Podcast
Questions and Answers
What is the primary role of red blood cells (erythrocytes)?
What is the primary role of red blood cells (erythrocytes)?
- Transporting oxygen to tissues. (correct)
- Aiding in blood clot formation.
- Participating in inflammatory responses.
- Filtering waste products in the kidneys.
Which hormone primarily stimulates the bone marrow to produce red blood cells?
Which hormone primarily stimulates the bone marrow to produce red blood cells?
- Interleukins
- Gastrin
- Thrombopoietin
- Erythropoietin (correct)
Where does hematopoiesis primarily occur in adults?
Where does hematopoiesis primarily occur in adults?
- Bone marrow (correct)
- Spleen
- Kidneys
- Liver
What dietary components are specifically required for effective hematopoiesis?
What dietary components are specifically required for effective hematopoiesis?
What happens to the majority of erythropoietin when the kidney senses low oxygen in the bloodstream?
What happens to the majority of erythropoietin when the kidney senses low oxygen in the bloodstream?
What is the lifespan of a typical red blood cell (RBC)?
What is the lifespan of a typical red blood cell (RBC)?
Where does the breakdown of red blood cells (hemolysis) primarily occur?
Where does the breakdown of red blood cells (hemolysis) primarily occur?
What component is hemoglobin broken down into during hemolysis?
What component is hemoglobin broken down into during hemolysis?
Jaundice, characterized by yellowing of the skin and eyes, may indicate what condition?
Jaundice, characterized by yellowing of the skin and eyes, may indicate what condition?
Which term defines a condition where red blood cells have a diminished capacity to deliver oxygen to tissues?
Which term defines a condition where red blood cells have a diminished capacity to deliver oxygen to tissues?
What does the term '-cytic' refer to when describing anemia in a microscopic exam of RBCs?
What does the term '-cytic' refer to when describing anemia in a microscopic exam of RBCs?
Which type of anemia is characterized by small and abnormally shaped erythrocytes with decreased hemoglobin concentration?
Which type of anemia is characterized by small and abnormally shaped erythrocytes with decreased hemoglobin concentration?
Which condition is associated with increased destruction of erythrocytes?
Which condition is associated with increased destruction of erythrocytes?
Mutation on which chromosome results in an abnormal type of hemoglobin called 'Hgb S'?
Mutation on which chromosome results in an abnormal type of hemoglobin called 'Hgb S'?
What is a common characteristic of sickled cells that leads to organ ischemia and intense pain?
What is a common characteristic of sickled cells that leads to organ ischemia and intense pain?
Which of the following is a common treatment approach during a sickle cell crisis?
Which of the following is a common treatment approach during a sickle cell crisis?
How can hydroxyurea help manage sickle cell anemia?
How can hydroxyurea help manage sickle cell anemia?
Which genetic disorder results in the abnormal formation of hemoglobin due to missing or variant genes?
Which genetic disorder results in the abnormal formation of hemoglobin due to missing or variant genes?
What therapy can be administered to clients dealing with iron overload as a result of Thalassemia?
What therapy can be administered to clients dealing with iron overload as a result of Thalassemia?
What process is impaired in iron deficiency anemia?
What process is impaired in iron deficiency anemia?
In which part of the small intestine does iron absorption predominately occur?
In which part of the small intestine does iron absorption predominately occur?
What substance impacts iron absorption?
What substance impacts iron absorption?
What is a common side effect of oral iron supplementation?
What is a common side effect of oral iron supplementation?
Where is Vitamin B12 stored over time?
Where is Vitamin B12 stored over time?
What type of anemia is specifically associated with a deficiency in vitamin B12?
What type of anemia is specifically associated with a deficiency in vitamin B12?
What is the underlying cause of pernicious anemia?
What is the underlying cause of pernicious anemia?
What is a common neurological consequence of vitamin B12 deficiency?
What is a common neurological consequence of vitamin B12 deficiency?
What vitamin deficiency during pregnancy can cause neural tube defects in the fetus?
What vitamin deficiency during pregnancy can cause neural tube defects in the fetus?
How is folic acid primarily absorbed in the body?
How is folic acid primarily absorbed in the body?
In which condition do stem cells fail to produce mature blood cells, leading to a deficiency in all three blood cell types?
