Podcast
Questions and Answers
What primarily regulates water reabsorption in the body?
What primarily regulates water reabsorption in the body?
- Antidiuretic hormone (ADH) (correct)
- Natriuretic peptide
- Aldosterone
- Renin-angiotensin system
Which condition is associated with difficulties in ADH production and release?
Which condition is associated with difficulties in ADH production and release?
- Diabetes Mellitus
- Nephrogenic diabetes insipidus
- Pressure natriuresis
- Central diabetes insipidus (correct)
What effect does an increase in blood pressure have on sodium excretion?
What effect does an increase in blood pressure have on sodium excretion?
- Sodium excretion increases (correct)
- Sodium excretion remains constant
- Sodium is secreted more actively
- Sodium excretion decreases
What is the main function of pressure diuresis?
What is the main function of pressure diuresis?
What is the concept of Effective Circulating Volume (ECV) related to?
What is the concept of Effective Circulating Volume (ECV) related to?
What is the role of the thalamus in sensory perception?
What is the role of the thalamus in sensory perception?
Which type of nerve fibers are primarily associated with nociceptors?
Which type of nerve fibers are primarily associated with nociceptors?
Which sensory system is responsible for proprioceptive and tactile sensation?
Which sensory system is responsible for proprioceptive and tactile sensation?
What is a key feature of dermatomes?
What is a key feature of dermatomes?
Which statement best describes sensory adaptation?
Which statement best describes sensory adaptation?
What is the primary function of the renal corpuscle?
What is the primary function of the renal corpuscle?
Which components form the filtration barrier in the nephron?
Which components form the filtration barrier in the nephron?
What does GFR stand for in the context of kidney function?
What does GFR stand for in the context of kidney function?
Which nephron type is primarily involved in the regulation of water and electrolytes?
Which nephron type is primarily involved in the regulation of water and electrolytes?
What is the approximate daily urine output produced by healthy kidneys?
What is the approximate daily urine output produced by healthy kidneys?
Which component of the juxtaglomerular apparatus is responsible for sensing sodium concentration?
Which component of the juxtaglomerular apparatus is responsible for sensing sodium concentration?
Which process occurs first in the urine formation sequence?
Which process occurs first in the urine formation sequence?
Which factor is not considered in determining the Glomerular Filtration Rate (GFR)?
Which factor is not considered in determining the Glomerular Filtration Rate (GFR)?
What is the primary function of the thin descending limb of the loop of Henle?
What is the primary function of the thin descending limb of the loop of Henle?
In the ascending limb of the loop of Henle, what transport mechanism is responsible for NaCl reabsorption?
In the ascending limb of the loop of Henle, what transport mechanism is responsible for NaCl reabsorption?
What percentage of filtered water is typically reabsorbed in the thin descending limb of the loop of Henle?
What percentage of filtered water is typically reabsorbed in the thin descending limb of the loop of Henle?
What role does the antidiuretic hormone (ADH) play in the distal and collecting tubules?
What role does the antidiuretic hormone (ADH) play in the distal and collecting tubules?
Which of the following segments is impermeable to water and urea?
Which of the following segments is impermeable to water and urea?
What is the maximal concentrating ability of urine in terms of osmolarity?
What is the maximal concentrating ability of urine in terms of osmolarity?
How does the countercurrent multiplier system contribute to renal function?
How does the countercurrent multiplier system contribute to renal function?
Which type of cell in the late segment of the distal tubule functions to regulate acid-base balance?
Which type of cell in the late segment of the distal tubule functions to regulate acid-base balance?
What is the normal pH level of the human body?
What is the normal pH level of the human body?
Which process involves the secretion of H+ and reabsorption of HCO3- in the kidneys?
Which process involves the secretion of H+ and reabsorption of HCO3- in the kidneys?
What is a primary mechanism of respiratory regulation of acid-base balance?
What is a primary mechanism of respiratory regulation of acid-base balance?
What type of acidosis is characterized by an increase in Pco2 levels?
What type of acidosis is characterized by an increase in Pco2 levels?
Which of the following is NOT a function of the kidneys in acid-base regulation?
Which of the following is NOT a function of the kidneys in acid-base regulation?
Which condition is characterized by hyperventilation and low Pco2?
Which condition is characterized by hyperventilation and low Pco2?
Which type of sensory receptor responds primarily to changes in temperature?
Which type of sensory receptor responds primarily to changes in temperature?
Which sensory system is responsible for sensing pain and temperature?
