maintain normal intracranial pressure (ICP).
- The body can compensate for volume changes within the skull by altering CSF production/absorption, increasing/decreasing cerebral blood flow, and brain tissue compensation.
- If volume continues to rise despite compensation, ICP will increase.
- Increased ICP decreases blood flow to the brain, leading to compression and ischemia.
Hydrocephalus
- A condition caused by an imbalance in the production and /or absorption of CSF.
- CSF accumulates in ventricles of brain becoming dialated.
- Can be Congenital or Acquired Conditions
- Congenital conditions causes include: Myelomeningocele, Aqueduct stenosis and Intrauterine viral infections such as Cytomegalovirus (CMV) and Toxoplasmosis.
- Acquired includes: Intraventricular hemorrhage, Tumor, CSF infection, or Head Injury
- Communicating Hydrocephalus (Non-obstructive) - No Obstruction the flow within the Ventricular System
- Impaired absorption or increased amount of CSF.
- Noncommunicating Hydrocephalus.
- Obstruction the flow within the Ventricular System.
- Clinical Manifestation will Vary between infants and older children/Adults:
- Infants will show symptoms such as Bulging Fontanels, Setting Sunsign Eyes and a Rapid increase in head circumference
- May also contain High Pitched cry, becomes Irritable and Lethargic
- Adults & Older childred Will experience Headaches on Awakening,
Nausea and Vomiting, difficulties with walking and Poor Memory.
- May also complain of, vision change or Change in LOC (Difficulties concentrating)
- If you can't resolve pressure then leads to Somnolence, Seizures, Cardiopulmonary distress , and/or Brain death.
- Therapeutic Management should be directed at relieving Ventricular pressure.
- Should be addressed by treating the underlying cause and any complication causing problems.
- And finally, Treatment can be by way of Surgically removing obstructions using, a Tumor , or Cysts.
- Also, Can be treated with Shunt procedures like Ventriculoperitoneal (VP) or Ventriculoarterial (VA) Shunt.
Hydrocephalus VP Shunt Complications
- Infection being the most common w/in 2 Months.
- Can be treated w/ IV intra-thecal antibiotics
- Recurrent infections may require removing shunt
- this can be temporary
- A malfunction leading to Kinking, Plugging, tubing migration or the beginning of Thrombus formation at the distal end of tubing.
- Nursing Patient Management to Monitor Hydrocephalus
- Place paint on un-operated side with Patient remaining flat.
- devices/magnets at minimum of 3cm from shunt valve, Usually behind ear!
- Perform Neuro and abdominal assessment
- Check Vitals signs and perform Daily head circumference monitoring!
- Provide Patient, Family support, educating on what to look or that would signal a dysfunction or infection.
Mobility
- Purposeful physical movement, including gross motor, fine motor, and coordination, which needs:
- Intact/functional neurological and musculoskeletal systems, and anatomical function for a change in position or location that demonstrates purposeful, pain-free movement.
- This enhances quality of life through improved functional ability, joint mobility, muscle strength, and system functioning (cardiac, respiratory, GI). Risk factors: older adults, chronic pain, injury/trauma, and congenital deformities.
- Negative consequences includes Reduction in muscle mass, atrophy, joint contraction, pressure ulcer development, anxiety, boredom or a Disturbed the body image.
Parkinson's Disease
- A chronic, progressive neurodegenerative disorder with Characteristics such as, Bradykinesia, Rigidity, Blank facial expression, slow monotone speech , and Tremor while resting.
- Etiology remains to be unknown, but may include Well Water.
- Risk factors are degeneration of dopamine producing neurons in the brain, and results in imbalance of dopamine and acetylcholine in the basal ganglia.
- The main Diagnostics is by patients history and having, Presence of TRAP with asymmetric onset!
Parkinson's Disease Collaborative care
- Nurse should be aware of side effects such as: spontaneous involuntary movement, Hallucinations, Dementia, Depression, Dysphagia and Aspiration or injuries such as Falls.
- Medications that could support collaborative care are: Levodopa/Carbidopa which Corrects imbalance of neurotransmitters,
Benztropin (Cogentin) to help Decreases muscle stiffness/saliva and Selegiline anti-depressent.
- Also big point is, Don't give Levodopa with food! patient should consult pt, ot/st, Dietician for best treatment.