In which condition do stem cells fail to produce mature blood cells, leading to a deficiency in all three blood cell types?
What term describes a deficiency in all three types of blood cells (red blood cells, white blood cells, and platelets)?
What term describes a deficiency in all three types of blood cells (red blood cells, white blood cells, and platelets)?
What treatment can can be taken for Aplastic Anemia?
What treatment can can be taken for Aplastic Anemia?
What condition is characterized by an increased production of red blood cells (RBCs) in the bone marrow?
What condition is characterized by an increased production of red blood cells (RBCs) in the bone marrow?
What is the mainstay treatment-phlebotomy's goal?
What is the mainstay treatment-phlebotomy's goal?
What should clinicians take careful measures to consider with Folic Acid?
What should clinicians take careful measures to consider with Folic Acid?
Beyond transporting oxygen, what additional function does blood perform related to gas exchange?
Beyond transporting oxygen, what additional function does blood perform related to gas exchange?
What determines the differentiation of pluripotent stem cells into specific types of blood cells?
What determines the differentiation of pluripotent stem cells into specific types of blood cells?
A patient has a condition causing reduced oxygen delivery to their kidneys. How does this directly impact erythropoiesis?
A patient has a condition causing reduced oxygen delivery to their kidneys. How does this directly impact erythropoiesis?
How does the unique biconcave shape of erythrocytes contribute to their function?
How does the unique biconcave shape of erythrocytes contribute to their function?
During hemolysis, what prevents iron from causing toxicity?
During hemolysis, what prevents iron from causing toxicity?
What does an elevated level of unconjugated bilirubin indicate?
What does an elevated level of unconjugated bilirubin indicate?
What is the long-term consequence of untreated anemia in individuals with increased hemolysis?
What is the long-term consequence of untreated anemia in individuals with increased hemolysis?
How does the presence of hemoglobin S (Hgb S) affect erythrocyte morphology and function in sickle cell anemia?
How does the presence of hemoglobin S (Hgb S) affect erythrocyte morphology and function in sickle cell anemia?
What triggers vaso-occlusive crises in sickle cell anemia?
What triggers vaso-occlusive crises in sickle cell anemia?
How does hydroxyurea reduce the frequency of vaso-occlusive crises in sickle cell anemia?
How does hydroxyurea reduce the frequency of vaso-occlusive crises in sickle cell anemia?
Iron overload is a frequent complication of Thalassemia. What causes this?
Iron overload is a frequent complication of Thalassemia. What causes this?
Which factor primarily determines an individual's daily iron requirements?
Which factor primarily determines an individual's daily iron requirements?
What role does Vitamin C play in iron absorption?
What role does Vitamin C play in iron absorption?
What hematological change indicates successful iron replacement?
What hematological change indicates successful iron replacement?
How does the body store Vitamin B12 for future use?
How does the body store Vitamin B12 for future use?
A patient with pernicious anemia is not able to absorb Vitamin B12. What causes this?
A patient with pernicious anemia is not able to absorb Vitamin B12. What causes this?
Why are neurological changes a consequence of Vitamin B12 deficiency?
Why are neurological changes a consequence of Vitamin B12 deficiency?
How is a B12 deficiency primarily corrected?
How is a B12 deficiency primarily corrected?
What is the primary role of folic acid in cellular function?
What is the primary role of folic acid in cellular function?
Why is folic acid supplementation critical during early pregnancy?
Why is folic acid supplementation critical during early pregnancy?
How does folic acid deficiency affect red blood cell production?
How does folic acid deficiency affect red blood cell production?
What is pancytopenia, which is seen in Aplastic Anemia?
What is pancytopenia, which is seen in Aplastic Anemia?
How does polycythemia vera increase the risk of cardiovascular events?
How does polycythemia vera increase the risk of cardiovascular events?
Clinicians should be aware of what relationship between Folic Acid and Vitamin B12?
Clinicians should be aware of what relationship between Folic Acid and Vitamin B12?
What is the primary goal of phlebotomy in treating polycythemia vera?
What is the primary goal of phlebotomy in treating polycythemia vera?
Flashcards
What is blood?
What is blood?
Liquid tissue composed of cells suspended in a watery plasma.