Which sensory system is responsible for sensing pain and temperature?
What kind of adaptation do rapidly adapting receptors exhibit?
What kind of adaptation do rapidly adapting receptors exhibit?
In acid-base imbalance, what does an increase in HCO3- typically indicate?
In acid-base imbalance, what does an increase in HCO3- typically indicate?
Flashcards are hidden until you start studying
Study Notes
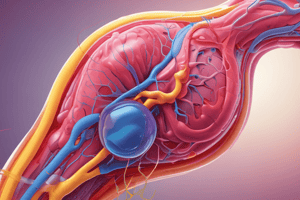
Nephron Structure
- The nephron is the functional unit of the kidney, responsible for filtering blood and producing urine.
- Each kidney contains approximately 1 million nephrons, each weighing about 150 grams.
- Each nephron is made up of two main parts: the renal corpuscle and the renal tubule.
- The renal corpuscle is composed of a glomerulus (a capillary network) and Bowman's capsule (a surrounding epithelial sac).
- The renal tubule is a long, convoluted tube that extends from the Bowman's capsule, divided into sections: proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct.
Glomerular Filtration
- Glomerular filtration is the first step in urine formation, where blood is filtered through the glomerulus into Bowman's capsule.
- The filtration barrier consists of three layers: endothelium (capillary lining), basement membrane (between endothelium and podocytes), and epithelium (podocytes, specialized cells wrapping capillaries).
- The filtration process excludes blood cells and large proteins, allowing smaller molecules like water, glucose, electrolytes, and waste products to pass.
Juxtaglomerular Apparatus
- The juxtaglomerular apparatus (JGA) is a specialized structure where the distal tubule comes in close contact with the glomerulus.
- The JGA plays a crucial role in regulating glomerular filtration rate (GFR) through the tubuloglomerular feedback mechanism.
- The JGA has two key components:
- Macula densa: A group of densely packed epithelial cells in the thick ascending limb of the loop of Henle that sense changes in tubular fluid flow and composition.
- Juxtaglomerular cells: Specialized smooth muscle cells in the walls of the afferent arteriole that secrete renin, an enzyme involved in blood pressure regulation.
Urine Formation
- Urine formation involves four distinct processes:
- Glomerular filtration: Initial filtering of blood into the nephrons, producing approximately 180 liters of filtrate per day.
- Tubular reabsorption: Reabsorption of essential nutrients, water, and electrolytes back into the bloodstream from the renal tubules.
- Tubular secretion: Active transport of waste products and excess ions from the bloodstream into the renal tubules.
- Urinary excretion: The final processed urine containing waste products and excess water is excreted out of the body.
GFR Regulation
- GFR is the volume of filtrate produced by the kidneys per minute.
- GFR is determined by the glomerular filtration pressure (EFP), which is the difference between glomerular pressure (PGC), Bowman's capsule pressure (PBS), and capillary oncotic pressure (πGC).
- GFR regulation involves mechanisms affecting blood pressure, blood volume, and constriction/dilation of afferent and efferent arterioles supplying the glomerulus.
- The kidneys can tightly regulate GFR over a wide range of blood pressures, known as auto-regulation.
Transport in the Nephron
- The renal tubule plays a key role in reabsorbing essential substances and excreting waste products.
- Different segments of the renal tubule have distinct transport properties:
- Proximal Tubule: Responsible for the reabsorption of most of the filtered glucose, amino acids, sodium, and chloride.
- Loop of Henle: Critical for concentrating urine through the countercurrent multiplier system. The descending limb is permeable to water but impermeable to salts, while the ascending limb is impermeable to water but permeable to salts.
- Distal Tubule: Fine-tunes electrolyte balance by reabsorbing sodium and chloride, secreting potassium and hydrogen ions, and regulating calcium reabsorption.
- Collecting Duct: Final reabsorption of water (regulated by ADH) and removal of excess potassium and hydrogen ions.
Renal Osmoregulation
- The human kidney can produce urine with a wide range of concentrations, from very dilute (50 mOsm/L) to highly concentrate (1200 mOsm/L).
- The regulation of urine concentration is essential for maintaining body fluid osmolality and electrolyte balance.
- The countercurrent multiplier system within the loop of Henle allows for the establishment of a high osmotic pressure gradient in the renal medulla, driving water reabsorption.
- Antidiuretic hormone (ADH) plays a critical role in regulating water reabsorption in the distal tubule and collecting duct, promoting concentrated urine formation when the body is dehydrated.