Strokes
- Ischemic stroke: obstruction from a clot that is blocking blood flow to the brain.
- Hemorrhagic stroke: blood vessel ruptures which is stopping blood flow to the brain.
- Transient ischemic attack (TIA): caused by a temporary clot.
- Strokes are classified based on the underlying pathophysiologic findings: ischemia from inadequate blood flow or hemorrhage from bleeding.
- Loss of function varies according to brain tissue's location and extent of involvement.
- Prevalence: Currently 5th leading cause of death in US and Leading cause of serious, long-term disability.
- Survivors: 15-30% will experience permanent disability, requiring longterm care for both the survivor and family.
- Risk factors: include Nonmodifiable (Age, Gender , ethnicity, Family History) and/or Modifiable (Hypertension, Heart Disease, Diabetes, Tobacco Use, and Obesity.
- Can be identified in it's in early recognition using the, (B)E FAST or (F)AST acronym
Strokes Transient Ischemic Attack
- Transient episodes of
neurologic dysfunction caused
by focal brain, spinal cord or Retinal Ischemia,
but without acute infarction of
the brain.
- this is, Associated with an increased RISK
- symptoms typically last less than 1 hour. 1/3rd will progress to an ischemic stroke!
- Thrombotic being most common (60 %)
- Its devlopes where Atherosclerosis plaques have already causes narrowing
- Embolic Occurs when an embolus occludes a cerebral artery
- Most emboli originate in the endocardial layer of the heart Can also be sudden onset
- Patient will typically be put on a course of,
Treatment aTPA (clot buster)
Anti-Coagulation therapy.
- It's common too that Males > Women
- It's commin to that, TIA typically makes this Uncommon and it is on Sudden onset, activity!
- Males > W, ~1/3 (30%) experience TIA but During or after sleep.
- Prevention of Strokes- (THIS IS KEY!)
- Diet High Fruites and Veggies, consider Diet in case its duto Clog, prevent formation of Atherosclerosis by lowering fat and NA+ levels!
- NO Tabacco and Alcohol intake and Reduce Salt and/or Sugar in your Meals/Foods
- Take as Many meds prescribed!
- During a Stroke, it important to Assess respiratory status
- You provide position and, Asses presence of gag reflex! Assess Manifestation of Stroke in, infusing TPA for patients who will meet criteria
- This is Important because it needs to be, Administer within 3 hrs!
- Continue by monitoring Cardiovascular & neurologic status Giving Repostion/ROM.
Hemorrhagic Stroke
- Intracerebral stroke from bleeding within the brain caused by a rupture:
- Possible cuases Hypertension, coagulation disorders, anticoagulant therapy, or ruptured aneurysms.
- Patient will also experence frequent Headaches
- Subarachnoid : Intracranial bleeding into the CSF space between the arachnoid and pia meter
- this can be caused by Ruptured Aneurysm, Trauma and Illicit Drug use.
- Patient will more then often have Sudden onset
- Can be treated using:
- Surgical decompression if indicated
- Clipping or coiling of aneurysm
- Tight-lacing
- The chances for Hemorrhaging are More Common In Females
- For a Stroke what is importantis to always: THINK FAST
- Hemorrhagic stroke
Right & Left Brain Damage
-
Right-Brain Damage
- Paralysis or weakness occurs on the Left's side of the body and results in being, hemiplegic.
-
You also must take in to account, the Lefts, Spatial neglect.
- It takes more work to solve spatial-perception problems. And It may also have an Impulsive nature.
- In contrast also on other side is a decrease in attention on short attention spans when trying to perfoam a new actions
- It takes more work to solve spatial-perception problems. And It may also have an Impulsive nature.
-
Left-Brain Damage-
- Paralysis or weakness occurs on the (R) s/o the body resulting in being, hemiplegic.
-
Difficulty with speech occurs, typically in verbal-expressive language
- Slow or hesitant in language and a decreased attention span.
-
Diagnostic Studies:
-
Can be perform to check the Extents of the damage with CT. Also MRI and Cerebral and Carotid angiography
-
A CBC helps check Lipid profiel For Therapies- PT, Speech and OT, you most know!
-
Families can give support but also are impacted because a Family Member would need assist and maybe relocated
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.