Functions of blood
Functions of blood
Transports oxygen and nutrients, removes carbon dioxide, forms blood clots, carries immune cells, delivers waste to kidneys/liver, and regulates body temperature.
What is plasma?
What is plasma?
The liquid component of blood (55%), made of water, sugar, fat, protein, and salts.
Cellular components of blood
Cellular components of blood
Signup and view all the flashcards
What is hematopoiesis?
What is hematopoiesis?
Signup and view all the flashcards
What are Red blood cells (RBCs)?
What are Red blood cells (RBCs)?
Signup and view all the flashcards
What are White blood cells (WBCs)?
What are White blood cells (WBCs)?
Signup and view all the flashcards
What are Platelets?
What are Platelets?
Signup and view all the flashcards
What is Erythropoiesis?
What is Erythropoiesis?
Signup and view all the flashcards
What is Erythropoietin?
What is Erythropoietin?
Signup and view all the flashcards
What are Erythrocytes?
What are Erythrocytes?
Signup and view all the flashcards
What is Hemoglobin?
What is Hemoglobin?
Signup and view all the flashcards
What is Anemia?
What is Anemia?
Signup and view all the flashcards
What is a Complete Blood Count (CBC)?
What is a Complete Blood Count (CBC)?
Signup and view all the flashcards
What is MCV (Mean Corpuscular Volume)?
What is MCV (Mean Corpuscular Volume)?
Signup and view all the flashcards
What is MCHC (Mean Corpuscular Hemoglobin Concentration)?
What is MCHC (Mean Corpuscular Hemoglobin Concentration)?
Signup and view all the flashcards
Macrocytic-normochromic Anemias
Macrocytic-normochromic Anemias
Signup and view all the flashcards
Microcytic-hypochromic Anemias
Microcytic-hypochromic Anemias
Signup and view all the flashcards
Normocytic-normochromic Anemias
Normocytic-normochromic Anemias
Signup and view all the flashcards
What is Blood Loss Anemia?
What is Blood Loss Anemia?
Signup and view all the flashcards
What is Hemolytic Anemia?
What is Hemolytic Anemia?
Signup and view all the flashcards
What is Sickle Cell Anemia?
What is Sickle Cell Anemia?
Signup and view all the flashcards
What is Thalassemia?
What is Thalassemia?
Signup and view all the flashcards
What is Hydroxyurea?
What is Hydroxyurea?
Signup and view all the flashcards
Metabolic functions of iron(Fe2+)
Metabolic functions of iron(Fe2+)
Signup and view all the flashcards
What is Iron-Deficiency Anemia?
What is Iron-Deficiency Anemia?
Signup and view all the flashcards
Ferrous sulfate
Ferrous sulfate
Signup and view all the flashcards
What is Vitamin B12?
What is Vitamin B12?
Signup and view all the flashcards
What is Pernicious Anemia?
What is Pernicious Anemia?
Signup and view all the flashcards
What is Megaloblastic anemia?
What is Megaloblastic anemia?
Signup and view all the flashcards
Cyanocobalamin
Cyanocobalamin
Signup and view all the flashcards
What is Folic Acid?
What is Folic Acid?
Signup and view all the flashcards
What is Aplastic Anemia?
What is Aplastic Anemia?
Signup and view all the flashcards
What is Polycythemia?
What is Polycythemia?
Signup and view all the flashcards
What s Polycythemia vera?
What s Polycythemia vera?
Signup and view all the flashcards
Study Notes
Module III: Transport - Concepts in Oxygen Transportation
- Blood is a liquid tissue of cells in a watery plasma.
Functions of Blood
- Transports oxygen and nutrients to tissues.
- Transports carbon dioxide for removal through the lungs.
- Forms blood clots, preventing excess blood loss.
- Carries infection-fighting cells and antibodies.
- Delivers waste to kidneys and liver for blood filtering.
- Regulates body temperature.
Blood Components
- Plasma (55%) is the liquid component containing water, sugar, fat, protein, and salts.
- Cellular components (45%) include RBCs, WBCs, and platelets.
- Blood, pumped by the heart, circulates through vessels continuously with a total volume of 4-6 L, which makes up 7-8% of body weight.
Hematopoiesis
- Hematopoiesis is the formation of new blood cells, producing 200 billion cells daily in the bone marrow.