Disorders of Urine Concentration
- Central Diabetes Insipidus: Occurs when the pituitary gland fails to produce or release adequate ADH, leading to the production of large amounts of dilute urine.
- Nephrogenic Diabetes Insipidus: Results from a kidney's inability to respond to ADH effectively, causing dilute urine production.
Renal Regulation of ECF Volume, NaCl, and Blood Pressure
- Effective circulating volume (ECV) refers to the portion of the blood volume that is effectively perfusing the tissues.
- The body monitors and regulates ECV through various systems:
- Atrial Natriuretic Peptide (ANP): Released from the heart to promote sodium and water excretion and lower blood pressure.
- Renin-Angiotensin-Aldosterone System (RAAS): A complex hormone cascade triggered by low blood pressure or volume that increases sodium and water reabsorption, thus raising blood pressure.
- Sympathetic Nervous System: Stimulates vasoconstriction and renin release, leading to increased blood pressure.
Renal Regulation of Acid-Base Balance
- The kidneys play a crucial role in maintaining the body's acid-base balance, the pH of the extracellular fluid (ECF).
- The kidney's primary function is to:
- Reabsorb filtered bicarbonate (HCO3-) from the renal tubules.
- Secrete hydrogen ions (H+) into the tubules.
- Generate new HCO3- to buffer acids.
- Acidosis (low pH) and alkalosis (high pH) are conditions that disrupt acid-base balance. Respiratory compensation involves altering breathing rate and depth to adjust CO2 levels in the blood, while renal compensation involves adjusting H+ and HCO3- reabsorption and excretion to correct the pH.
The Somatosensory System
- The somatosensory system is responsible for processing sensory information from the body, including touch, temperature, pain, pressure, and proprioception.
- Sensory receptors transduce physical stimuli into electrical signals, which are transmitted through a chain of neurons:
- Sensory receptor: Detects the stimulus (touch, temperature, pain, etc.).
- Primary afferent neuron: Transmits the signal from the receptor to the spinal cord.
- Spinal cord: Relays the signal to the brainstem and thalamus.
- Thalamus: A relay station for sensory information, sending the signal to the sensory cortex.
- Sensory cortex: Processes the sensory information received from the thalamus, leading to conscious perception.
Types of Sensory Receptors
- Exteroceptors: Detect stimuli from the external environment, such as touch, temperature, pressure.
- Interoceptors: Detect stimuli from within the body, such as hunger, thirst, and pain.
- Mechanoreceptors: Respond to mechanical stimuli, such as touch, pressure, vibration.
- Chemoreceptors: Detect chemicals, such as taste, smell, and changes in blood oxygen/CO2 levels.
Somatosensory Pathways
- Dorsal Column-Medial Lemniscus System: Transmits information about touch, vibration, and proprioception to the brain.
- Anterolateral System (Spinothalamic Tract): Carries pain and temperature information to the brain.
Dermatomes
- Dermatomes are specific areas of skin innervated by sensory fibers from a single spinal nerve root.
- Each of the 31 pairs of spinal nerves has a corresponding dermatome.
- Dermatomes are clinically significant for localizing nerve damage or spinal cord injuries.
Thalamus
- The thalamus is a key relay station for all sensory information except smell.
- It processes and filters sensory input before sending it to the appropriate areas of the cerebral cortex.
Cerebral Cortex
- The cerebral cortex is the outermost layer of the brain responsible for processing sensory information, including touch, temperature, pain, and proprioception.
- The somatosensory cortex is located in the postcentral gyrus, specifically in Brodmann's areas 3, 2, and 1.
- The somatosensory cortex contains a "homunculus," a map of the body, where different body parts are represented in proportion to their sensitivity.
Neural Plasticity
- Neural plasticity refers to the brain's ability to change and adapt its structure and function in response to experience.
- This plasticity allows for learning, adaptation, and recovery from brain injuries.
Sensory Adaptation and Sensitization
- Sensory adaptation: A decrease in the sensitivity of a sensory receptor over time in response to a constant stimulus.
- Sensitization: An increase in the sensitivity of a sensory receptor to a stimulus.
- Central sensitization refers to sensitization occurring in the central nervous system.
Endogenous Analgesic System
- The body's natural pain-relieving system, which involves the release of endogenous opioids like endorphins.
- Key structures involved in this system include the periaqueductal gray, the raphe magnus nucleus, and a pain-inhibitory complex in the spinal cord.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.