- Requires B vitamins, vitamin C, copper, and iron, among other nutrients.
- Pluripotent stem cells are immature blood cells in bone marrow awaiting a signal for differentiation.
Circulating Cells
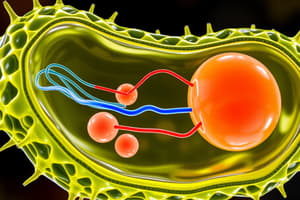
- Red blood cells (RBCs), or erythrocytes, carry oxygen (O2) to tissues and remove carbon dioxide (CO2).
- White blood cells (WBCs), or leukocytes, participate in inflammatory and immune responses.
- Granulocytes such as neutrophils, eosinophils, and basophils are included.
- Lymphocytes and monocytes are another.
- Platelets, or thrombocytes, help with normal blood clotting.
Erythropoiesis
- Erythropoiesis is the process of RBC production, stimulated by erythropoietin.
- The hormone erythropoietin stimulates bone marrow to produce RBCs.
- Ninety percent of erythropoietin is secreted by the kidneys, and 10% comes from the liver.
- The kidney secretes erythropoietin when it senses low oxygen (hypoxia) in the bloodstream.
- Erythropoietin informs stem cells in bone marrow to differentiate into erythrocytes, taking seven days to go from immature stem cells (reticulocytes) until released.
- Amino acids, iron, folic acid, Vitamins B12, B2, B3, and B6 in the diet is needed for erythropoiesis.
Erythrocytes - RBCs
- RBCs are bi-concave round cells without a nucleus.
- Cells are able to change shape easily to fit through small blood vessels.
- Their primary job is oxygen transport via hemoglobin.
- Each RBC carries 200-300 million hemoglobin molecules with each heme group transporting 4 oxygen molecules.
Oxygen Transport
- Hemoglobin in red blood cells combines with oxygen within the capillaries. 98% combines with hemoglobin Hb, 2% dissolves in plasma.
RBC Life Cycle and Hemolysis
- RBC have a 120-day lifespan.
- Hemolysis is the breakdown of RBC in the liver and spleen by macrophages.
- Heme from hemoglobin breaks down into bilirubin and iron.
Hemolysis of RBCs
- Bilirubin from RBC breakdown attaches to plasma molecule, converts to conjugated bilirubin, and transports to liver.
- Conjugated (direct) bilirubin is water soluble and excreted in urine and bile.
- Unconjugated (indirect) bilirubin is plasma insoluble and, if accumulated, leads to jaundice.
- Jaundice can indicate hemolytic anemia (too much for liver to process) or liver dysfunction (slow liver).
Anemia Overview
- Anemia is a condition where RBCs have diminished oxygen delivery capacity to tissues and it has many different types.
- It indicates an underlying disorder as opposed to a distinct illness, where successful treatment depends on proper pathology identification and treatment.
Complete Blood Count (CBC) Parameters
- Complete blood count involves several parameters used to evaluate and define, with normal levels.
- Total red blood cells: Number of RBCs per liter
- Hgb: Amount of Hgb in blood g/dL
- Hct: Packed RBC volume, fraction of the whole blood that consists of RBC
- MCV: Size of the RBC
- MCH: Mass of the RBC
- MCHC: Concentration of Hgb (color)
- RBC distribution width: Measures the variation in RBC size and shape
- Platelets: Cells that assist clotting
- Reticulocytes: Immature RBCs
- MCH and MCHC indicate color of RBCs; low values indicate pale color.
Microscopic Exam of RBCs
- Mean corpuscular volume (MCV) is cell size, with -cytic referring to cell size. Macro is large, micro is small, and normo is normal.
- Mean corpuscular hemoglobin concentration (MCHC) is the hemoglobin concentration and its color, so -chromic refers to color. Hypo is decreased and pale while normo is normal.
Classification of Anemia
- Macrocytic-normochromic anemia features large, abnormally shaped erythrocytes with normal hemoglobin concentration. Pernicious anemia and folate-deficiency anemia are examples.
- Microcytic-hypochromic anemia has small, abnormally shaped erythrocytes with decreased hemoglobin concentration. Iron-deficiency anemia or thalassemia are examples.
- Normocytic-normochromic anemia features destruction or depletion of normal erythroblasts or mature erythrocytes. Aplastic anemia, hemorrhagic anemia, sickle-cell anemia, and hemolytic anemia are included.
Types of Anemia
- There are three main types: blood loss, increased erythrocyte destruction (hemolysis), and decreased erythrocyte production.
- Blood loss can be acute or chronic.
- Increased erythrocyte destruction (hemolysis), caused by Sickle Cell and Thalassemias.
- Decreased erythrocyte production, caused by iron, Vitamin B12, and folic acid deficiency plus aplastic anemia.
Blood Loss Anemia
- Acute blood loss can be caused by trauma.
- Chronic blood loss from menstruation, peptic ulcer disease, or colon cancer may be asymptomatic.
- Hypoxia from blood loss will stimulate bone marrow to produce red blood cells; concentrations take 3-4 weeks to return to normal.
- Treatment includes treating the underlying issue along with transfusions when needed.
Increased Destruction of Erythrocytes (Hemolytic Anemias)
- Hemolytic anemias lead to red blood cells being destroyed faster than being made.
Sickle Cell Disease
- Sickle cell trait is a condition where someone has one abnormal gene and one normal gene.
- Sickle cell disease is autosomal recessive, meaning it is inherited and there are 2 copies of the mutated genes
- Chromosome 11 mutation results in abnormal hemoglobin called "Hgb S."
Sickle Cell Anemia
- Hbg S causes RBCs to become elongated and sickle-shaped, where rigidity and flexibility are decreased.
- Sickled cells cannot carry oxygen adequately and "clog" up capillaries, leading to organ ischemia and intense pain (vaso-occlusive crisis).
Sickle Cell vs. Normal RBC Lifespan and Parameters
- Normal RBCs have a 120-day lifespan with normal oxygen-carrying capacity, 12-14 g of Hbg per ml, and are normally destroyed.
- Sickled cells have a 10-40-day lifespan with decreased oxygen-carrying capacity, 6-9 g of Hbg per ml, and RBCs are destroyed at an accelerated rate.
- Precipitating factors for crisis include fever, stress, dehydration, trauma, acidosis, and hypoxia.
Sickle Cell Anemia Characteristics
- The RBC lifespan is only 10-40 days with increased destruction by the spleen and leading to anemia.
- Over time, crises produce progressive organ damage and the decrease in average lifespan.
- Manifestations generally first appear around 6 months of age.
- The three drivers causing the crisis are vaso-occlusion, hemolysis, and anemia, which can all result in organ damage.
Complications/Effects of Sickle Cell Disease
- The complications include recurrent infections, anemia, pain, jaundice, organ damage, heart failure, and stroke.
Sickle Cell Anemia Treatment
- Acute treatment focuses on hydration, oxygenation, and pain management using hydromorphone and morphine.
- Long term treatment involves avoiding precipitating factors through hydration and up-to-date vaccinations.
- Physical exams every 3-6 months and annual eye exams, plus medications like Hydroxyurea, blood transfusions, bone marrow transplants, and gene therapy contribute to treatment.
Hydroxyurea
- Hydroxyurea is an antineoplastic agent that increases the amount of fetal hemoglobin (Hb F).
- Improves oxygenation and decreases the sickling of RBCs and alters the adhesion of RBC to the endothelium.
- It causes bone marrow suppression (neutropenia, anemia, low platelets) as an adverse effect, plus oral ulcers, rash, and nail changes, and hyperpigmentation.
- Clinical considerations for oral administration: do not use during pregnancy/breastfeeding; a clinical response takes 3-6 months. Additionally, it reduces mortality, hospitalization, reduces vaso-occlusive episodes by 50%, and blood counts (CBC) should be monitored every 2 weeks during initiation. Supplement with folic acid.
Sickell Cell Anemia: Gene Therapy to cure
- First extract stem cells from patient's bone marrow.
- Infuse them with normal gene for hemoglobin.
- Condition patient's bone marrow to recieve new stem cell, then insert it.
Thalassemia
- Thalassemia is an autosomal recessive genetic disorder resulting in abnormal formation of hemoglobin due to missing or variant genes that code for it.
Thalassemia Manifestations
- Manifestations include iron overload from transfusions or hemolysis, which can damage the heart, liver, kidneys, and pancreas.
- Bone deformities from bone marrow expansion which especially occurs in the face and skull, causing increasing break chances.
- Enlarged spleen and liver cause a protuberant abdomen (splenectomy = infection).
- Slowed growth rates and jaundice also present.
Thalassemia Treatment
- Blood transfusions are administered because the body cannot make the right hemoglobin.
- Chelation therapy exists as a treatment for iron overload using deferasirox.
- Folic acid supplementation, bone marrow transplant can aid in normal RBC synthesis.
Decreased Production of Erythrocytes
- Type of anemia.
Iron (Fe2+)
- Iron has metabolic functions as a mineral, essential to the function of several mitochondrial enzymes involved in metabolism and energy production. Also, 60-80% of iron in the body is associated with hemoglobin inside RBCs.
- Regulation occurs through intestinal absorption, where only 10% of iron in the diet is absorbed.
- Calcium decreases iron absorption and vitamin C will increase it.
- Elimination is minimal and recycling is a conservation process.
Iron (Fe2+) Overview
- Free iron is toxic, so the body binds the mineral to protein complexes.
- Ferritin and hemosiderin maintain iron stores inside the cells. Transferrin transports iron to sites in the body where it is needed.
- Bone marrow for hemoglobin, the liver for storage as ferritin, and muscle and tissues for myoglobin and iron-containing enzymes all use up needed iron.
Daily Requirements of Iron
- The requirements depend on the rate of RBC production, where there is more need for females than males.
- Increased need during pregnancy.
- Dietary sources vary.
- 14-18: 11mg men & 15mg women
- 18-50: 8-9mg men & 15-18mg women
- 50+: 8-9mg
- Pregnancy: 15-27mg
Iron-Deficiency Anemia
- Imbalances can occur between iron uptake and demand, along with inadequate iron to synthesize hemoglobin.
- Etiologies include decreased iron intake from poor diet, infants/children consuming cows' milk, and vegetarianism.
- Blood loss from women menstruation and chronic GI loss, or decreased iron absorption are causes. (decreased stomach acid = GI diosrders)
Iron Deficiency Anemia Studies
- Complete Blood Count reveals a low hemoglobin/hematocrit, MCV (microcytic), and MCHC (hypochromic).
- Iron Studies reveal low serum Fe, low serum Ferritin, higher serum transferrin, and high TIBC.
Iron-Deficiency Anemia Manifestations
- Manifestations may be asymptomatic until Hgb values are less than 7-8 g/dl.
- Pallor, weakness, and fatigue, dyspnea, palpitations, and tachycardia, along with Pica are all manifestations.
- Late manifestations include glossitis (red, sore tongue), angular stomatitis (dry, sore corners of the mouth), and brittle, concave (spoon-shaped) nails.
Ferrous Sulfate
- Supplies body with iron to be absorbed and used for bodily processes.
- GI disturbances (70%) such as constipation, nausea, abdominal pain, and flatulence, darkening of stools, and staining of teeth can occur.
- Oral administration (20% elemental) in tablets, elixir, or solution form, but avoids enteric coating (EC) and sustained release for decreased absorption.
Ferrous Sulfate: Clinical Considerations
-
Increase dietary iron in the diet such as liver, egg yolks, muscle meats, yeast, grains, and green leafy vegetables. Administration:
- Don't give within 1 hour of bedtime; best on empty stomach, but given with a small snack, can help with GI discomfort.
- Dosed every other day.
- Ascorbic acid increases absorption.
-
May need to take for 3 to 5 months to fully restore iron reserves. It is also important to monitor efficacy and iron stores
- CBC to look for increased reticulocyte count in one week and hemoglobin of 2 g/dL in one month.
-
Side effects are more energy and that fatigue and pallor should subside. (Iron is toxic in overdose.)
Advantages and Disadvantages of Iron Supplements
-
Oral iron can be in the form of ferrous sulfate, ferrous gluconate, and ferrous fumarate- it is effective for most patients. Low risk of serious adverse events. Gi side effects are common, compliance may be low.
-
Iv iron can be Iron sucrose, Iron dextran, and Ferumoxytol, and it. effective the gi side effects are no compliance, and less gi side effects. But Requires monitored IV infusion Nurses must watch vitals Rare cases of allergic or infusion related reactions Require equipment and personnel for administration
Vitamin B12
- Vitamin B12 functions for two coenzymes used for cell growth and DNA replication.
- Absorption process:
- Binds with intrinsic factor (secreted by parietal cells of the stomach).
- B12 plus intrinsic factor can be absorbed by intestinal wall.
- After absorption, dissociation occurs allowing free B12 to bind with transcobalamin II for storage in the liver and immediate use for growth. And occurs slowly over time.
Vitamin B12 Deficiency
- Daily requirements: 2.4 mcg/day from meat and dairy products, and absorption of Vitamin B12 requires Intrinsic Factor (IF)- deficiencies causes pernicious anemia.
- Etiologies include an inadequate amount of animal products in diet, chronic gastritis an autoimmune/gastrectomy. 10-30% age over age of 50s have inablutya b12 absorption.
- Requires diagnostic Measurement of plasma B12, and Complete blood count (CBC).
Vitamin B12 Deficiency Consequences
- Megaloblastic anemia results, where DNA synthesis is impaired and growing cells cannot divide with oversized cells because the cell cannot mature.
- Neurological changes result from decreased myelin along with tingling, numbness of feet/hands.
- Elevated homocysteine levels and Peripheral and cerebral hypoxia, along with mental changes or psychosis.Also causes GI and mouth ulcerations.
Cyanocobalamin
- Cyanocobalamin is a supplement with a coenzyme for various metabolic functions, used in cell replication and hematopoiesis.
- Oral, sublingual, intranasal, subcutaneous, or intramuscular administration; mild-moderate deficiency: oral route vs severe deficiency, malabsorption, or pernicious anemia: IM injection or sublingual. Follow the correct severity, dosage, and monitor.
Vitamin B12 Deficiency (Summary)
- Etiology is Vitamin B12 deficiency in diet (lack of meat and/or dairy), pernicious anemia, and gastric bypass.
- Primary hematologic effect results because of Megaloblastic anemia
- Neurologic effect results in Demyelination of neurons.
- Can be diagnosed CBC or through plasma tests.
- Treat with Cyanocobalamin with usual time of therapy of lifelong.
Folic Acid Deficiency Overview
- Vitamin B9
- For two coenzymes for cell growth and DNA.
- absorbed in small intestine.
- eliminated through urine
- If intake of folic acid were to cease, signs of deficit would develop rapidly
Folic Acid Requirements + Sources
- 200 mcg/day males
- 180 mcg/day for females.
- 400-800 if pregnant from greens, liver, and yeast.
Folic Acid Deficiency manifestation
- Causes anemia
- Looks like b12 def
- can use neural tube deffects
Folic Acid Treatment
- It is necessary for formation of several coenzymes with adverse effects.
- Give higher doses.
- Urine may turn a yellow color.
- Mask an irreversible nuerologic dmg.
- Ret count and so on can fix it as well
Etiolgies and Treatment
- Causes a lot. The the treat is usually cya
- But can be overcomed with folic acid
- Can be short of long term by any means
Aplastic Anemia Overview
- Anemia causing mature cells to no longer reproduce through stem cells
- Causes pancytopenia, aka Deficiency in all three types of cells
- Can cause problems within all bc ranges
Aplastic Anemia Main
- Hereditary
- Chemical exposure
- Immune
- Treatment includes replace and blood transfusion
Polycythemia
- Opposite of anemia
- Increased production of RBC
- Also increased homolobin
- Very and second degree
Polycythemia Vera
- a hyper proliferation
- Makes the blood thick
- Can make blood clot
- Treatment includes phlebohtomy
- Also aspirin hydro and bone marrow transplantant
Clinical Pearls
- All blood cells originate from stems cells in the bone marrow.
- Erythropoiesis requires vitamins from the diet.
- Patients with elevated bilirubin may present with jaundice. This may be a sign of increased red cell destruction (hemolysis).
- A CBC can help direct diagnosis of anemia types.
- Iron deficiency anemia is most common type. Always know how to counsel patients taking ferrous sulfate.
- Use IM cyanocobalamin if patient has pernicious anemia.
- BE CAREFUL! Folic acid can obscure neurologic symptoms of B12 deficiency and can lead to permanent damage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.